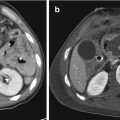
Fig. 21.1
Acute arterial bleeding; axial CT image of the pelvis on arterial (a) and venous (b) phases. Extravascular hyperattenuating focus with attenuation similar to that of the iliac arteries in the extraperitoneal left pelvic space (arrow) (a) enlarging (arrow) in the following phase of acquisition (b)

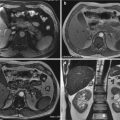
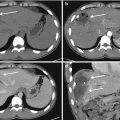
Fig. 21.2
Venous bleeding; axial CT image of the pelvis without c.m. (a) and with c.m. on arterial (b), venous (c), and capillary late (d) phases. Extrapelvic hematoma seen as an iso-hypoattenuating area in the right gluteal region (a) has the same attenuation values in the arterial phase (b). In the portal venous phase (c), a late focus of extravascular hyperattenuation appears into the hematoma (arrow), enlarging during capillary late phase (arrow) (d)
Fractures involving the lesser sciatic foramen and mostly the greater sciatic foramen, common pathway for many pelvic vessels, have a great risk of bleeding, especially from the superior gluteal and the internal pudendal arteries. Therefore, the fracture location can be used to presume the injured artery [10, 11] but a readily and certain identification can only be obtained by a CT angiography.
There are a host of factors that influence the diagnostic quality of a CT examination and lead to a misinterpretation [12] but a careful attention to technique is crucial. For the purposes of this review, we will not discuss about contrast media CT protocol but it should be noted that a preliminary unenhanced scan must be obtained to differentiate active extravasation from other high-attenuation entities, such as bone fragments, foreign bodies, or drugs [13] (Fig. 21.3). Once ongoing hemorrhage is identified as focal area of high attenuation (greater than 90UH), equally important are coronal maximum intensity projection (MIP) reformatted images, useful to detect the exact site of extravasation [5]. Finally, multiplanar reformation (MPR), viewed in combination with axial images, may be used to evaluate vessel along its long axis and reveal subtle injuries [1] (Fig. 21.4).



Fig. 21.3
Unenhanced (a) and post-contrast arterial phase (b) axial CT image. Hyperdense area close to the right ischio-pubic branche (long arrow) showing an attenuation higher than that of the iliac arteries (short arrows) (b) but equal in both unenhanced (a) and arterial (b) phases, corresponding to a bone fragment

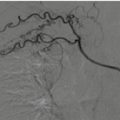
Fig. 21.4
Axial unenhanced (a) and arterial phase (b) CT image, coronal reformatting (c) and angiography (d) of the pelvis. Large extraperitoneal hematoma in the left pelvic side wall, appearing as an hyperattenuating collection in the unenhanced (a) and arterial axial images (b); the coronal reformatting of the arterial phase (c) shows a minute focus of enhancement (arrow), corresponding to an active arterial bleeding. Selective angiography (d) confirmed blood extravasation and the exact site (arrow)
21.6.2 Other Form of Vascular Injuries
Vessel injuries may be present in the absence of active hemorrhage [5]. These lesions must be known and accurately identified since can be a source of emboli, occlusion, or progress to complete rupture with a concomitant active hemorrhage. Vessel wall injuries have a spectrum of imaging more subtle at CT, ranging from irregular narrowing and outpouching to complete occlusion.
21.6.2.1 Intimal Tear and Arterial Dissection
At imaging, the separation of the intima from the adjacent media leads to a segmental, linear, or curvilinear hypoattenuating filling defect originating from the vessel wall in the enhanced arterial lumen. In the case of dissection, blood is interposed between the intima/inner media and the outer adventitia by forming a true and false lumen. Arterial dissection may be caused by mechanical forces from trauma often in combination with underlying arteriopathies. Dissection may cause thromboemboli that may occlude the arterial lumen. With thrombosis an arterial dissection may manifest at CT as a crescent focal region of vessel narrowing. Traumatic dissection can also be the cause of an intermittent ongoing bleeding, not evident on CT, and therefore it requires an angiographic study [4, 7, 13].
21.6.2.2 Pseudoaneurysm
A pseudoaneurysm occurs secondary to a complete or partial disruption of the wall vessel with blood contained by the adventitia or perivascular tissues through formation of a fibrous capsule (Fig. 21.5). Pseudoaneurysm are unstable and at increased risk for rupture or partial thrombosis and cause emboli to distal organ. At imaging, a focal well-circumscribed arterial outpouching of contrast-enhanced blood is seen adjacent to the vessel lumen. On portal veins and delayed phase images, pseudoaneurysm does not enlarge and reflect the attenuation of the blood pool, showing a hypoattenuating values over time as arterial enhancement washes out [4, 7, 13] (Fig. 21.6).



Fig. 21.5
Pseudoaneurysm: a complete or partial disruption of the wall vessel leads to an outpouching blood collection delimited by adventitia or fibrous capsule

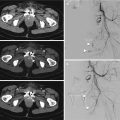
Fig. 21.6
Pseudoaneurysm on axial CT image on arterial (a) and venous (b) phases. A focal well-circumscribed arterial outpouching of contrast-enhanced blood is seen inside left iliac muscle (arrow) in the arterial phase (a). On portal venous phase (b), the area does not enlarge and it reflects the attenuation value of the blood pool
21.6.2.3 Occlusion
Occlusion of a major vessel may result from intimal disruption with subsequent platelet aggregation, leading to thrombosis. A full-thickness injury with spasm also can cause a vessel occlusion and in these cases the possibility of hemorrhage should be taken seriously, even if there is no extravasation of c.m. when CT is performed. Occlusion appears as abrupt cutoff of a contrast-enhanced vessel [4, 13].
21.6.2.4 Focal Stenosis
Intra- or extramural hematoma, intimal injuries with partial thrombosis, and spasms are all potential causes of focal areas of narrowing and irregularity of the arterial lumen. On CT images, generally, it can be hard to differentiate a spasm from a true injured vessel and although an arterial spasm generally appears as concentric smoothly tapered traits of narrowing adjacent or even distal to the site of injury, imaging findings are not specific and cannot be used to exclude other type of vessel injuries. Nevertheless, vasospasm should remain in the differential diagnosis because, although it may resolve spontaneously, it can also mask an intraluminal thrombosis [7].
21.6.2.5 Arteriovenous Fistula
Arteriovenous fistulas, a direct communication between an artery and a vein, are rare in blunt trauma and difficult to detect and the diagnosis often delayed. Although infrequent, immediate diagnosis of this injury is important due to high risk of rupture. The typical finding on MDCT is an early filling of a pelvic vein with contrast material in the arterial phase when c.m. should only be visible within the pelvic artery. It is important to look through contralateral anatomic equivalent of the pelvis veins because an asymmetric early filling can also be diagnostic [4, 7, 13].
21.7 Urological Injuries After Pelvic Trauma (Urinary Bladder and Urethra)
Genitourinary injuries are well-identified complications and occur in as many as 15–20% of pelvic fractures cases, especially if pubic symphysis is involved (3,8). Pelvic fracture pattern, as shown by the pelvic X-ray eventually performed at emergency room, may predict the risk of genitourinary injury and the presence of blood at the urethral meatus and gross hematuria [14], should raise the suspicion for a genitourinary injury. In patients with blunt trauma pelvic fracture associated with bladder injury, it was demonstrated that pelvic injuries included diastasis of the pubic symphysis greater than 1 cm and fracture of obturator ring, with a displacement greater than 1 cm [15]. In the western world, the most common cause of urological injuries are wide-impact blunt abdominal traumas in road accidents, but the incidence of penetrating trauma is increasing [16, 17]. Whether the trauma is blunt or penetrating, associated multiorgan injuries are common and affect frequently the liver and the spleen [18].
21.7.1 Urinary Bladder Trauma
Motor vehicle crashes, falls, and crush injuries are the most frequent cause of bladder trauma [19] and major mechanisms of injuries are blunt trauma or penetrating trauma by fracture fragments. In any case, 60–90% of patients suffering from a blunt trauma bladder injury have associated pelvic fractures [19] and 25% of intraperitoneal bladder lesions occur without a pelvic fracture [20]. Injuries range from contusions to rupture and most of the ruptures result from a blunt trauma with distended bladder. In effect the type and the extent of lesion depend not only on external mechanism but also on the state of bladder relaxation at the time of trauma. Beyond contusion lesions, limited to the mucous membrane with no imaging finds [21], intraperitoneal rupture occurs when a strong compression on the lower abdomen causes sudden increase in pressure in a distended lumen bladder. The rupture affects the dome which is the weakest portion of the bladder and covered by peritoneum, causing an intraperitoneal extravasation which outline peritoneal structures, such as the bowel and the mesentery. Yet most frequent bladder injuries are extraperitoneal rupture (accounting for 80–90% of cases) and generally associated with pelvic fractures [14]. Urine extravasation can be restricted in the pelvic extraperitoneal space (simple extraperitoneal rupture) or reach distant locations, as the anterior abdominal wall, the penis, the scrotum, and the perineum since the injury may cause a disruption of the fascial planes of the pelvis (complex extraperitoneal rupture). Combined intraperitoneal and extraperitoneal bladder injuries occur in as many as 5% of major bladder trauma [14].
21.7.1.1 Classification
The American Association for the Surgery of Trauma (AAST) classified bladder injuries according to five grades scale, while the Societé Internationale d’Urologie (SIU) uses a classification into four types (type 1 bladder contusion, type 2 intraperitoneal rupture, type 3 extraperitoneal rupture, type 4 combined injury). The latter classification does not take into account the length and extent of the wall laceration but it simply aims to determine the presence of the injury as assessed by contrast extravasation on CT cystography [14].
21.7.1.2 Imaging
Diagnosis of bladder injury on MDCT may be challenging if bladder is not well distended. On the other hand, polytrauma patients are catheterized and bladder is empty when they are examined. Decision to performing a CT cystography is taken on the basis of clinical and radiological basis. The finding of pelvic fractures may be determinant but if associated with gross hematuria, the indication for evaluation of bladder is absolute. Relative indications are also gross hematuria without pelvic fracture, microhematuria with pelvic fracture, and isolated microhematuria. The only reliable method for filling the bladder is the retrograde active distension with c.m [14]. The passive distension of the bladder during the abdominal CT cannot be considered reliable on to diagnose bladder rupture, even with bladder catheter clamped or acquisition of a delayed scan, no matter if bladder appears distended. Indeed, the antegrade approach may detect intra- or extraperitoneal fluid but is not capable to differentiate urine from ascites. 300 ml of diluted water-soluble iodinated radiopaque c.m. is introduced into the bladder through a urethral catheter, and a CT scan performed before the infusion of intravenous c.m. for routine next abdominal CT [22]. Typically, a CT cystography shows a contrast extravasation into perivesical fat and occasionally into anterior abdominal wall, allowing a distinction between intra- and extraperitoneal rupture (Figs. 21.7 and 21.8). This distinction has a paramount importance and immediate therapeutic implications because intraperitoneal rupture requires surgical management while extraperitoneal rupture can be treated conservatively [23].