Chapter 15 Pediatric Eye Diseases
Introduction
Because of its lack of invasiveness and its painless nature, ultrasonography, especially B-scan, has taken on a very important role in the evaluation of a number of ocular disorders of children. This is especially true for peripheral retinal lesions for which scleral depression or contact lens examination is impossible without anesthesia. Furthermore, a number of causes of a white pupillary reflex in children (leukocoria) can be differentiated on the basis of ophthalmoscopy with additional information from ultrasonography. Ultrasonography also provides important information on orbital tumors and correlates with histopathological features.1
Technique
Individuals performing ultrasound examinations on children quickly learn that a combination of gentleness and playful firmness are essential to obtaining the child’s cooperation and achieving the desired goal of a reliable examination. B-scans are generally performed through the closed eyelids in children (Chapter 3). This does not result in a significant loss of quality or information for the conditions the test is utilized for. A-scans or ultrasound biomicroscopy on the other hand can only be performed by corneal contact or using a water immersion adaptor. They require excellent cooperation, otherwise they can be done under anesthesia (Chapter 4). A-scans are most commonly done in preparation for cataract surgery, or less frequently to determine axial length for the diagnosis of microphthalmia or nanophthalmos.
Clinical conditions
Orbit
Hemangiomas and lymphangiomas
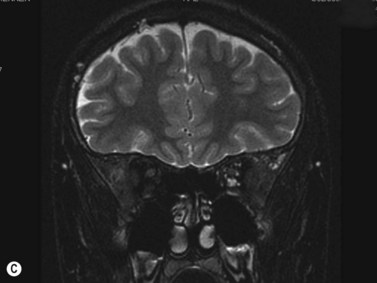
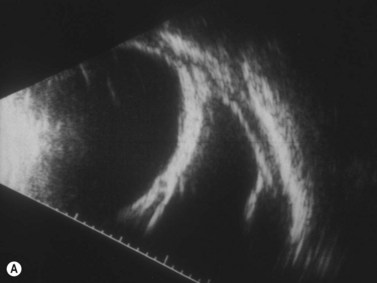
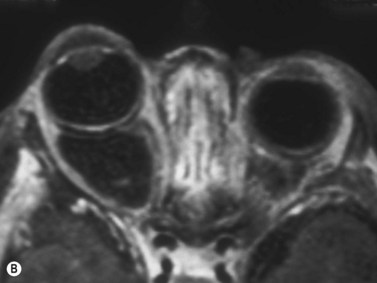
Hemangiomas are the most common orbital tumors in children. Lymphangiomas are less common. Hemangiomas are composed of vascular channels with a proliferation of capillary vascular endothelial cells; some have a cavernous component with larger venous spaces. Hemangiomas generally run a course of increase in size in the first year of life, followed by a regression over a few years. Lymphangiomas tend to remain stationary with episodic exacerbation secondary to hemorrhage or inflammation. These tumors do not invade structures but grow around them and push them. The orbit may be enlarged. While MRI is generally obtained in all cases, B-scan is helpful in the diagnosis as it shows a specific pattern of vascular spaces (Figure 15.1).2
Orbital cysts
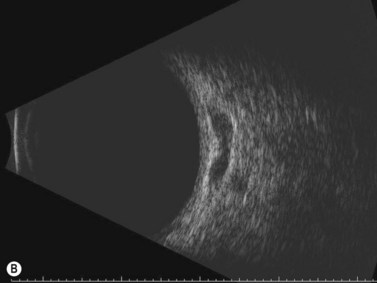
Cystic lesions of the orbit in children include microphthalmia with cyst, congenital cystic eye, and cysts associated with teratomas. Extension of encephaloceles into the orbit can also mimic a primary orbital cystic lesion. The associated clinical findings give away the diagnosis. In microphthalmia with cyst, the eye is reduced in size and may have a coloboma (Figure 15.2). The eye itself may be very small and the cyst may constitute the main orbital content. In such cases there usually is a bulge in the lower lid with small eye pushed superiorly. Congenital cystic eye is extremely rare;3 There is no lens and the globe is replaced by a large cyst. Teratomas are present at birth and are composed of a variety of tissues derived from two or more of the three embryonic layers.4 The tumor can be small and retrobulbar or may be extremely large and push the eye forward while enlarging the orbit significantly. Such birth defects can be detected during prenatal ophthalmic ultrasonography (Chapter 14).
Rhabdomyosarcoma
Rhabdomyosarcomas are rapidly enlarging orbital tumors of striated muscle origin that can be fatal if not diagnosed and treated early.5 Patients present with proptosis, eyelid swelling or ptosis. Several histopathological varieties exist including: alveolar, embryonal and mixed. Treatment consists of total excision followed by a combination of chemotherapy and radiotherapy. Survival is excellent in cases where the diagnosis is made promptly after the onset of signs and symptoms. Mortality was 3% in one series of 33 patients.6 MRI remains the main imaging modality.
Anterior segment
Peters’ anomaly
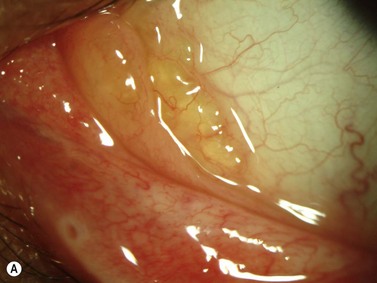
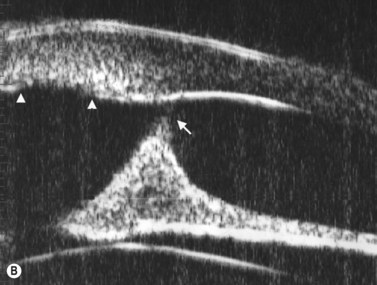
In this heterogeneous group of malformations, there is a central corneal opacity with variable degree of iridolenticulocorneal adhesions. The abnormality results from failure of separation of the lens vesicle from the posterior aspect of the cornea. A central defect in the corneal endothelium and Descemet’s membrane is pathognomonic (Figure 15.3). Two-thirds of cases are bilateral. A cataract may be present and posterior pole malformations such as persistent hyperplastic primary vitreous (PHPV) and colobomas of the disk and retina are common. Ultrasound biomicroscopy and B-scan are helpful in determining the extent of anterior segment involvement, especially in cases where corneal opacification is severe.7