Renal and bladder
• Urinary tract infection—febrile or recurrent nonfebrile
• Prenatal GU abnormality
• Voiding dysfunction
• Renal colic
• Palpable abdominal mass
• Single umbilical artery
• Hypertension
• Hematuria
• Proteinuria
• Azotemia
• Family history polycystic kidney disease
• Hemihypertrophy
• Urinary retention
• Syndrome associated with renal involvement (e.g., Tuberous sclerosis, CHARGE, VACTERL, WAGR)
• Surveillance of:
– Vesicoureteral reflux
– Nephrolithiasis
– Hydronephrosis
– Cystic renal disease
– Neurogenic bladder dysfunction (e.g., myelodysplasia)
– Obstructive uropathy (e.g., Posterior urethral valves)
Scrotal
• Palpable intrascrotal mass
• Acute scrotal pain
• Acute scrotal swelling
• Varicocele
• Testicular asymmetry
Technique
Kidneys : The kidneys are imaged in both longitudinal and transverse planes with the child primarily in the supine position. If the child is able to follow commands, the kidneys are best imaged with the child making a deep inspiration pushing the kidney caudally below the ribs. If the child cannot follow commands, the images might be better obtained with a bolster placed under the flank or with the child turned on the side and the arm raised above the head to open up the space between the ribs and the iliac crest allowing better access to the kidney. Images must be taken with the child in the prone position for better visualization of the kidney between the ribs. The right kidney is imaged along the anterior axillary line using the liver as an acoustic window while the left kidney is imaged along the posterior axillary line using the spleen as an acoustic window. Imaging is done with a curved linear array probe. For children under age 18 months or so, a 6–12 MHz probe is used while older children are better imaged using a 3.5–5 MHz probe.
Bladder : The bladder is imaged with the child in the supine position using a curved array probe (7.7–11 MHz for children under 18 months or 3.5–5 mHz for older children) which makes small skin contact and is easy to angle to gather the most information. The sonographer performs the study in both the transverse and longitudinal directions with the bladder at least partially filled looking for a normal bladder and surrounding organs and documenting any luminal, intraluminal, or extraluminal abnormalities. The transverse images are taken moving from the pubis to the umbilicus in 1–2 cm intervals while the longitudinal images are taken moving from the midline in either direction in 1–2 cm intervals. Measurements are made in the transverse plane measuring the height and width of the urine within the bladder and then the length in the sagittal plane. These three measurements are multiplied together and then multiplied by 0.65 [2] to calculate the bladder volume. Efflux of urine from the ureteral orifices can be demonstrated by applying the Doppler mode over the appropriate location on the bladder floor.
Scrotum : Ultrasound imaging of the scrotum is performed with the child supine and the scrotum supported by a folded towel placed between the thighs. In older children and adolescents, the penis position is maintained suprapubically with a second towel or held in position by the patient. Scanning should be performed with 7–18 MHz high-frequency linear array transducer. Both testes and epididymides should be compared for size, echogenicity, masses, and vascularity and imaged in both the transverse and longitudinal axes. Spectral Doppler analysis of the intratesticular vasculature of both testes is performed when indicated. In patients presenting with acute scrotum, the asymptomatic side should be scanned first so that grayscale and color Doppler gain settings are set optimally to obtain a baseline for comparison with the affected side. In the presence of a suspected varicocele, having the child perform the Valsalva maneuver or placing the child in the upright position can improve the evaluation of venous distention.
Documentation
The documentation of the ultrasound examination should be as complete and systematic as the examination itself. Mention should be made of normal and abnormal findings. All measurements that were taken should be documented. An example of some components of documentation of the kidneys, bladder, and scrotum is shown in Table 12.2.
Table 12.2
Documentation of ultrasound examination
Kidneys: | ||||||
Size: | ________ x_________x_________ | |||||
Abnormal location | No | Pelvic | Horseshoe | |||
Hydronephrosis | No | Grade | 1 | 2 | 3 | 4 |
Malrotated | No | Yes | ||||
Duplication | No | Yes | ||||
Proximal ureteral dilation | No | Yes | ||||
Cortical thinning | No | Yes | ||||
Abnormal cortical echotexture | No | Yes | ||||
Cortical cyst | No | Size____mm UP___MP___LP___ | ||||
Stones | No | Size____mm UP___MP___LP___ | ||||
Mass | No | Yes | ||||
Bladder: | ||||||
Pre-void volume | ________cc | Post-void volume | ________cc | |||
Thickened bladder | No | Yes | ||||
Distal ureteral dilation | No | Yes | ||||
Bladder mass | No | Yes | ||||
Pelvic mass | No | Yes | ||||
Bladder stones | No | Yes | ||||
Scrotal: | ||||||
Right Left | ||||||
Testis size: ________ x_________x_________ | ||||||
Testis mass | No | Yes | ____ mm Location______ | |||
Microcalcifications | No | Yes | ||||
Varicocele | No | Yes | _____mm | |||
Epididymal cyst | No | Yes | _____mm | |||
Hernia | No | Yes | ||||
Hydrocele | No | Yes | ||||
Kidney
Normal Anatomy
The proper evaluation of kidney assesses the location, orientation, axis, size, echogenicity of the parenchyma and the integrity of its contour, the nature of the central echogenic focus, and the absence of a visible proximal ureter (Fig. 12.1).


Fig. 12.1
Sagittal view of a normal kidney demonstrating a normal position in the flank and a normal axis, with good corticomedullary differentiation, a collapsed central echogenic focus, and hypoechoic pyramids oriented radially about the perimeter
Normal kidneys lie in the retroperitoneum along the psoas, orientated parallel to it; both are oblique such that the upper pole of the kidney is posterior to the lower pole. The size of the kidney is age-dependent and is determined by measuring the distance between the two poles and compared to published nomograms [3]. From a sonographic perspective, the most important neighbor is the anterior relationship to the liver on the right side and the spleen on the left side. During the first several months of life, the echogenicity of the renal parenchyma may be isoechoic or hyperechoic in comparison to the adjacent liver or spleen and then becomes hypoechoic in comparison.
The renal cortex can be distinguished from the medulla by the presence of a line, reflecting the subtle differences in echogenicity. The presence of this corticomedullary differentiation is an indicator of normal architecture and a marker of parenchymal integrity.
The contour of the pediatric kidney can be smooth but is often lobulated. The lobes of parenchyma consist of a central pyramid covered by cortical parenchyma and the Columns of Bertin are located between these pyramids. The lobulated appearance regresses with time and the contour becomes smooth.
The renal pyramids are seen as hypoechoic areas radially distributed surrounding the central echogenic focus (CEF) that are most commonly seen in infants and also regress with time. The CEF consists of the renal pelvis, hilar vasculature and lymphatics, and sinus fat (accounting for its hyperechoic appearance). In the sagittal plane, there is ordinarily a single CEF surrounded by a symmetric thickness of parenchyma. The CEF should be collapsed upon itself unless it is distended with urine and the walls of the renal pelvis separate. The proximal ureter should not normally be visible on sonogram .
Renal Anomalies
Anomalies or abnormalities of the kidneys in children can be described developmentally as either congenital or acquired and then again anatomically by number, location, vascular, parenchymal, and collecting system.
Unilateral Renal Agenesis (Fig. 12.2)

Fig. 12.2
An empty renal fossa demonstrating the psoas muscle posterior and the normal liver anterior and superior
Unilateral renal agenesis is most commonly detected in children during imaging performed (1) prenatally, (2) for a urinary complaint, (3) during screening for associated anomalies, or (4) incidentally during evaluation of unrelated conditions. On ultrasound, the renal fossa is empty of a reniform structure and may instead be occupied by bowel. Otherwise the surrounding organs are normal in appearance. It is important that the person performing the study then scans the pelvis to determine if the kidney is ectopic in position. In infants, the adrenal will be prominent and in the normal anatomical position. The remaining kidney will be large reflecting compensatory hypertrophy. The diagnosis can be confined by nuclear scintigraphy (DMSA), MR, or CT; although Krill et al. found that measuring the polar size of the kidney on ultrasound offers sufficient accuracy in predicting a solitary kidney [4]. VCUG is indicated because of the significant incidence of vesicoureteral reflux in the remaining renal unit [5].
Renal Ectopia
Kidneys begin their embryologic journey in the bony pelvis with the renal pelvis oriented anteriorly and then reach the renal fossa and finish their medial rotation by the ninth week of gestation. However, this process may abort anywhere along the course of ascent. Similarly, the metanephric blastema may cross over to the contralateral side and may attach to the other metanephric blastema (crossed-fused ectopia ).
A normal appearing reniform kidney may be seen in the pelvis behind the bladder (Fig. 12.3). However, because of the associated malrotation of a pelvic or crossed (fused, non-fused) kidney, the cortex may appear variable in echogenicity and in corticomedullary differentiation. Also, or for the same reason, measurement of polar length may be artificially small.
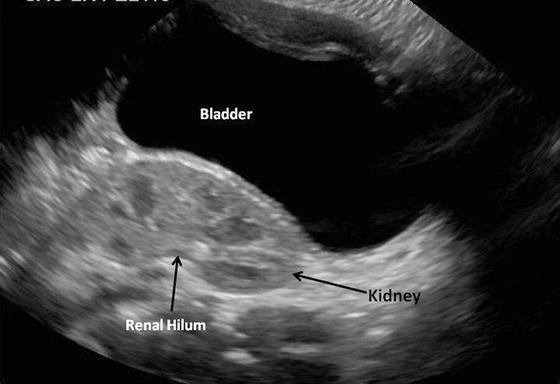
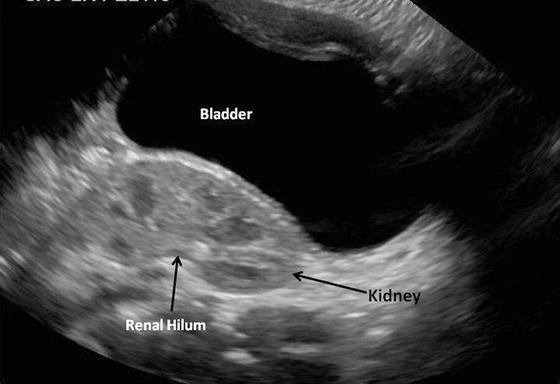
Fig. 12.3
The presence of an ectopic kidney in the pelvis situated posterior to the urinary bladder. The kidney has normal contour and echogenicity but is malrotated due to incomplete medial rotation during ascent
The horseshoe kidney is the most common fusion anomaly in children (Fig. 12.4). This may be suspected when both malrotated kidneys are positioned caudal to their usual position. Horseshoe kidneys are at risk for UPJ obstruction and Wilms’ tumor and these may be detected easily by ultrasound. The isthmus between the two kidneys may be thick on ultrasound; function of the isthmus can be evaluated by nuclear scintigraphy.
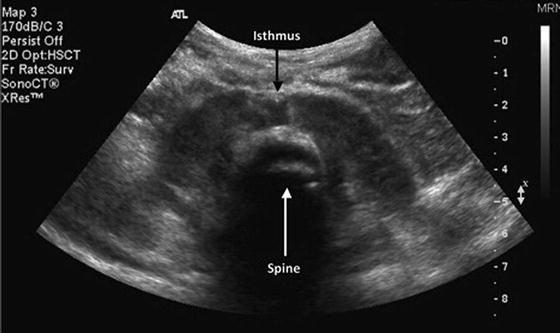
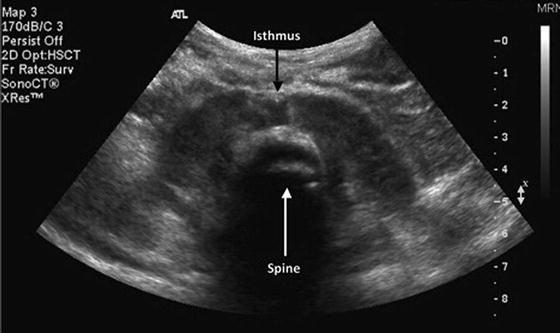
Fig. 12.4
Transverse view demonstrating the caudal location of malrotated and fused kidneys, i.e., a horseshoe kidney. The isthmus is identified in the midportion of the kidney and the spine located posteriorly
Renal Vein Thrombosis
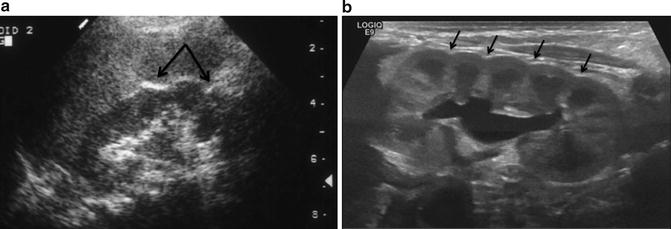
Ultrasound is well suited for evaluating the kidney with suspected renal vein thrombosis . Risk factors for renal vein thrombosis include dehydration, traumatic delivery, and sepsis. During the acute phase, during which there is considerable edema, ultrasound will demonstrate an enlarged kidney with loss of corticomedullary differentiation (Fig. 12.5). The parenchyma is hypoechoic early in the process due to edema but becomes hyperechoic as fibrosis sets in. Thrombi in smaller vessels are seen as radiating linear echogenic bands in the parenchyma. At later phases, atrophy will be seen as well as calcifications in the area of the thrombi. Venous flow is absent when Doppler is applied .
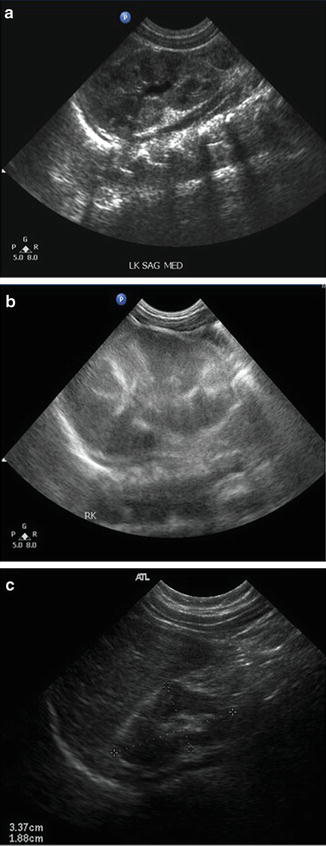
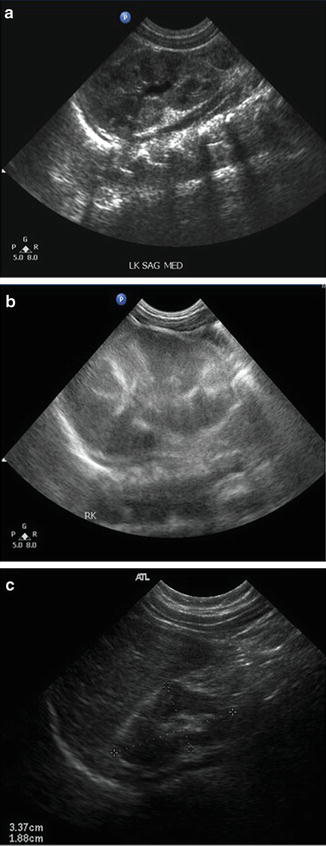
Fig. 12.5
Sequence of renal sonograms from a neonate with renal vein thrombosis. (a) Sagittal view of the left kidney demonstrating normal echogenicity and pyramids with grade 1 hydronephrosis. (b) Sagittal view of the right kidney taken at the same time as (a) demonstrates a larger kidney with poor corticomedullary differentiation. (c) Six months later, the left kidney has become atrophic and continues to have poor corticomedullary differentiation
Infection and Scarring (Fig. 12.6)
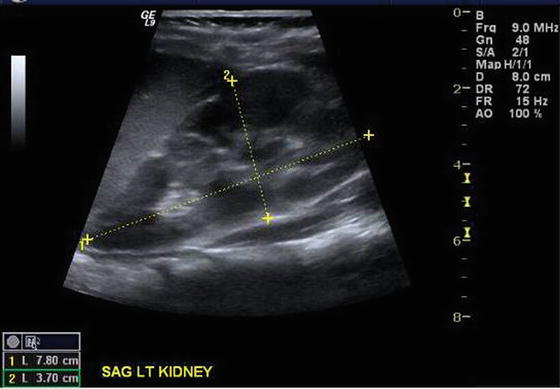
Fig. 12.6
Sagittal view of the kidney of a hospitalized, febrile (103.4 °F), 3-year-old girl whose catheterized urine culture grew 100,000 E. Coli. The kidney is enlarged (7.8 cm) and has disturbed echogenicity due to edema and inflammation
Urinary tract infections are a leading indication for ordering renal ultrasound in children. The spectrum of the clinical presentation of UTIs is variable and often matches the ultrasound findings. In many cases, the sonogram of the kidneys and bladder are completely normal. In some cases, all is normal except for some self-limited mild hydronephrosis or hydroureter as a result of the dilating effect of bacteria-released endotoxins. When there is diffuse pyelonephritis, the kidney will be enlarged and hypoechoic (either diffusely or multifocal) with loss of corticomedullary differentiation.
Following a pyelonephritic episode, particularly when associated with vesicoureteral reflux, the healing parenchyma may leave a scar. The scar needs to be large to be detected on ultrasound: the indented contour in the area(s) of scar reflecting cortical loss. This contraction of parenchyma may be focal or in severe cases involves the entire kidney. In such cases, the size of the kidney will also contract. One needs to avoid confusing these scars with persistent fetal lobulations. Scarring typically occurs over calyces (the point of retrograde entry of bacteria to the parenchyma) while the contour indentations associated with fetal lobulations are between the calyces (reflecting the adjacent lobes of renal development) (Fig. 12.7).