Figure 5.1
Goitrous thyroid in congenital hypothyroidism . Axial CT images (a–c) show a massively enlarged thyroid (arrows) in a 5-month-old with a TSH over 300. Full ultrasonic visualization of the thyroid gland is difficult in young children because of the overall short length of their necks compared to the size of most high-frequency transducers and because of the relatively high positioning of the thyroid gland in the neck compared to adults. This is best appreciated on sagittal CT images from the same patient, which well demonstrates the patient’s short neck and how the path of least resistance for the thyroid to enlarge is posterior (arrows, d). On a 3D CT reconstruction (e), note how the thyroid gland (arrow) wraps around the airway (asterisk)
Thyroid Aplasia
Thyroid aplasia presents with CH and an absence of any thyroidal tissue. The defect is usually sporadic, but there are some familial forms, and both autosomal dominant and autosomal recessive inheritance patterns have been reported. Neck ultrasound fails to reveal any thyroid tissue in the thyroid bed, and no uptake is seen with I-123 scintigraphy.
Thyroid Hypoplasia
Ultrasound in children with CH may sometimes demonstrate a small but otherwise normal-appearing thyroid gland (Fig. 5.2). This is particularly common in those children who have CH and trisomy 21 (children with trisomy 21 are also more likely to have small benign thyroid cysts) (Fig. 5.3). There are published charts of normal thyroid volumes for different populations, and these should be used to evaluate the size of the thyroid in children with hypothyroidism, congenital, or otherwise.
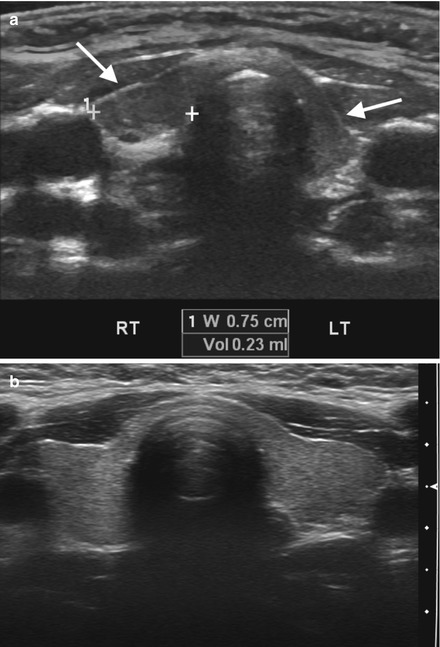
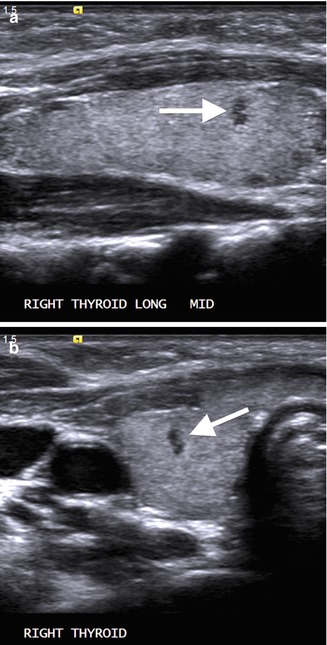
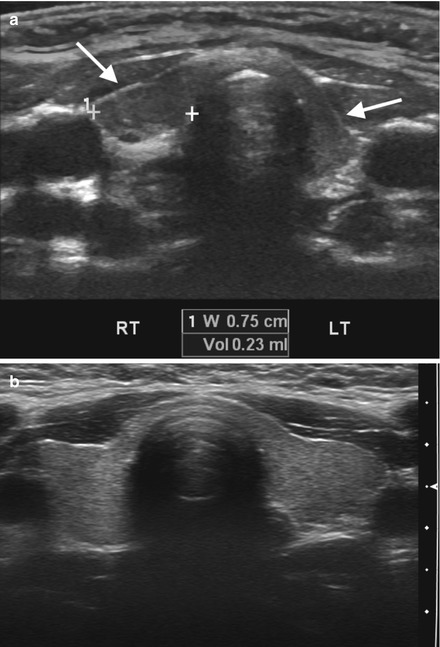
Figure 5.2
Thyroid hypoplasia . In thyroid hypoplasia (a), the gland is small and difficult to visualize; the right and left lobes may both be small (arrows; left lobe measured), and the isthmus may be relatively normal thickness, as shown in a patient with congenital hypothyroidism and trisomy 21. Compare this to the thyroid of a normal child (b), which is well-defined, normal volume, and well-proportioned
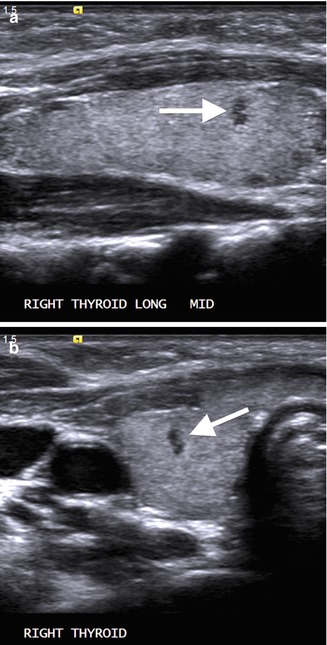
Figure 5.3
Benign thyroid cyst in trisomy 21 . Longitudinal (a) and transverse (b) ultrasound images in a 26-month-old boy with trisomy 21 show the typical appearance of a very small hypoechoic cyst (arrows) seen in patients with Down syndrome. Note lack of significant posterior acoustic enhancement because these cysts are so small
Thyroid Hemiagenesis
Thyroid hemiagenesis is a rare congenital anomaly in which one lobe of the thyroid fails to form. It is the most innocuous form of thyroid dysgenesis and is much more common in girls. In hemiagenesis it is almost always the left lobe that is absent; the right lobe has a normal size and appearance, and, although blunted, the isthmus is usually present (Fig. 5.4). For unknown reasons, the isthmus will be absent in rare cases of right hemiagenesis (Fig. 5.5). Although hemiagenesis is considered an incidental finding, numerous studies have shown that these patients have a slightly increased rate of all forms of thyroid pathology, from hyperthyroidism to carcinoma. The diagnosis of thyroid hemiagenesis should be clearly communicated to the surgeon in patients who are to undergo any type of neck surgery.

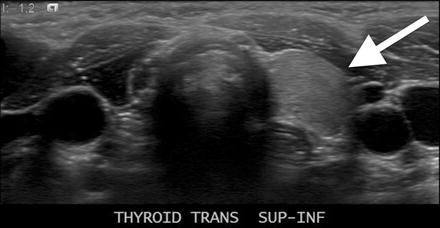

Figure 5.4
Left thyroid hemiagenesis . Axial CT image in a 26-month-old with a retropharyngeal abscess shows absence of the left lobe of the thyroid gland. The right lobe is shown with an arrow, and the right jugular vein (J) and carotid artery (c) are also annotated. Although not present in this child, patients with an absent left thyroid lobe usually have a small but blunted isthmus
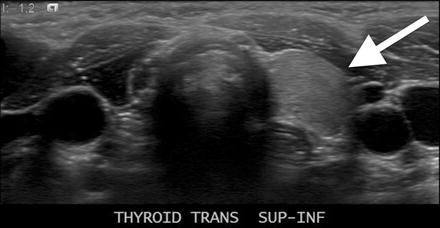
Figure 5.5
Right thyroid hemiagenesis . A transverse image of the thyroid reveals a normal left lobe (arrow) but no right lobe or isthmus. Right thyroid hemiagenesis is quite rare
Ectopic Thyroid
Ectopic, or aberrant, thyroid tissue can be found anywhere along the normal path of thyroid descent but is most commonly found at the base of the tongue, in which case it may be referred to as a lingual thyroid (Fig. 5.6). Ultrasound of the thyroid bed may reveal a hypoplastic thyroid or no thyroid tissue at all. Further imaging workup varies according to local preferences and practice; although I-123 scintigraphy is very sensitive for the presence of ectopic thyroid tissue, it fails to localize exactly where along the path from the base of the tongue to the inferior neck any potential aberrant thyroid tissue exists. Contrast-enhanced CT is especially helpful for the evaluation of thyroid ectopia because of its excellent spatial resolution and ability to provide multiplanar images, which best identify smaller rests of ectopic thyroid tissue (Fig. 5.7), or any potential thyroglossal duct remnants.
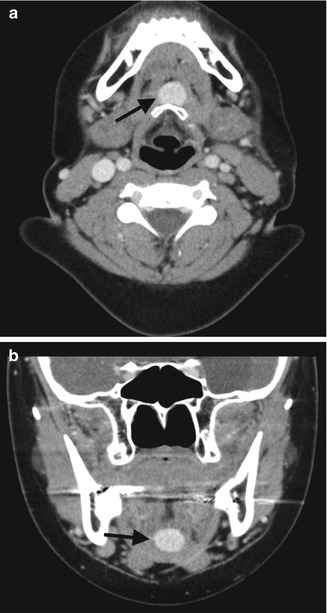
Figure 5.6
Lingual thyroid . An axial enhanced CT scan through the neck in a young child with hypothyroidism (a), a long-standing sensation of neck fullness, and tongue mass on radiographs show a clump of high attenuation thyroid tissue in the base of the tongue, known as a lingual thyroid. Ultrasound of the thyroid bed revealed no thyroid tissue in the expected location between the shadow of the tracheal air column (white arrows, a) and the carotid arteries (black arrows, b)
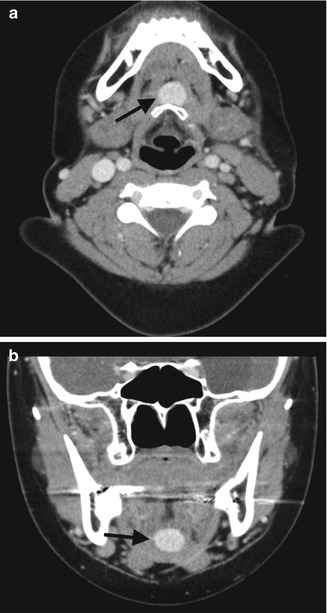
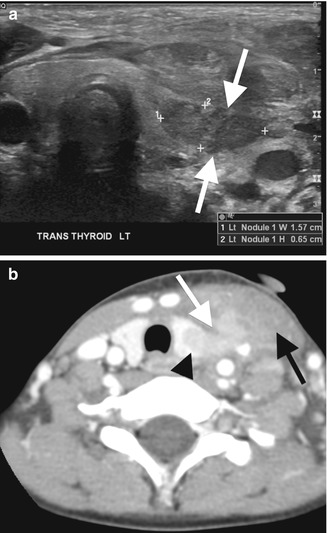
Figure 5.7
(a, b) Ectopic thyroid . Aberrant thyroid tissue may be found anywhere along the course of the thyroglossal duct, from the base of the tongue to the thyroid bed. Although scintigraphy is often espoused as the study of choice to identify ectopic thyroid tissue, it provides little spatial resolution. CT has the advantage of significantly better spatial resolution and the ability to provide multiplanar reconstructions, which can often better demonstrate rest of aberrant tissue, as shown in this patient with hypothyroidism, no thyroid tissue in the thyroid bed, and a small rest of aberrant thyroid (arrows) anterior to the hyoid bone
Thyroglossal Duct Cysts
The thyroglossal duct is a normally transient structure that involutes during fetal life; if it fails to do so, any remnants may slowly collect fluid and eventually manifest as a cystic neck mass. Ninety percent of thyroglossal duct cysts (TGCs) present before age 10, and the typical history is a young child with a painless and compressible midline or paramidline mass. There is often a history of waxing and waning size, which occurs when there is irritation from recurrent upper respiratory tract infection or minor trauma. Sometimes TGCs become secondarily infected and present as an acutely painful, inflamed mass. If a TGC has not been complicated by prior infection or bleeding, then it appears as an anechoic cystic mass with increased through transmission and sharp, well-defined margins. They are usually spherical but may have tubular configuration (Fig. 5.8). About half are found at the level of the hyoid bone, a quarter above it, and another quarter below it; they should never be found below the level of the thyroid. If complicated by prior hemorrhage or infection, TGCs may have more echogenic contents, small septations, and a thickened, irregular margin; they occasionally appear solid (although should still cause increased through transmission) (Fig. 5.9). Complete surgical resection is needed, or TGCs will recur.
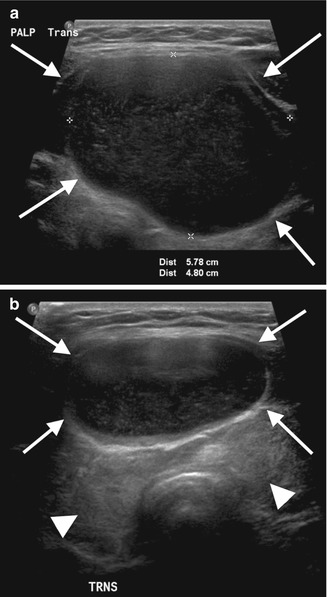
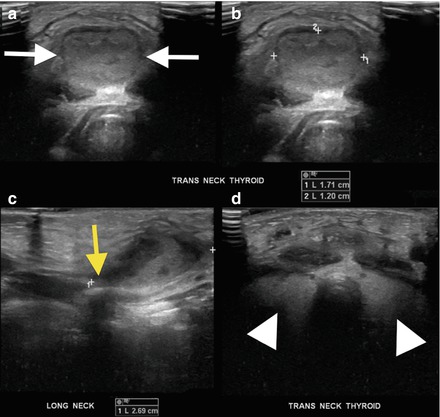
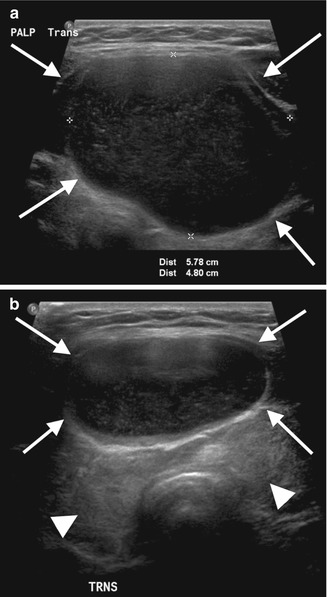
Figure 5.8
Thyroglossal duct cyst . An US was obtained on this teenager to evaluate a long-standing palpable thyroid mass. The mass turned out to be a thyroglossal duct cyst. Transverse US images show a predominantly anechoic cyst with scattered low-level echoes (arrows, a and b). This minimally complex thyroglossal duct cyst sits just above the level of the thyroid gland (arrowheads, b)
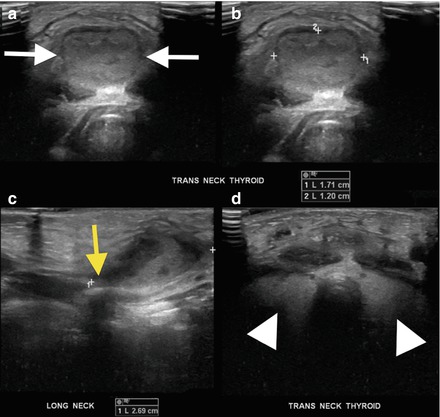
Figure 5.9
(a–d) Complex thyroglossal duct cyst . US was performed to evaluate a new painful thyroid mass in a 2-year-old boy. The images demonstrate that the mass is actually a heterogeneous, isoechoic cystic collection (calipers and white arrows) separate from the thyroid gland (arrowheads). This was an infected thyroglossal duct cyst; note its “tail” (yellow arrow) extending cephalad toward the tongue, reflecting this TGC’s embryologic origins
Branchial Apparatus Anomalies
Another embryologic anlage that may cause pediatric thyroid abnormalities is the branchial apparatus. Branchial apparatus anomalies (BAAs) include a spectrum of epithelial-lined remnants that only involve the left lobe of the thyroid. Third and fourth BAAs may become infected and cause suppurative thyroiditis, abscess, cystic mass, or sinus tract to the pyriform sinus; imaging depends on the specific patient’s complication. Suppurative thyroiditis—which can be caused by a BAA or occur primarily—begins as a focal area of abnormally decreased echogenicity within the thyroid (Fig. 5.10). With worsening infection and abscess formation, a complex focal fluid collection may develop, usually with heterogeneous but hypoechoic internal contents; if caused by a BAA, a sinus tract may extend up into the deep neck toward the pyriform sinus. Such complications are best visualized by contrast-enhanced CT imaging (Fig. 5.11).