Percutaneous Translumbar Inferior Vena Cava Cannulation and other Alternative Vascular Access Techniques
Today, cannulation of the large veins of the chest and neck is considered routine and permits reliable central venous access in virtually any patient. Long-term catheterization with subcutaneously tunneled Dacron-cuffed silicone or polyurethane catheters has seen growing popularity because of the patient comfort provided by such access systems. With proper catheter care, patients can maintain tunneled catheters for periods in excess of 1 year. Acute complications of central vein cannulation may occur but are unusual if current techniques and equipment are used. The more significant problems are associated with long-term catheterization. Chief among these are infection, venous thrombosis, and loss of future access sites.
With improvement in medical care, certain patients have emerged who require lifelong central venous access. One example would be patients who have short-gut syndrome following surgery, trauma, radiation, or gastrointestinal tract disease who require total parenteral nutrition (TPN) or hydration. Other patients who frequently have access problems are those on chronic maintenance hemodialysis. Catheter hemodialysis is not the optimum technique for renal replacement therapy1; however, the clinical reality often calls for catheter hemodialysis in patients with acute renal failure, in patients with chronic renal disease in whom the renal function is declining faster than expected, and in patients in whom a permanent arteriovenous (AV) shunt has not had time to mature. This step is taken to treat sepsis at least temporarily in patients with established vascular or peritoneal access and for revision of AV grafts and fistulae. Failure to tolerate either a native AV fistula or a polytetrafluoroethylene (PTFE) graft is another reason for long-term catheter hemodialysis.
The right internal jugular vein is the standard access route because it is less likely to lead to future venous stenosis.2,3 The subclavian vein and the external jugular vein have been largely abandoned as catheter access routes for the same reason. These patients are at high risk for vessel occlusion, the former because of the irritating nature of the TPN solution and the latter because of the large-diameter catheters required to sustain the flow needed for effective hemodialysis. Occlusion of the central veins of the chest and neck also may follow surgery, radiation therapy, congenital abnormalities, or infection or may be seen in patients with hypercoagulable states. Maintenance of an adequate vascular access becomes an important factor in the success of management of these patients.
To help care for the patient with access problems, alternative techniques to subclavian and jugular cannulation have been developed. The purpose of this chapter is to review these options. Potential solutions include the following:
1. Surgical techniques
a. Exposure of the deep veins in the chest
b. Creation of an arteriovenous fistula (AVF)
c. inferior vena cava (IVC) placement via infraumbilical veins
2. Percutaneous techniques
a. Recanalization of obstructions
b. Collateral pathways around obstructions
c. IVC placement, infraumbilical access
d. IVC placement, translumbar access
e. IVC placement, transhepatic access
f. Right atrium (RA) placement, transhepatic venous access
 Surgical Techniques
Surgical Techniques
Right Atrium, Superior Vena Cava, or Azygos Vein Cannulation
Reports in the literature describe the successful use of these sites for catheterization. Established surgical options for venous access through thoracotomy include direct catheter placement into the RA,4 azygos vein5–7 or superior vena cava (SVC).7 Obviously, these are techniques of last resort. Thoracotomy is required and catheter removal is not straightforward. Patients who have had previous thoracotomies or reduced cardiopulmonary reserve are at higher risk from complications of thoracotomy.
Recent improvements in technique allow placement into these vessels using minimally invasive surgery by thoracoscopy.8,9 The azygos vein, hemiazygos vein, and SVC are also accessible by cannulation of an intercostal vein.6,10–12 This has been done surgically through open exposure of the intercostal vein11,13 or by percutaneous puncture of an intercostal vein10 and combined with radiologic recanalization of occlusions or the use of retrieval baskets to guide the catheter to its final position.6,12 Direct percutaneous puncture of the hemiazygos vein with placement of a Broviac catheter has been reported.14 With the development of techniques for inferior vena cava (IVC) catheter placement and, in particular, the successful use of the translumbar percutaneous catheter techniques, the need for surgical placement of catheters into the azygos vein or RA has been reduced.
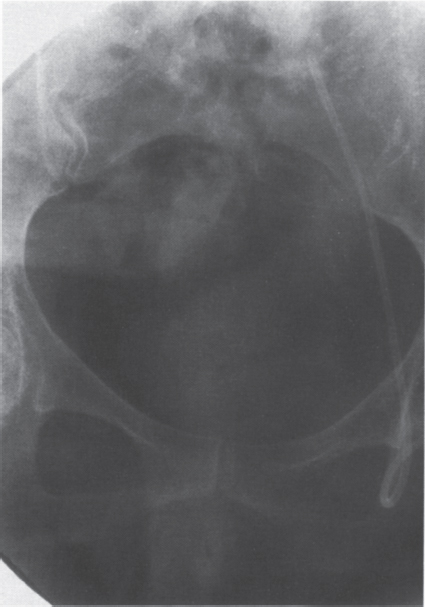
FIGURE 27–1. Single-lumen infusion through the inferior epigastric vein.
Surgical Creation of Arteriovenous Fistula
The concept of creating a native arteriovenous fistula (AVF) or prosthetic graft to allow repeated long-term vascular access has been tested successfully for both TPN15 and chemotherapy.16 Pseudoaneurysms, infection, and thrombosis eventually will lead to the loss of these accesses. Also, an extremity AW will function properly only if there is unimpeded venous outflow. Therefore, this strategy is unlikely to be successful in a patient already in need of alternative vascular access.
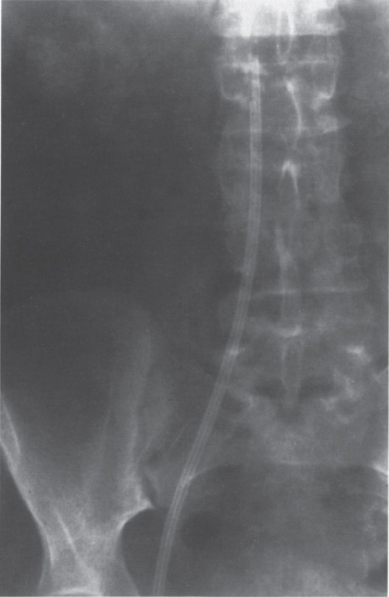
FIGURE 27–2. Double-lumen hemodialysis catheter placed through the right common femoral vein.
Surgical IVC Placement through Infraumbilical Veins
All these techniques take advantage of placing the catheter tip in the large-caliber, high-flow environment of the IVC using the saphenous,11,17–23 femoral,19,24–39 inferior epigastric,40–43 iliac,44 gonadal,19,45,46 or lumbar veins47 for initial catheter entry. The inferior epigastric (Fig. 27–1), femoral (Fig. 27–2), and saphenous (Fig. 27–3) approaches share the disadvantage of the catheter traversing the iliac venous systems. Some reports in the literature state that long-term complications from this catheterization technique are equivalent to subclavian and jugular catheter placement.19 Others disagree with this statement and claim an increased risk of venous thrombosis (Fig. 27–4) as well as a higher rate of infection. Also, many patients will object to placement of long-term catheters in the groin.
Surgical isolation and cannulation of the gonadal veins and subsequent placement of the catheter tip in the IVC are relatively new techniques19 (Fig. 27–5). Three cases were reported by Williard et al,19 and their experience was that these catheters function as well as catheters placed through the saphenous and epigastric venous system. Indeed, Po et al46 mentioned having placed a hemodialysis catheter through the left gonadal vein into the IVC.
All these techniques require fluoroscopic observation during advancement of the catheter; otherwise, the catheter tip may not find its way to the IVC and may end up in small venous tributaries (Fig. 27–6). One case was reported in which the IVC was surgically exposed and a Hickman catheter placed just inside the IVC through a venotomy of a lumbar vein and secured with a purse-string suture.47 The report states that the catheter function was uncomplicated. The importance of this case report is that it introduced the concept of translumbar access to the IVC for catheter placement.
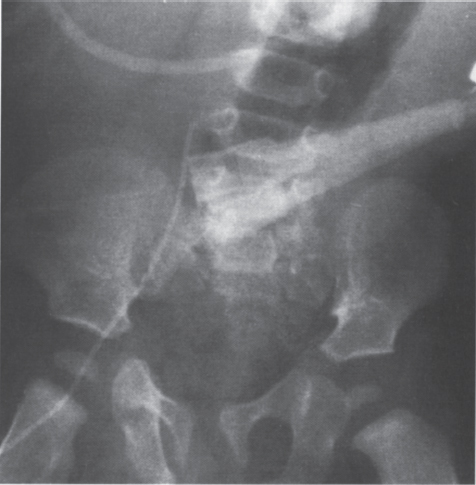
FIGURE 27–3. Infusion catheter placed through the right saphenous vein in a child.

FIGURE 27–4. Acute superficial femoral vein thrombosis following placement of inferior epigastric infusion catheter (same patient as Fig. 27–1).
 Percutaneous Techniques
Percutaneous Techniques
Recanalization of Venous Occlusions
Central venous catheters can be placed across a chronic occlusion after the occlusion has been traversed with a guidewire or catheter.12,48 Steerable guidewires and hydrophilic coatings along with high-quality digital imaging systems are invaluable for this purpose. Even sharp-needle recanalization of occlusions has been described.49 The through-and-through guidewire technique may be needed to provide a mechanical advantage for advancing catheters and sheaths across the obstruction. Intravascular snares or retrieval baskets have been used to grab the tip of catheters or wires, pulling them across the obstruction.12 The concerns about a dislodging clot or occluding collaterals have not proven to be significant in actual practice.

FIGURE 27–5. Single lumen infusion catheter placed through the right gonadal vein.
Catheter Placement via Collateral Channels
It is possible to follow collateral vessels around an obstruction and to reenter a more central part of the vein.50,51 Again, these techniques require high-quality imaging equipment and familiarity with catheter and guidewire technology.
Percutaneous Infraumbilical IVC Catheters
The previous comments regarding surgically placed infraumbilical access catheters apply equally to percutaneous placement. In everyday clinical practice, this access is limited to femoral vein catheters for hemodialysis, although as mentioned, any vein that leads to the IVC can be cannulated.
For a long time, the femoral vein access was used successfully for acute dialysis. In general, the patient is bedridden; in this clinical situation, patient mobility is of less concern, and nursing care can help prevent infection. The ambulatory patient frequently does not tolerate a femoral catheter, even when tunneled. If future renal transplantation or lower-extremity AV shunt access is a possibility, a femoral catheter should be avoided because of concerns about iliofemoral stenosis or thrombosis.
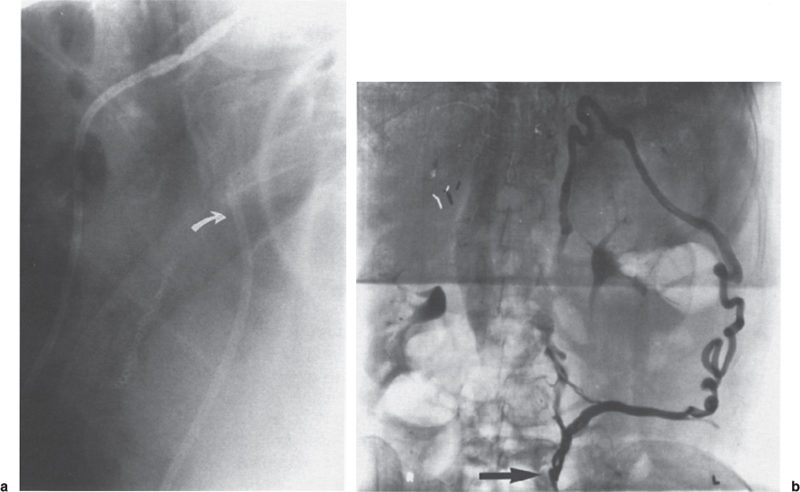
FIGURE 27–6. (a) Lateral view of the infusion catheter placed through an inferior epigastric artery (same patient as Fig. 27–1). Catheter tip (arrow) located posteriorly. (b) Catheter tip not in the inferior vena cava but located in paraspinal tributary. Large collateral vessel opacified.
Translumbar Cannulation of the IVC
This technique was first reported by Kenney et al52 and used for TPN administration in an adult.52 The catheter remained in place for 11 months. It was removed because of suspected catheter sepsis. The same group subsequently reported more patients, including use of an IVC catheter in a child.53,54 Further experience with these catheters was reported by Robards et al,55 who placed an infusion catheter in a 2-year-old child. Subsequently, the same group56 reported a larger series of pediatric inferior vena cava catheters. Lund et al57 demonstrated the safety of placing and removing large (14F) catheters. Computed tomography (CT) scans performed both after catheter placement and after catheter removal showed a normal appearance of the retroperitoneum without hemorrhage, supporting the clinical observations of other groups that these catheters are remarkably free of placement complications. A CT study by Cazenave et al58 analyzed the best translumbar route for avoiding complications from puncture of nearby organs.58 A large series of 230 IVC catheters were reported in abstract form by McCowan et al.59 Further development of this technique was reported by Lund et al,60 who placed dedicated double-lumen, large-caliber hemodialysis and apheresis catheters. Reported uses of the translumbar technique include apheresis and hemodialysis,60–65 parenteral nutrition,53,54,56,66 chemotherapy,53,66 use in children,53,55,56,67,68 placement of a LeVeen shunt,69 and for implantation of access ports.66
Placement Technique
The placement of an IVC catheter is basically an extension of the translumbar aortography technique. The procedure has four stages:
1. Localization of the IVC
2. Puncture and cannulation of the IVC
3. Catheter tunneling
4. Tract dilatation and catheter placement
Localization of the IVC. The IVC can be approached by using simple fluoroscopic localization and bone landmarks in a technique similar to translumbar aortography.
The IVC can be opacified using a small angiographic catheter placed via the femoral vein. In patients with IVC filters in place (Fig. 27–7) or when there is a question of anomalies (Fig. 27–8), occlusions, or compression, angiographic evaluation of the IVC for patency is mandatory. Radiopaque instruments such as guidewires, catheters, wire baskets, or intravascular snares could be placed through the femoral vein to serve as stationary targets during the puncture (Fig. 27–9).
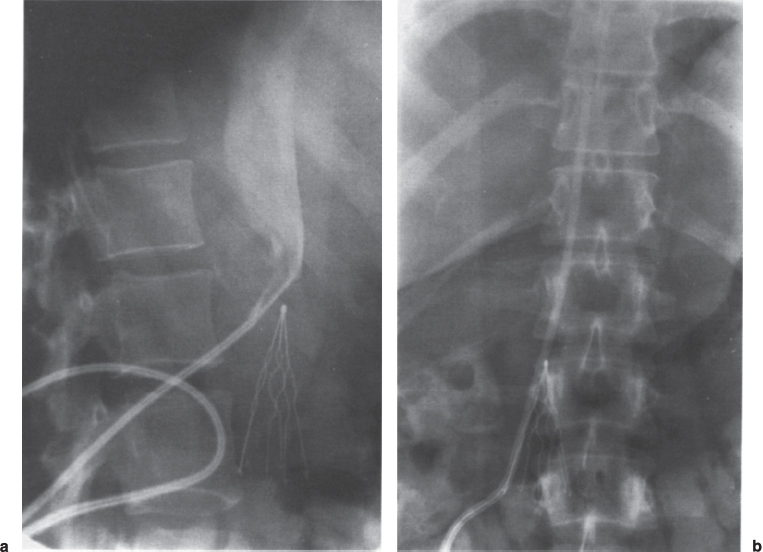
FIGURE 27–7. (a) Lateral view confirms the patency of the inferior vena cava before placement of infusion catheter in this patient with preexisting Greenfield IVC filter and no other venous access. (b) Anteroposterior view of course of inferior vena cava catheter in this patient.
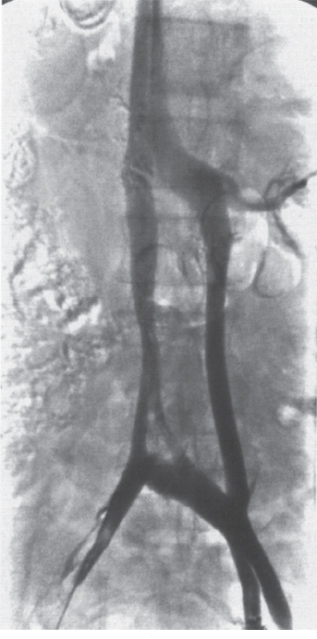
FIGURE 27–8. Intravenous cholangiogram shows duplication of inferior vena cava in this patient referred for IVC catheter placement.
In infants and small children, ultrasound has been used for localization. Alternatively, the initial puncture could be performed with CT guidance.
Puncture. An initial skin incision is made using local anesthesia just above the iliac crest 3 to 4 inches from the midline (see Fig. 27–9). Cazenave et al58
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree