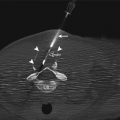
Fig. 18.1
Illustration of an ultrasound-guided renal biopsy in the sagittal plane shows sampling of the renal cortex from the inferior pole. The right kidney is most commonly selected due to its more caudal location, compared to the left

Fig. 18.2
A 47-year-old woman with multiple myeloma and renal dysfunction. Ultrasound-guided biopsy of the right renal cortex
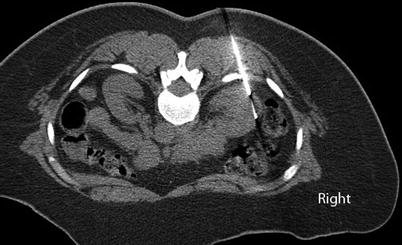
Fig. 18.3
A 73-year-old woman with morbid obesity and renal dysfunction of unknown etiology. CT guidance was chosen for biopsy of the right renal cortex due to the patient’s body habitus. Axial CT image of the abdomen in prone position shows the biopsy needle inserted into the lateral aspect of the right kidney
Devices
When percutaneous renal biopsy was first introduced, 14-gauge manual needles (e.g., Tru-Cut) were used to obtain large samples of renal cortical tissue. Subsequently, spring-loaded biopsy needles were introduced to clinical practice and have increasingly gained popularity. Large-gauge (14 gauge) manual needles provide a large number of glomeruli per core biopsy sample [31, 32]. Automated needles provide more glomeruli per core biopsy than provided by manual biopsy needles of the same gauge [33, 34]. For needles of similar gauge, there is no difference in the number of complications between manual and spring-loaded needles [33], but when 14-gauge manual needles were compared to smaller automated needles, there were fewer complications with the smaller automated needles [31, 35, 36]. In addition to the needle size and mechanism of action, the number of cores taken during the biopsy helps determine the success of the procedure. Some investigators recommend obtaining at least two core biopsy samples from the kidney [17, 28, 37].
Approaches, Relevant Anatomy, and Technical Considerations
Percutaneous renal biopsies are usually performed with the patient in a prone position, providing access to both kidneys (Fig. 18.3). In patients with systemic disease affecting the kidneys, either kidney can be biopsied to determine a diagnosis. However, care must be taken to avoid an atrophic kidney with an underlying chronic abnormality. Occasionally, a lateral decubitus or sitting position may provide better access, a safer approach, or more comfort for an obese or pregnant patient (Fig. 18.4). The lower pole of the kidney is usually selected for nontarget renal biopsy to decrease the risk of hemorrhagic complications (Fig. 18.1). Imaging immediately prior to the biopsy can help identify renal cysts and tumors; ideally, renal cysts or tumors should not be traversed to reach the renal cortex. Biopsy may be performed with or without the use of a coaxial guide needle.
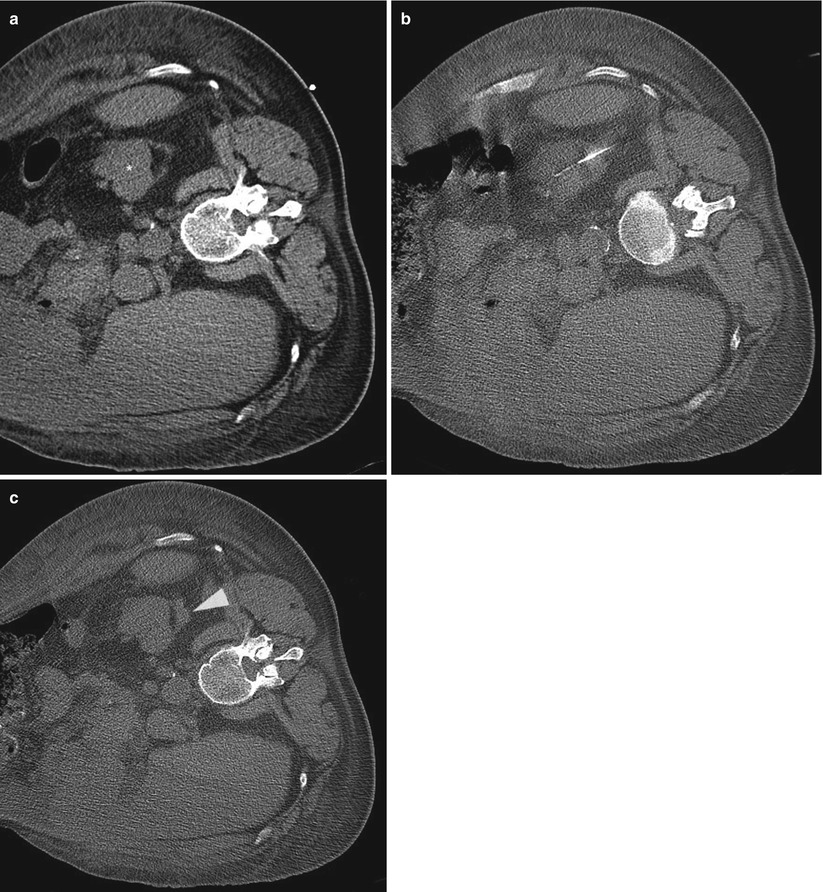
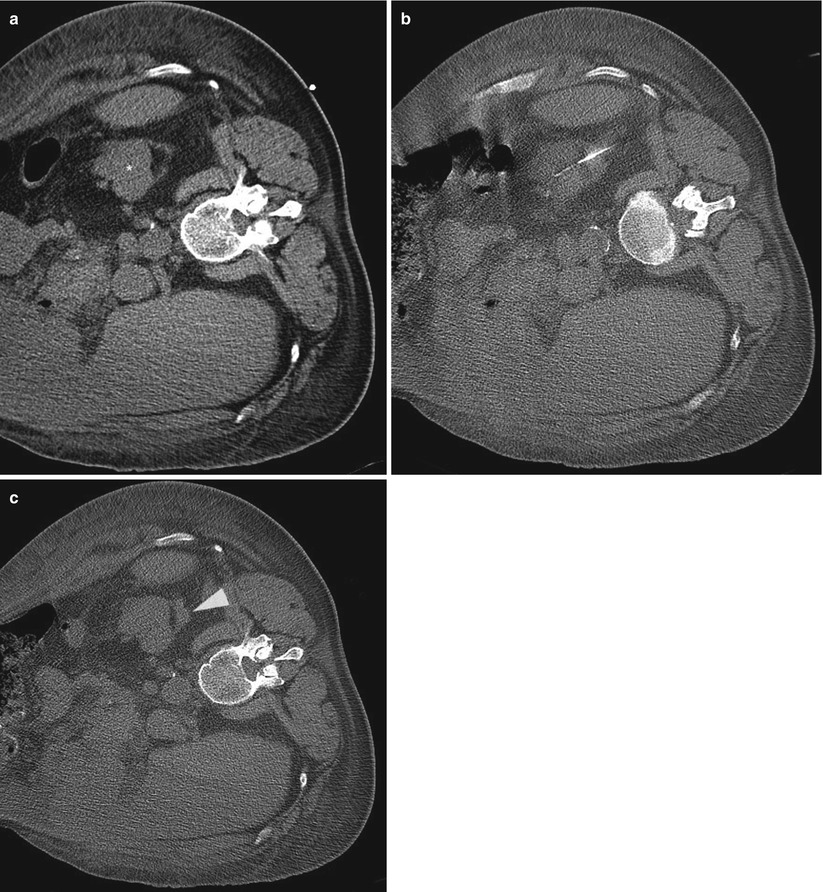
Fig. 18.4
A 62-year-old man with colon carcinoma and renal dysfunction. CT-guided renal biopsy was performed in the right decubitus position due to the patient’s body habitus. Axial CT image of the abdomen in right lateral decubitus position (a) shows the left renal parenchyma surrounded by perinephric fat. CT image during the biopsy (b) shows small perinephric hemorrhage. The hematoma (arrowhead) remained stable several minutes after removing the biopsy needle (c)
A transvenous renal biopsy has been advocated for patients who have thrombocytopenia, coagulopathy, or a solitary kidney; who are morbidly obese, in whom percutaneous biopsy has failed; or who may require simultaneous renal and hepatic or cardiac biopsy (Fig. 18.5) [39–41]. The risk of perinephric bleeding is reduced because the renal capsule is not punctured in transjugular renal biopsy. For transjugular renal biopsy, the patient is placed in a supine position on the angiography table. Ultrasonography is used to access the jugular vein. The right internal jugular vein is preferred, but either the right or left internal or external jugular vein may serve as the initial access site. Initial reports of the transjugular technique described aspiration of renal tissue through a modified Colapinto needle [38]. More recently, a spring-loaded biopsy gun with a 19-gauge side-cutting needle has produced good results [39, 41]. The renal access and biopsy set (RABS-100; Cook, Bloomington, IN) has several components: a 7-French introducer sheath with stiffening cannula, a 5-French 90-cm multipurpose catheter, and a 19-gauge 70-cm Quick-Core biopsy needle. After gaining access to the jugular vein, a 9-French introducer sheath is placed. The renal vein is selected using the multipurpose catheter. The right renal vein is preferred owing to the more favorable angle and shorter course from the inferior vena cava. A subcortical vein in the lower pole of the kidney is then selected. With the catheter pushed into the periphery of the selected vein, contrast medium is injected to opacify a wedge of renal parenchyma. Over a guidewire, the catheter is removed, and the 7-French introducer sheath with stiffening cannula is advanced to the same location. Next, the Quick-Core spring-loaded needle is inserted into the cannula. The cannula is rotated laterally and posteriorly. The needle is advanced into the renal cortex and a tissue sample is obtained. Several tissue samples can be obtained while maintaining access with the cannula. In one study, up to five tissue samples were obtained [39]. In another study, See et al. reported a modification of this technique using a long flexible 7-French sheath instead of the stiff cannula [41]. The sheath was advanced over a guidewire into the peripheral subcortical vein. In absence of the stiff metallic cannula, the needle tip must be protected by a catheter prior to insertion into the sheath. A 70-cm-long 19-gauge Quick-Core biopsy needle was loaded into a 60- or 65-cm 5-French straight catheter with the catheter covering the tip of the needle. The assembly was then loaded into the 7-French sheath and was advanced to the biopsy target area. The catheter was pulled back exposing the needle tip to obtain a tissue sample.
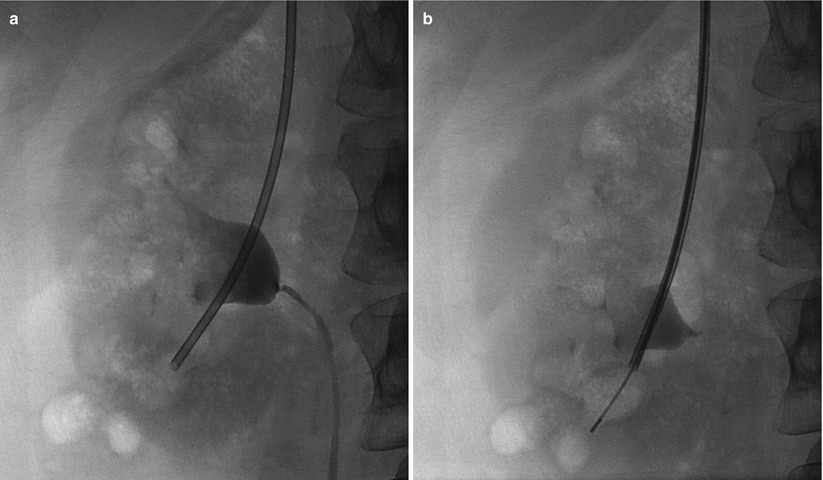
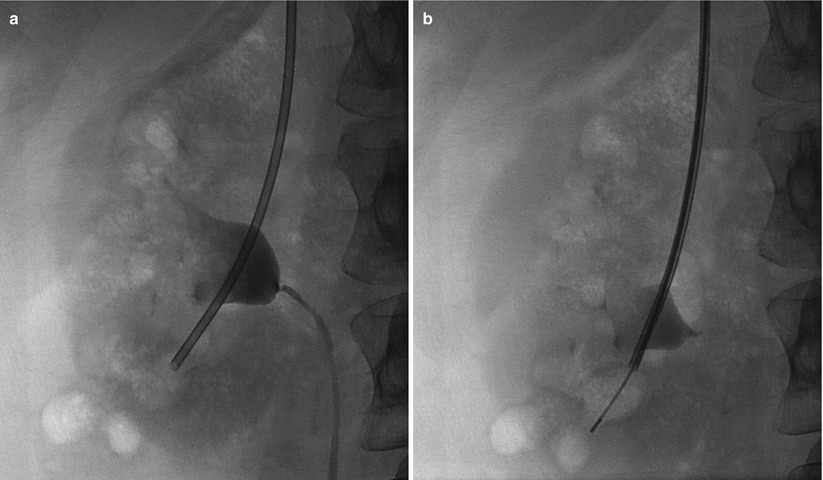
Fig. 18.5
Transjugular kidney biopsy. Fluoroscopic image of the right kidney (a) shows the introducer sheath in the lower pole of the kidney. The core biopsy needle with a blunt tip (b) is inserted into the renal cortex to obtain a biopsy sample (Images courtesy of Sanjay Misra, M.D.)
Potential Complications
Varying degrees of bleeding may be encountered after percutaneous renal biopsy [17, 18, 28, 37, 42–44] (Table 18.1). Percutaneous renal biopsy often results in perinephric hemorrhage. Generally, perinephric bleeding is slight and self-limiting and does not require therapy (Fig. 18.6). However, a retroperitoneal hematoma can enlarge rapidly and cause signs and symptoms of blood loss (Fig. 18.7). Both percutaneous and transjugular renal biopsy may also cause bleeding into the collecting system, resulting in microscopic or gross hematuria, but this form of hemorrhage is often self-limiting. Gross hematuria may result in blood clots that can cause ureteral obstruction. Persistent hematuria may be a sign of arteriovenous fistula formation. In up to 18 % of patients who underwent renal biopsy, arteriovenous fistulas were identified using color Duplex sonography [17, 45]. Although most of these arteriovenous fistulas resolve spontaneously with time [35], occasionally persistent hematuria, hypertension, or high-output heart failure may be encountered. In a transplanted kidney, arteriovenous fistula may cause renal insufficiency [45]. Finally, a subcapsular hematoma, if large enough, may exert pressure on the renal parenchyma, leading to pain and pressure. In a Page kidney, a large subcapsular hematoma exerts sufficient pressure to induce ischemia, activating the renin-angiotensin system, which can lead to chronic hypertension [46–48]. Most clinically significant bleeding complications are identified within 24 h [49]. Major risk factors for bleeding include thrombocytopenia, coagulopathy, hypertension, renal insufficiency, and anemia [28, 43, 49–51]. The risk of mortality from percutaneous renal biopsy is less than 0.1 % [28, 44, 52].
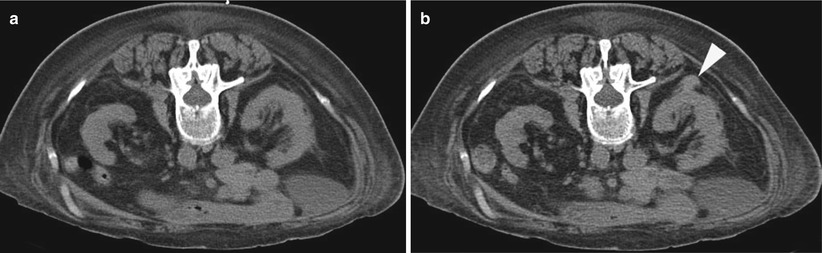
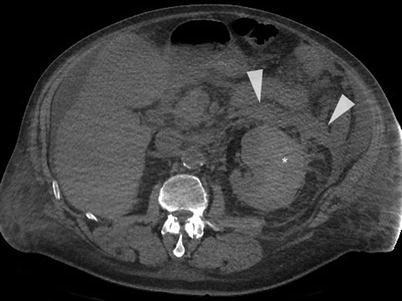
Table 18.1
Incidence of bleeding after percutaneous renal biopsy
Type of bleeding | Incidence |
|---|---|
Transient microscopic hematuria | Nearly 100 % |
Transient gross hematuria | 3–18 % |
Decrease in hemoglobin 1 g/dL or more | Nearly 50 % |
Severe bleeding causing hypotension | 1–2 % |
Severe bleeding requiring transfusion | Up to 6 % |
Surgery required to control bleeding | 0.1–0.4 % |
Severe bleeding leading to nephrectomy | Nearly 0.3 % |
Risk of mortality | 0.02–0.1 % |
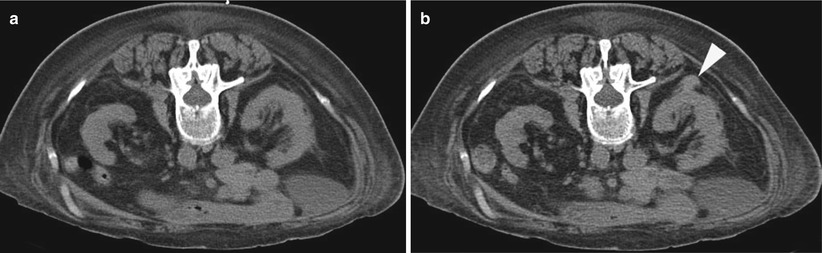
Fig. 18.6
An 82-year-old woman with toxic goiter and acute renal failure was referred for percutaneous renal biopsy. Axial CT image of the patient in prone position (a) shows small left kidney; biopsy samples were obtained from the right kidney. Immediately after the biopsy, CT image of the abdomen (b) shows a small right perinephric hematoma (arrowhead). There were no clinical consequences
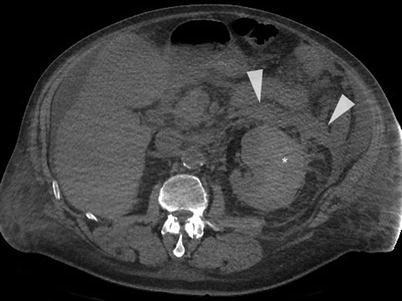
Fig. 18.7
The patient in Fig. 18.4 returned to the emergency center 3 days after the renal biopsy complaining of left flank pain. A non-contrast CT of the abdomen reveals a large retroperitoneal (arrowheads) and subcapsular hematoma. He was admitted for conservative management with transfusion of packed red blood cells
Some researchers have recommended that patients should be observed in a supine position for 4–6 h and then remain on bed rest overnight. Close to 90 % of complications are identified within 12 h after biopsy [49], and over 90 % of complications are detected within 24 h after biopsy. Determining the optimum observation time after renal biopsy requires consideration of both healthcare cost and patient safety [53]. Several studies have claimed that observation for 12 h after renal biopsy is safe and cost-effective [51, 54, 55]. In a study of 44 patients, postrenal biopsy hematuria was detected in 52 % of patients within ≤2 h, 85 % within ≤4 h, and 97.7%within ≤6 h after biopsy [55].
Management of Complications
In the past, surgery was recommended to control severe or persistent bleeding caused by percutaneous renal biopsy and may have resulted in nephrectomy in a small number of patients [56]. At the time of this writing, angiography and selective embolization is the treatment of choice in patients with life-threatening or persistent bleeding and/or symptomatic arteriovenous fistula. In most cases, selective embolization guided by angiography can easily manage the bleeding and preserve the remainder of the kidney (Fig. 18.8) [57].
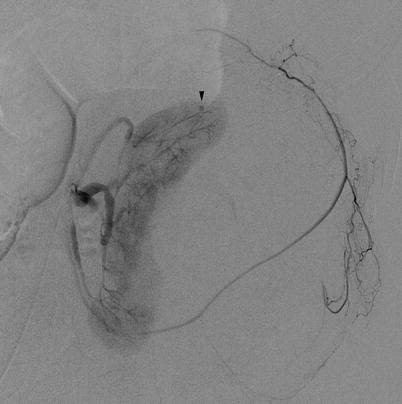
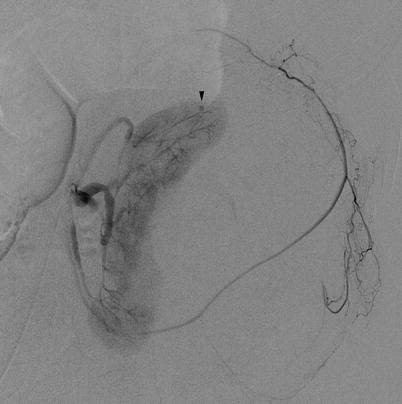
Fig. 18.8
The patient from Fig. 18.4 failed to stabilize after 3 days of conservative management and transfusion. An angiogram was performed. Diagnostic left renal angiogram in the parenchymal phase shows a small pseudoaneurysm (arrowhead) in the superior pole of the kidney, in the region of the biopsy. The arterial branch was successfully embolized with no further clinical evidence of bleeding. Note the stretching of the capsular artery and deformation of the renal parenchyma from the large subcapsular hematoma
Outcomes and Results
In cases of kidney disease, renal biopsy samples are routinely evaluated by light microscopy, immunofluorescent microscopy, and electron microscopy following optimal preservation, thin-tissue sectioning (2–3 μm thick), and use of special stains (e.g., periodic acid-Schiff, Jones’ silver, or trichome) [6, 58]. The goal is to comprehensively evaluate all components of the renal parenchyma including glomeruli, tubules, vessels, and interstitium. An adequate tissue sample is a prerequisite for successful pathologic evaluation. However, the definition of tissue adequacy varies among studies. It is almost impossible to arrive at an absolute number of glomeruli necessary to make a definitive diagnosis in every case. Some investigators believe that up to 20 glomeruli are needed for complete qualitative and quantitative evaluation of interstitial tubular and glomerular parameters [59]. Others believe that an adequate sample contains at least five glomeruli [60]. For most cases, tissue samples are considered adequate if they contain five or more glomeruli for light microscopy, two or more glomeruli for immunofluorescent microscopy, and at least one glomerulus for electron microscopy. Immunofluorescent studies require fresh tissue from a frozen sample, but the immunoperoxidase technique may be used instead to utilize tissue that was fixed in formalin [61]. When automated biopsy needles that are 18-gauge or larger are used to obtain at least two tissue samples from the kidney, adequate tissue can be obtained in the majority of cases [29–36, 62, 63] (Table 18.2). Automated 18-gauge biopsy needles that are currently used pose less risk of postbiopsy hemorrhage than by the manual 14-gauge biopsy needles used in the past [35, 60]. Riehl et al. also found that complication rates were lower in biopsies of transplanted kidneys than in biopsies of native kidneys [35].
Table 18.2
Percutaneous renal biopsy outcomes
Reference | Number of biopsies | Needle size | Number of glomeruli | Percentage diagnostic biopsy |
|---|---|---|---|---|
Wiseman et al. [29] | 24 | 14 G, 18 G | 12 per specimen | 96 % |
Doyle et al. [31] | 69 | 14 G Tru-Cut, 18 G | 21.7 per core | 96 % |
86 | 16.7 | 99 % | ||
Kim et al. [32] | 67 | 14 G Tru-Cut, 18 G | 15.3 ± 8.4 per core | 100 % |
99 | 9.95 ± 6.9 | |||
Burstein et al. [33] | 232 | 14 G Tru-Cut, | 28 ± 15 per bx | 93.5 % total |
91 | 18 G | 21 ± 13 | ||
Feneberg et al. [34] | 252 | Silverman 14 G, | 22.3 ± 14.4 per core | 95.8 %a |
568 | Tru-Cut 14 G, automated 14 G | 26.6 ± 13.1 | 95.7 % | |
262 | 32.1 ± 12.4
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|