Stage
Radiographic findings
Initial (increased density stage)
Increased density of femoral head, with or without subchondral fracture; radiolucencies appear in the metaphysis
Fragmentation stage
Varying pattern of lucency appear in epiphysis; the femoral head may be flattened and widen; metaphyseal changes resolve
Reossification stage
New bone appears in femoral head which gradually reossifies
Residual (healed) stage
Femoral head is fully reossified and remodels to maturity
Table 33.2
Lateral pillar classification system
Group | Lateral pillar radiographic findingsa |
|---|---|
A | No density change |
No loss of height | |
B | Some density changes |
Height ≥ 50 % | |
Central pillar collapse | |
B/C | Thin lateral pillar |
Borderline height | |
C | Height < 50 % |
33.3.1.2 MRI
MRI is useful in cases of suspected LCP when radiographs are unrevealing, because it is highly sensitive for the detection of early ischemia. Signal intensity alterations of the femoral head that indicate marrow edema are early signs of LCP. MRI can demonstrate the presence and extent of infarction of the femoral head and enhancement of lateral column of the femoral head, suggesting recanalization that is associated with good prognosis (Fig. 33.10). Transphyseal enhancement or transphyseal bone bridging on MR images has been considered as one of the bad prognostic factors. Extension of physeal cartilage into the metaphysis reflects the same process responsible for the radiographic findings of metaphyseal radiolucencies (Fig. 33.11) (Sebag et al. 1997; Song et al. 2000; Dwek 2009; Jaramillo 2009; de Sanctis 2011).
33.3.2 Slipped Capital Femoral Epiphysis
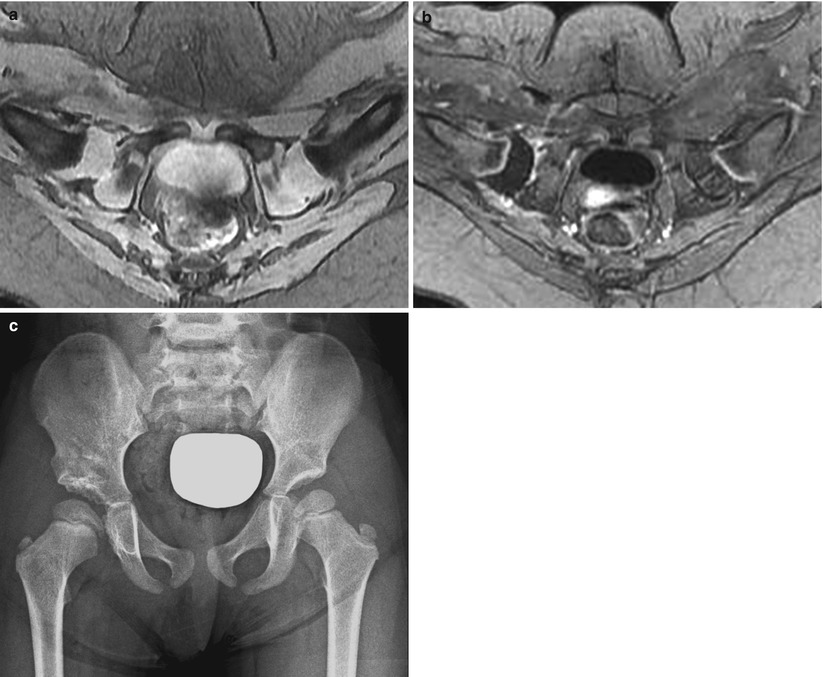
Slipped capital femoral epiphysis (SCFE) is defined as the displacement of the femoral head relative to the femoral neck and shaft. SCFE is more common in boys than in girls (2.5:1), and affected children are frequently obese. In approximately one-third of patients, there is bilateral (but not typically simultaneous or symmetric) involvement of the hips. SCFE is most commonly idiopathic; however, it also has been noted in conjunction with renal osteodystrophy and endocrinopathies, including hypothyroidism and hypopituitarism. There is a history of trauma in approximately 50 % of patients. The earliest radiographic sign is widening and irregularity of the physis with rarefaction in its juxtaepiphyseal portion. In the normal hip, a line drawn tangential to the superior femoral neck (Klein line) on the AP view intersects a small portion of the lateral capital epiphysis; while typical posterior displacement of the capital epiphysis has occurred, this line does not intersect the capital femoral epiphysis. With chronic slip, sclerosis may be seen in the medial femoral neck with bone remodeling (buttressing) (Fig. 33.12). CT and MR may also be used to make the diagnosis of SCFE. Diffuse or globular physeal widening is the earliest evidence of SCFE on MRI (Fig. 33.13). Due to complete loss of osseous continuity, SCFE is associated with high incidence of avascular necrosis as a complication (Fig. 33.14) (Dwek 2009; Tins et al. 2009; Jarrett et al. 2013).
33.3.3 Septic Arthritis
Early diagnosis of septic arthritis is crucial because any delay in the initiation of appropriate treatment can result in a poor outcome such as destruction of the femoral head, degenerative arthritis, or permanent deformity. The most common diagnostic dilemma is that septic arthritis cannot be confidently differentiated from transient synovitis, the most common disease entity in pediatric patients with an irritable hip, on the basis of clinical, laboratory, and radiographic findings (Lee et al. 1999).
Although US is highly accurate in the detection of hip effusion, differentiation of septic arthritis from transient synovitis or other arthritides cannot be achieved with US. Therefore, joint fluid aspiration is essential for early diagnosis of septic arthritis (Fig. 33.15) (Zawin et al. 1993; Robben et al. 1999).
MRI may play an important role in noninvasive differentiation of septic arthritis from transient synovitis in the pediatric patient with an irritable hip. Signal intensity alterations in the bone marrow of the affected hip joint and contrast enhancement of the soft tissues are useful in the differentiation of septic arthritis from transient synovitis. In transient synovitis, contralateral (asymptomatic) joint effusions are more common than septic arthritis, and bone marrow signal intensity alteration is usually absent in transient synovitis (Fig. 33.16) (Lee et al. 1999; Dowen et al. 2006; Yang et al. 2006; Kwack et al. 2007).
33.3.4 Juvenile Idiopathic Arthritis
Juvenile idiopathic arthritis (JIA) is a heterogeneous group of disorders. JIA is defined as a chronic arthritis that persists for a minimum of six consecutive weeks in one or more joints, commencing before the age of 16 years and after active exclusion of other causes. Hip involvement is frequent and is associated with significant morbidity and functional problem.
Contrast-enhanced MRI is the most sensitive imaging modality available to determine whether arthritis is present, but it rarely helps in establishing a specific diagnosis. MRI can be helpful, however, in clarifying the differential diagnosis such as pelvic osteomyelitis or para-articular osteoid osteoma. MRI also can reveal hemosiderin deposition and hemarthrosis suggestive of bleeding disorders, pigmented villonodular synovitis, and synovial vascular malformation. The synovial intima lacks a tight junction or basement membrane and thus allows rapid diffusion of gadolinium compounds into the joint fluid. Therefore, images must be obtained immediately after intravenous injection of contrast materials to display only synovial enhancement caused by active pannus (Argyropoulou et al. 2002; Malattia et al. 2010).
33.3.5 Idiopathic Chondrolysis
Idiopathic chondrolysis of the hip is an uncommon pediatric disorder that occurs during adolescence. It is characterized by pain and limp, with a rapid loss of articular cartilage of the femoral head and acetabulum, resulting in narrowing of the joint space and progressive stiffness in the joint. Conventional radiographic hallmarks include a concentrically narrowed joint space <3 mm without the osteophyte formation typical of osteoarthritis, accompanied by osteopenia. Other findings include protrusio acetabuli, subchondral cysts, widening of the femoral head and neck, and premature physeal closure. A geographic pattern of bone marrow edema centered within the proximal femoral epiphysis accompanied by ipsilateral ill-defined adjacent acetabular bone marrow edema, mild synovial hypertrophy, and little or no joint fluid is a characteristic early MRI finding of idiopathic chondrolysis (Fig. 33.17) (Rowe and Ho 1996; Johnson et al. 2003; Laor and Crawford 2009).
33.3.6 Osteoid Osteoma
Intra-articular osteoid osteoma, which occurs within or near a joint, is considered a separate clinical entity. The most commonly involved joint is the hip. Intra-articular osteoid osteoma is rare, and its clinical manifestations may be puzzling. Imaging findings of intra-articular osteoid osteoma differ from those of intracortical osteoid osteoma. With intra-articular osteoid osteoma, reactive cortical thickening is minimal or absent, a finding believed to be due to a lack of cambium, the inner layer of the periosteum. At CT, the nidus is well defined and round or oval with low attenuation. An area of high attenuation may be seen centrally, a finding that represents mineralized osteoid (Fig. 33.18) (Ebrahim et al. 2001; Gaeta et al. 2004; Szendroi et al. 2004).
33.4 Illustrations: Pediatric Hip Disorders
33.4.1 Proximal Femoral Focal Deficiency
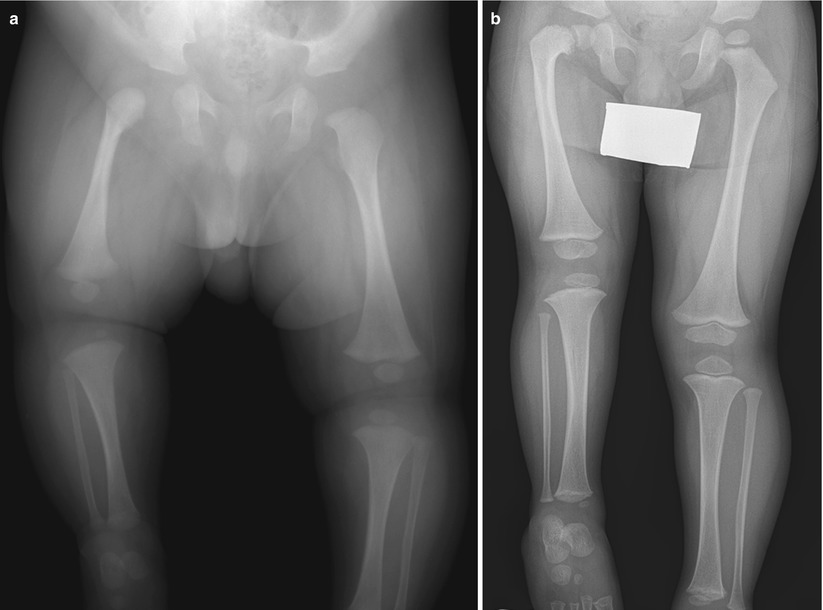
Fig. 33.1
Proximal femoral focal deficiency. (a) Anteroposterior radiograph of a 4-month-old infant with a short right femur shows hypoplastic right femur. Right acetabulum is relatively normal. (b) Follow-up radiograph obtained 3 years later shows a short right femur with coxa vara deformity. Note the hypoplastic right proximal femoral epiphysis and flattened right proximal tibia epiphysis
33.4.2 Developmental Coxa Vara
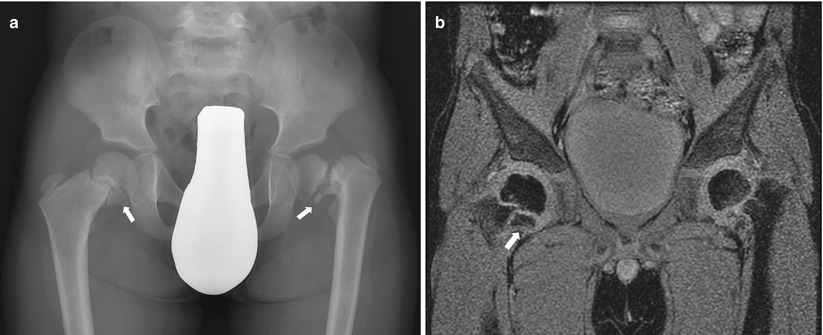
Fig. 33.2
Bilateral coxa vara. (a) Proximal femoral growth plates are vertically tilted. Slight fragmentation (arrows) is seen at the medial aspect of each proximal femoral growth plate. Note the wide left proximal femoral growth plate. (b) Coronal GRE image shows vertically tilted proximal femoral growth plate and bony fragment at medial aspect of the proximal femoral metaphysis (arrow)
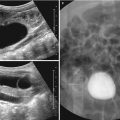
33.4.3 Hip Ultrasonography: Coronal View
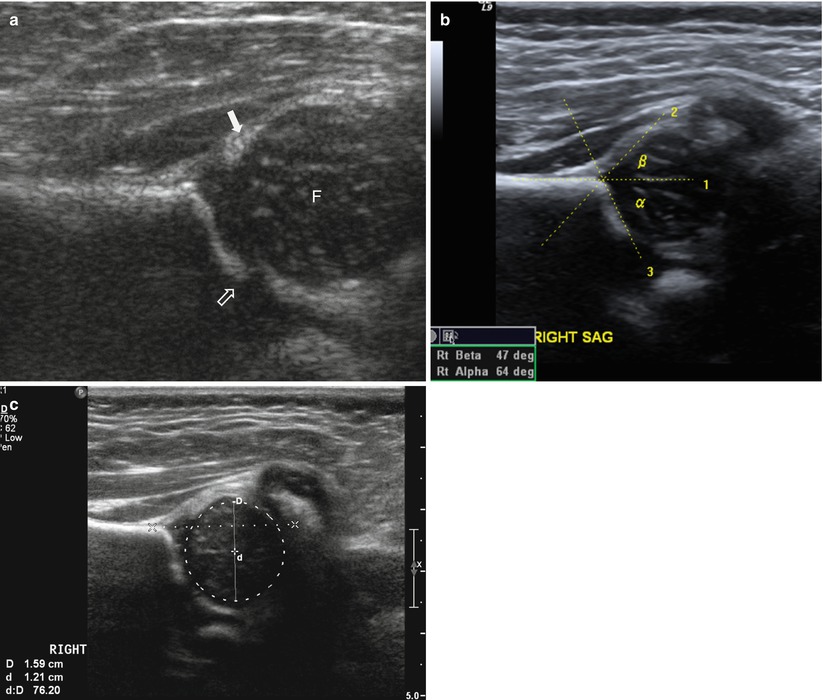
Fig. 33.3
Normal hip ultrasonography: coronal view. (a) Coronal view of hip joint in the standard plane shows low echoic femoral head (F) resting against the bony acetabulum. Note the fibrocartilaginous tip of labrum (arrow) and junction of bony ilium and triradiate cartilage (open arrow). (b) Normal hip ultrasonogram with alpha and beta angles used in measurement. Alpha angles above 60° are normal. (c) Normal hip ultrasonogram with femoral head coverage index measurement. Coronal view of ultrasound demonstrates use of manufacturer processing to draw a horizontal line along the iliac bone and then outline the cartilaginous femoral head to measure percent coverage of the femoral head. Better than 50 % coverage is normal
33.4.4 Hip Ultrasonography: Transverse View
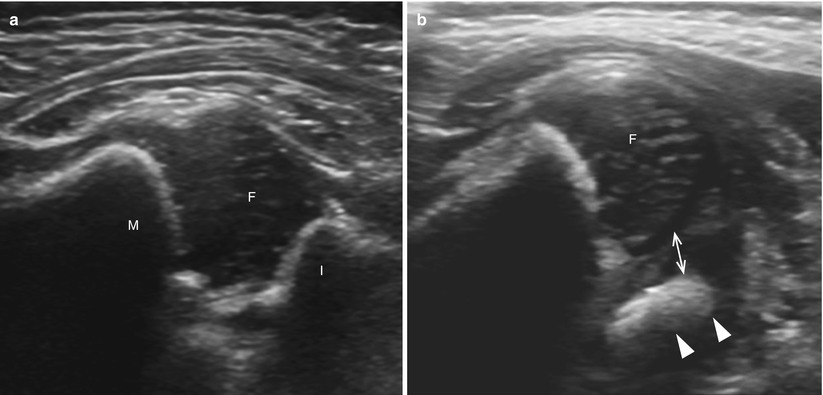
Fig. 33.4
Transverse view of the hip ultrasonography. (a) Normal transverse sonogram of the hip with the 90° hip joint flexion shows low echoic femoral head (F) between metaphysis (M) and ischium (I). (b) Instability of the hip in a newborn baby. With instability and displacement, the femoral head moves laterally and posteriorly. The laterally displaced femoral head (F) has no contact with the ischium (arrowheads) with the widening of space between femoral head and ischium (arrows)
33.4.5 Developmental Dysplasia of the Hip: Ultrasonographic Findings
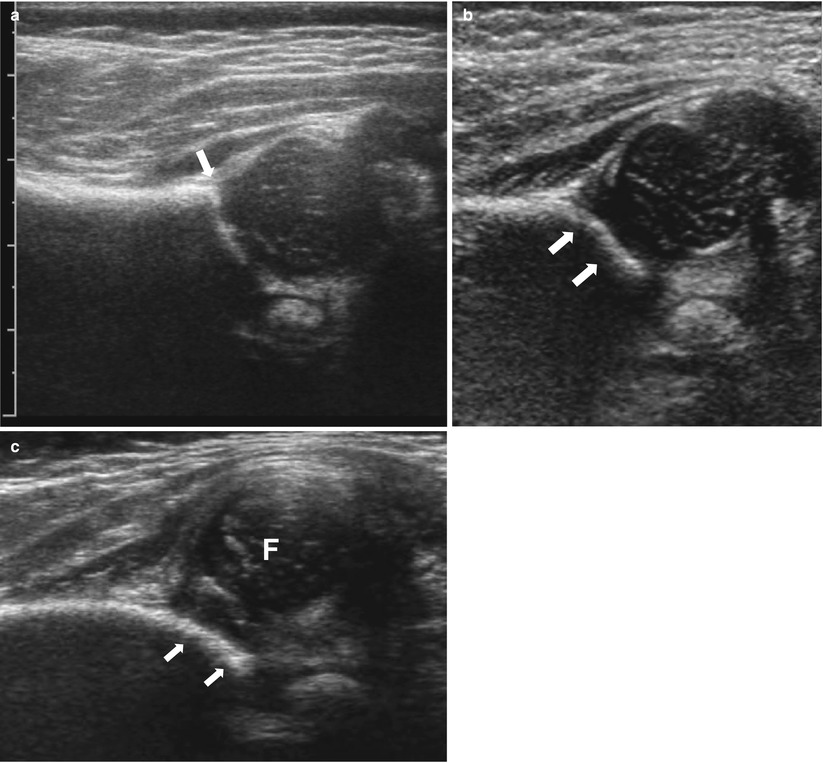
Fig. 33.5
Ultrasonographic spectrum of developmental dysplasia of the hip. (a) Normal hip. The superior acetabular rim is angular (arrow). (b) Lateral edge of the bony acetabulum shows rounded appearance (arrows) suggesting bony acetabular dysplasia. (c) Coronal view of ultrasound shows complete superior and lateral dislocation of the left femoral head from the shallow acetabulum (arrow)
33.4.6 Developmental Dysplasia of the Hip: Radiographic Findings
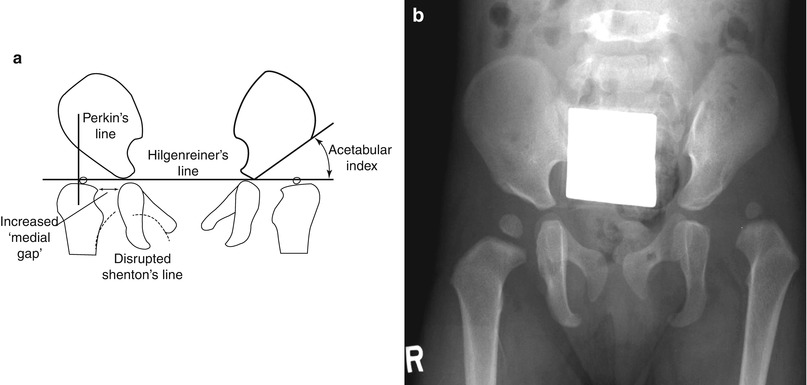
Fig. 33.6
Radiographic findings of developmental dysplasia of the hip. (a) Radiographic measurement used in evaluating developmental dysplasia of the hip. Hilgenreiner’s line is drawn through the triradiate cartilage. Perkin’s line is drawn perpendicular to Hilgenreiner’s line at the margin of the bony acetabulum. Shenton line curves along the femoral metaphysis and connects smoothly to the inner margin of the pubis. Medial gap is measured to quantify proximal and lateral displacement of the hip. The acetabular index is the angle between the lines drawn along the margin of the acetabulum. (b) Anteroposterior radiograph shows relatively small left femoral head ossification center, slightly steep left acetabular roof, and rounded left superior acetabular rim compared to the normal right side
33.4.7 Developmental Dysplasia of the Hip: Postoperative Imaging Findings