Pelvic USG (Uterus and Ovaries)
Full bladder is required for pelvic USG as fluid in the urinary bladder facilitates transmission of sound waves for better visualization of uterus and ovaries.
Prepubertal: Inverse pear shaped. Body of uterus is smaller than cervix.
Nonvisualized endometrial cavity.
Measures approximately 2 − 3.5 × 0.5 − 1.0 centimeters (L × AP).
Postpubertal: Nulliparous, pear shaped.
Measures approximately 4.5 − 9.0 × 1.5 − 3.0 × 4.5 − 5.5 centimeters (L × AP × T).
Uterine dimensions increase by 1–1.2 centimeters with parity and its body becomes rounded (Table 10.1).
Pattern of endometrium varies with menstrual cycle.
Anteroposterior diameter of cervix should not exceed that of uterine body.
Postmenopausal: Smaller and homogeneous with nonvisualization of endometrial cavity.
• Muscles in uterine walls appear hypoechoic.
• Posterior cul-de-sac (POD—Pouch of Douglas) is the most posterior and inferior reflection of peritoneal cavity located between rectum and vagina.
• Adnexa include ovaries, fallopian tubes, ligaments, and vessels.
Anteverted: Cervix and vagina forms a 90-degree angle (Figure 10.1).
Anteflexed: Body is flexed normally anteriorly on the cervix (270 degrees).
Retroverted: Uterus is tilted posteriorly toward the spine.
Figure 10.1 Showing normal echotexture of uterus, cervix, and vagina.
Table 10.1 Illustrates uterine dimensions in different stages of female
Uterus | Uterine length | Fundus: cervix | Endometrium |
Newborn | 3.5 centimeters | 1:2 | Bright endometrial stripe (due to in utero hormonal stimulation) |
Prepubertal | 2.5–3.5 centimeters | 1:1 | No endometrial stripe seen |
Postpubertal | 5–8 centimeters | 3:1 | Endometrium varies with menstrual phase |
Leads to poor visualization of the endometrial cavity.
Visualization of broad ligament leads to widening of adnexa.
Fundus appears echo poor in appearance simulating a fundal fibroid.
No contour abnormality and displacement of endometrium differentiates it from fibroid. TVS is better.
Retroflexed: Fundus points backward. Cervix may be interposed between the probe and the body of uterus.
Constricted lower part of the uterus connecting main body of the uterus to the vagina.
Nabothian cysts: Cysts within the cervix representing dilated or obstructed endocervical glands. Clinically not significant. Single cyst may sometimes simulate as low implanted gestational sac (Figure 10.2).
Bulky cervix: Anteroposterior diameter of cervix >~3.0 centimeters. Heterogeneous echotexture, history of white discharge warrants pap smear evaluation and follow-up. May occur due to cervicitis, fibroid, and malignancy.
Figure 10.2 Showing multiple nabothian cysts in the cervix.
Tubular structure with hypoechoic walls surrounding the central hyperechoic apposed surfaces of vaginal mucosa.
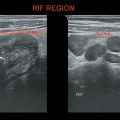
Bilateral oval, homogeneous structures lying laterally to the uterus with multiple well-defined anechoic follicles (Figure 10.3).
Ovarian volume—(L × W × AP) × 0.53 (Table 10.2).
Postmenopausal—1–6 cubic centimeters (>8 cubic centimeters is abnormal)—Ovaries are smaller, difficult to recognize. Sometimes they are hyperechoic without any follicles and similar to the surrounding tissues.
In some females up to 14–18 cubic centimeters of ovarian volume may be seen normally. Look for arrangement of follicles and stroma before diagnosing polycystic ovarian disease (PCOD) (Table 10.3).
Figure 10.3 Depicting bilateral ovaries in the adnexa and a normal ovary showing multiple follicles with dominant follicle.
Table 10.2 Illustrating ovarian volume in different age groups of females
<5–6 years | <1 cc |
6–11 years | 1.0–2.5 cc |
>11 years | up to 10 cc |
Premenstrual: Hyperechogenic
Postmenstrual: Thin, hypoechoic line (Table 10.4 and Figure 10.4)
Postmenopausal (not on hormone replacement therapy [HRT]) <4 millimeters ideally or maximum 8 millimeters
Table 10.3 Illustrating varying appearances of ovary in different stages of menstrual cycle
Days of menstrual cycle | Appearance |
5–7 days | Multiple small anechoic follicles in the ovary. |
8–12 days | One dominant follicle can be recognized, which increases in size up to 16–28 millimeters. |
24 hours before ovulation | Cumulus oophorus may be seen. |
At the time of ovulation | Follicle ruptures, expels the ovum into fallopian tubes. The remnants of the follicle are known as corpus luteum, which produces estrogen and progesterone for sustaining favorable conditions for implantation of ovum, if it gets fertilized. Follicle reduces in size and may be filled with echogenic debris. May retain fluid over next 4–5 days and increases in size to 2–5 centimeters. Corpus haemorrhagicum—if bleeding occurs into the follicle. Corpus albicans—if no pregnancy occurs and corpus luteum involutes. |
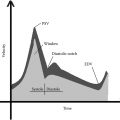
Table 10.4 Illustrating appearance of endometrium during different phases of the menstrual cycle
Date of cycle | Phase | Thickness | Appearance |
1–4 days | Menstrual | 1–4 millimeters | Thin interrupted central echo Small amount of fluid seen endovaginally |
5–14 days | Proliferative | 4–8 millimeters | Central echogenic line surrounded by thin hypoechoic (dark) band |
Periovulatory | 6–10 millimeters | Trilayered appearance Dark band with thin echogenic line on either side | |
15–28 days | Secretory | 8–16 millimeters | Thick, echogenic endometrium |
Figure 10.4 Illustrating varying appearances of endometrium depending on phases of menstrual cycle.
On HRT
Sequential HRT: Monthly withdrawal bleeding and cyclical endometrial thickening. At mid cycle 8–15 millimeters.
Continuous HRT: No cyclical endometrial changes with maximum 8 millimeters thickness.
1. Exclude pregnancy by urinary pregnancy test (UPT)
2. Dysfunctional/anovulatory uterine bleeding (DUB) is the most common cause (termed as hormonal imbalance)
3. Organic pathologies—Submucous myomas, polyps, hyperplasia, and carcinoma
In postmenopausal patients
• Thin, distinct endometrial echo <4–5 millimeters—high negative predictive value.
• Endometrial fluid collection with thin endometrium surrounding the fluid s/o inactive atrophic endometrium (secondary to cervical stenosis).
• Endometrial fluid collection—Endometrial tissue surrounding the fluid is thick and irregular suggestive of endometrial hyperplasia with atypia. Suggest saline infusion sonohysterogram.
• Polyp—Look for a feeder vessel.
• Submucous fibroid.
Figure 10.5 Illustrating thickened endometrium with cystic changes on a patient with carcinoma breast on tamoxifen.
K/C/O carcinoma breast on tamoxifen—Microcystic changes due to glandular cystic atrophy (Figure 10.5).
Localized overgrowth of endometrial glands and stroma can be
• Sessile
• Pedunculated
Three types:
Hyperplastic: Resembles glands of endometrial hyperplasia.
Atrophic: Cystic and dilated atrophic glands.
Functional: Undergo cyclical endometrial change.
Feeder vessel (Pedicle) seen entering the endometrium.
Common in perimenopausal and postmenopausal females.
USG—Endocavitary iso/hyperechoic mass surrounded by fluid (Figure 10.6).
D/D submucous fibroid—Broad base and irregular contour.
Normal layer of overlying endometrium can be appreciated.
Sonohysterography is diagnostic, in which 5 milliliters saline is infused into the endometrial cavity through a catheter during TVS.
Figure 10.6 Illustrating endometrium polyp in saline hysterography.
Excessive proliferation of endometrial glands. Thickening is hypovascular to differentiate from hypervascular carcinoma (Figure 10.7).
Due to unopposed estrogen stimulation (anovulatory, states, obesity, tamoxifen therapy).
S/s—Postmenopausal bleeding.
Simple: Cystic → cystic dilation of glands with abundant cellular stroma.
Complex: Adenomatous—More number of glands with scanty stroma.
In symptomatic postmenopausal female, endometrium >5 millimeters → abnormal
In asymptomatic postmenopausal female, endometrium >5–8 millimeters → abnormal
Figure 10.7 Illustrating thickened hyperplastic endometrium.
Figure 10.8 Illustrating thickened, heterogeneous endometrium.
In premenopausal, it is abnormal if
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree