Diffusion-weighted imaging (DWI) is a powerful imaging technique in neuroimaging; its value in abdominal and pelvic imaging has only recently been appreciated as a result of improvements in magnetic resonance imaging technology. There is growing interest in the use of DWI for evaluating pathology in the pelvis. Its ability to noninvasively characterize tissues and to depict changes at a cellular level allows DWI to be an effective complement to conventional sequences of pelvic imaging, especially in oncologic patients. The addition of DWI may obviate contrast material in those with renal insufficiency or contrast material allergy.
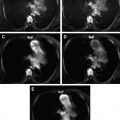
Diffusion-weighted imaging (DWI) is a well-established, powerful imaging technique used in neuroimaging but its value in abdominal and pelvic imaging has only recently been appreciated as a result of improvements in magnetic resonance (MR) imaging technology (eg, stronger diffusion gradients and parallel-imaging sequences). The usefulness of DWI in the abdomen and pelvis is linked to its capacity to more accurately characterize tissues, potentially differentiating malignant from benign entities.
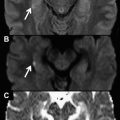
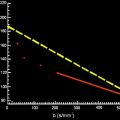
DWI is based on the principle of diffusion of water molecules in an environment. The restriction to flow of water molecules is governed by tissue cellularity (local environment) and the integrity of the cell membrane. Tumors typically display restricted diffusion because of their hypercellularity ; however, other types of disease conditions have been associated with restricted diffusion, including cytotoxic edema, abscess, and fibrosis. Tissues with low cellularity or those composed of cells with disrupted membranes allow greater movement of water molecules, which is visualized as decreased signal intensity on DW images and increased signal intensity on corresponding apparent diffusion coefficient (ADC) maps. This unique ability to characterize malignant tumors may obviate contrast material in those patients with renal insufficiency or contrast material allergy.
Examination of the pelvic region using DWI
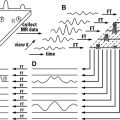
DWI is sensitive to the random displacement of water molecules within tissues and is performed by using echo planar imaging (EPI) combined with balanced motion-probing gradients (MPG), which are symmetric and of equal intensity about the 180° refocusing pulse. These MPG exploit the phase offset induced by the random motion of water molecules to discriminate tissues that restrict that motion of water. The intensity of MPG pulses is represented by the b-value (s/mm 2 ), a measure of the strength of the diffusion-sensitizing gradient. By using multiple b-value MPG, one can map and calculate the ADC.
Because the DWI sequence is a T2-weighted sequence, the DWI signal is influenced by the T2 of the tissue being imaged. Therefore, the interpretation of DWI must occur concomitant with the ADC image. High-intensity tissues on T2-WI may show increased signal intensity on DWI (the so-called T2 shine-through effect) if also high on ADC. For example, DWI with an intermediate b-value (eg, 500 s/mm 2 ) shows increased intensity not only in tumors but also in cysts. Thus, DWI with a higher b-value (eg, 800 or 1000 s/mm 2 ) may be required for the pelvis.
When imaging the abdomen and pelvis optimization of other sequence parameters is crucial because EPI is highly susceptible to distortions in the spatial field caused by air-containing bowel loops. To minimize susceptibility artifacts, shorter echo times (TE) and smaller numbers of echo train lengths (ETLs) are preferable; this can be achieved by the use of parallel-imaging techniques. Unlike sequential acquisitions, parallel imaging is based on the use of coils with multiple small detectors that operate simultaneously to acquire MR data. Each of these detectors contains spatial information that can be used as a substitute for time-consuming phase-encoding steps, thereby allowing both the acquisition time and the ETL to be reduced. In particular, DWI with parallel imaging reduces the number of phase-encoding steps. The effective TEcan be shortened and susceptible components of the ETL can be eliminated. This strategy keeps the susceptibility effect to a minimum. Although a wider receiver bandwidth reduces the signal-to-noise ratio (SNR), its use is recommended because it shortens the duration of the MR signal acquisition and reduces susceptibility artifacts.
In our standard protocols for pelvic DWI we use a 3-T magnet unit Magnetom Trio (Siemens, Erlangen, Germany) with a 6-channel body MATRIX and a gradient-recalled echo (GRE) EPI sequence (repetition time [TR] 5000 ms; TE 75 ms; field of view 400 mm; 4 averages; slice thickness 4 mm; interslice gap 1 mm; acquisition matrix 162 × 162; EPI factor 76; and bandwidth 2058 Hz/pixel) with fat suppression (spectral attenuated inversion recovery) and parallel-imaging technique (gene-ralized autocalibrating partially parallel acquisition [GRAPPA] factor of 2) using b-values of 0, 500, and 1000 s/mm 2 . Imaging time of DWI is 155 seconds for 30 slices. On a 1.5-T MR imaging scanner (Magnetom Avanto, Siemens, Erlangen, Germany) with a 6-channel torso coil we use a GRE EPI sequence (TR 2600 ms; TE 82 ms; field of view 350 mm; 2 excitations; slice thickness 7 mm; interslice gap 1 mm; acquisition matrix 128 × 128; EPI factor 128; and bandwidth 1302 Hz/pixel) using b-values of 0 and 1000 s/mm 2 with fat suppression and parallel-imaging technique (GRAPPA factor of 2) with an imaging time of DWI of 60 seconds for 20 slices. On a 1.5-T MR imaging scanner (Philips Intera, Philips Medical Systems, Best, Netherlands) with a 6-channel body coil we use a spin-echo (SE) EPI sequence (TR 2000 ms; TE 71.73 ms; flip angle 90°; field of view 280 mm; 2 excitations; slice thickness 5 mm; interslice gap 0.5 mm; acquisition matrix 128 × 128; ETL 111) with bandwidth of 1.7546 Hz/pixel with fat suppression and parallel-imaging technique (SENSE factor of 2) and an imaging time of DWI of 168 seconds for 23 slices. For a GE Excite system (General Electric Medical Systems, Milwaukee, WI, USA) at 1.5 T we use an SE EPI sequence (TR 5000 ms; TE 93 ms; flip angle 90°; field of view 280 mm; 2 excitations; slice thickness 5 mm; interslice gap 0.5 mm; acquisition matrix 128 × 128;) with bandwidth of 1.953 Hz/pixel with fat suppression and an imaging time of DWI of 4 minutes 30 seconds for 30 slices, 2 b-values (0 and 1000), and 6 directions. DWI is performed in the axial and also in the sagittal plane. The MPG pulses are placed in the x, y, and z axes. Respiratory trigger is not used. Data are then collected using echo planar readout. Fat suppression is added to the DWI to avoid chemical shift artifacts.
Isotropic DW (trace) images are reconstructed for b = 0, 600, 800, and 1000 s/mm 2 . From these b-values, ADC maps are computed. ADC measurement is performed on the axial and/or sagittal planes depending on the one that contained the largest region of interest that can be drawn.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree