, Giulia Bella and Valeria Buonocore
(1)
Radiologic, Oncologic and Anatomopathologic Sciences, Policlinico Umberto I, Rome, Italy
Abstract
Perianal fistulas are a relatively frequent gastrointestinal pathology and an important cause of morbidity. They are particularly common in patients with Crohn’s disease, who develop this complication in approximately 50% of cases [1,2]. Fistulas frequently arise from the obstruction and infection of the anal crypts, in which the glands of Hermann and Desfosses flow, by feces, foreign bodies, or small local traumas. The fistulas may then spread towards the skin, within the rectal wall, or through the external sphincter towards the ischiorectal fossa.
Perianal fistulas are a relatively frequent gastrointestinal pathology and an important cause of morbidity. They are particularly common in patients with Crohn’s disease, who develop this complication in approximately 50% of cases [1,2]. Fistulas frequently arise from the obstruction and infection of the anal crypts, in which the glands of Hermann and Desfosses flow, by feces, foreign bodies, or small local traumas. The fistulas may then spread towards the skin, within the rectal wall, or through the external sphincter towards the ischiorectal fossa.
20.1 Surgical Classifications of Anal/Perianal Fistulas
By definition, a fistula is an abnormal tract that connects two epithelial surfaces. The anatomic course of an anal fistula will be dictated by the location of the infected anal gland and the anatomic planes and boundaries that surround it. The radial positions of the fistula around the anus are referenced to a clock face, in which, according to the radiological classification, the 12 o’clock and 6 o’clock positions are, respectively, anteriorly and posteriorly directed [3].
Usually, the internal opening in the anal canal is located at the level of the dentate line, which is at the original site of the duct draining the infected gland. In most cases, this is located at the 6 o’clock position because the anal glands are more abundant posteriorly [4]. The fistula can reach the perianal skin by a variety of routes, some more tortuous than others, usually by variably penetrating and involving the muscles of the anal sphincter and surrounding tissues. Fistulas should be classified according to the route taken by the “primary tract” linking the internal and external openings.
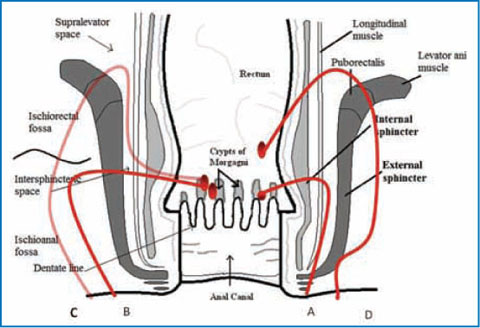
In 1934, Milligan and Morgan introduced the first classification of fistulas- in-ano based on the relationships between the tracts and the anorectal ring (anatomically, the puborectalis muscle). According to this early classification, anal fistulas were situated below the level of the ring whereas the anorectal type extended, at least partly, above the ring [5]. While this classification was subsequently modified and refined by other authors, the most comprehensive and practical classification, still in use today, is that of Parks et al., which is based on surgical findings [6]. Considering the external sphincter as the keystone, fistulas are classified into four main types and subtypes (Table 20.1, Fig. 20.1).
Type 1 fistulas (intersphincteric) (Figs. 20.1, 20.2) ramify only in the intersphincteric plane. This is the most common type and is sometimes known as the “low anal” fistula. It may be further subdivided into:
Simple intersphincteric fistula (Fig. 20.3). In this variety, the most common one, a tract passes from the primary abscess in the intersphincteric plane straight downwards to the anal verge.
Intersphincteric fistula with a high blind tract. A is a high extension of the fistula between the internal sphincter and the longitudinal muscle of the upper anal canal passes upwards into the rectal wall itself.
Intersphincteric fistula with a high tract opening into the lower rectum.
High intersphincteric fistula without a perineal opening. The fistula commences in the intersphincteric zone of the mid-anal canal and passes upwards to end blindly in the rectal wall or to re-enter the rectum.
High intersphincteric fistula with a pelvic extension. The tract passes upwards out into the pararectal space, instead of restricting its course to the rectal wall. There may or may not be a perineal opening.
Intersphincteric fistula from pelvic disease. An infection from the pelvis can track downwards and reach the anal margin. In either case it pursues an intersphincteric course or it the may be extrasphincteric. This type is not a pure anal fistula at all, as its origin is completely outside defined area.
Subcutaneous | No relation with the anal sphincter complex |
Intersphincteric | Within the intersphincteric region, between the internal and |
external sphincters | |
Transsphincteric | Extends through both the internal and the external sphincter |
Suprasphincteric | From the skin surface to the ischiorectal fossa, without |
communicating with the anal sphincter | |
Translevator | Above the levator ani muscle, within the pelvic region |
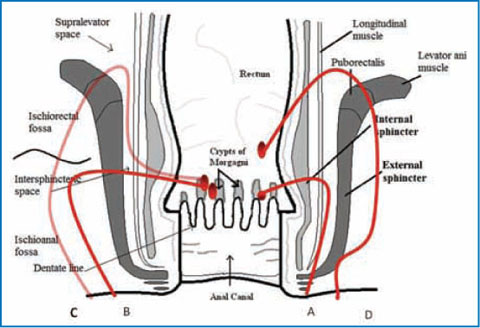
Fig. 20.1
The Parks classification of anal/perianal fistulas. A Intersphincteric fistula, B transsphincteric fistula, C suprasphincteric fistula, D extrasphincteric (translevator) fistula
In type 2 fistulas (transsphincteric) (Figs. 20.4, 20.5) the tract passes from the intersphincteric plane through the external sphincter complex at varying levels into the ischiorectal fossa. Two subtypes are recognized:
In uncomplicated cases, the tract passes from the intersphincteric plane of the mid-anal canal, through the external sphincter into the ischiorectal fossa and thence directly to the skin.
In a transsphincteric fistula with a high blind tract, the tract crosses the external sphincter as previously described but then divides into two, giving rise to lower and upper halves. The lower tract passes to the perineal skin but the upper tract may reach the apex of the ischiorectal fossa or even higher, passing through the levator ani muscles into the true pelvic cavity.
In type 3 fistulas (suprasphincteric) (Fig. 20.6) the tract passes in the intersphincteric plane over the top of the puborectalis, then downwards again into the ischiorectal fossa and finally to the skin.
In type 4 fistulas (extrasphincteric) a tract passes from the perineal skin through the ischiorectal fat and levator muscles into the rectum (Fig. 20.7). This type is outside the external sphincter complex altogether. The following subtypes are recognized:

In those secondary to a transsphincteric fistula, the tract from the latter passes upwards through the levator muscles to re-enter the rectum.
In extrasphincteric fistulas due to trauma, there is direct communication between the rectum and the perineum.
Extrasphincteric fistulas may also be due to a specific anorectal disease (inflammatory bowel disease or carcinoma).
Alternatively, anextrasphincteric fistula may be due to pelvic inflammation, in which case an infection spreads downwards through the pelvic tissue, breaking through the levator ani muscles and emerging in the perineum.
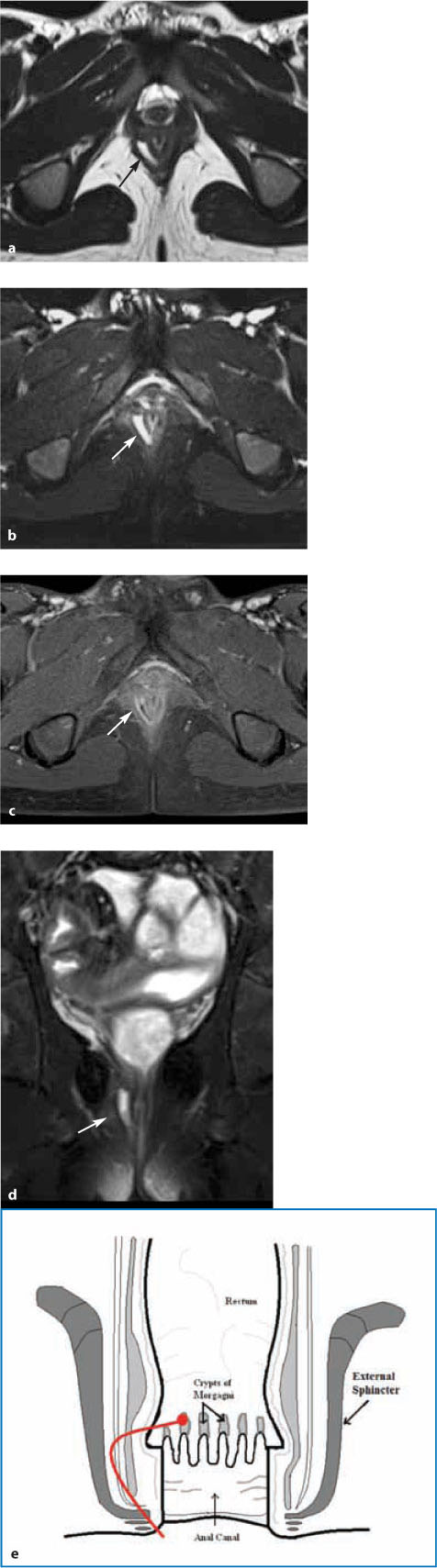
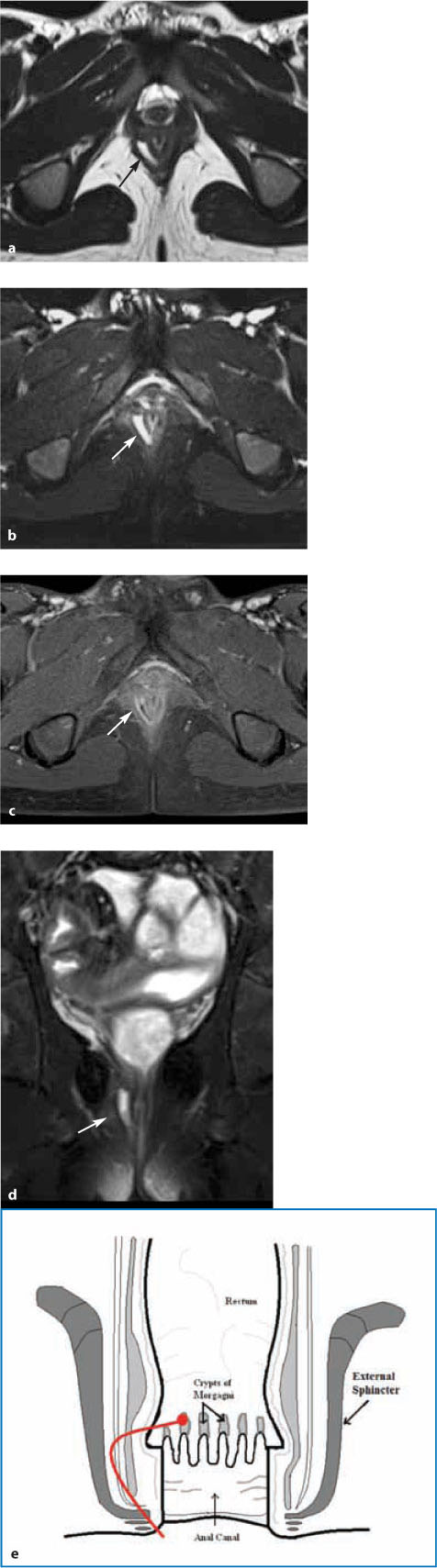
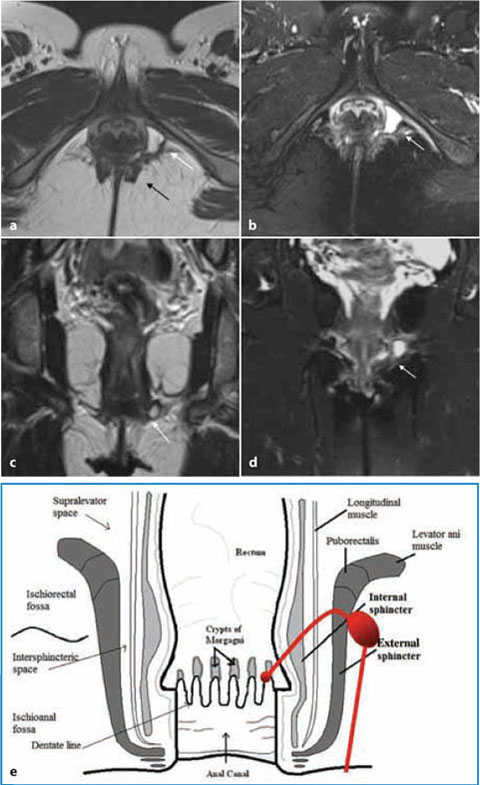
Fig. 20.2
Intersphincteric fistula, grade 1 according to St James University Hospital (SJUH) classification (Parks type I). a Axial high-resolution T2-weighted turbo spin echo image shows a linear hyperintensity in the intersphincteric right space (arrow). b On the axial highresolution T2-weighted fat- suppressed image, the focal hyperintensity in the intersphincteric left space is more clearly detected (arrow). c The axial T1-weighted turbo spin echo fat-suppressed image acquired after Gd IV injection shows an enhancing focal lesion corresponding to an intersphincteric fistula. d Coronal T2-weighted fat-suppressed image showing the intersphincteric tract (arrow). e Scheme of a grade 1 fistula according to the SJUH classification (Parks type I) (cont.

Fig. 20.3
Intersphincteric fistula with a small intersphincteric abscess, grade 2 according to St James University Hospital (SJUH) classification (Parks type I). a Axial high-resolution T2 sequence showing a thin intersphincteric posterior horseshoe tract, associated to a small left intersphincteric abscess at three o’clock (arrow). b Scheme of a grade 2 fistula according to the SJUH classification (Parks type I)
20.2 Radiological and Clinical Classification of Perianal Fistulas
Since relevant MRI findings are not included in the Parks classification, an MRI-based classification was proposed that relates the Parks surgical classification to anatomic MRI findings in the axial and coronal planes. The St James’ University Hospital classification was proposed by radiologists on the basis of imaging findings and does not represent an official surgical reference. In fact, in the evaluation of perianal fistulas radiologists are expected to be descriptive and accurate in their reports, as the details of the information they provide will be essential in future decisions regarding medical or surgical treatment [7,8].
Unlike the Parks classification, that of St James takes into consideration the secondary tracts and abscesses, as well as the primary tract [9]. Since secondary tracts can be missed by clinical examination, preoperative MRI has emerged to better define the fistula anatomy, select the surgical approach, and thereby avoid recurrence [10–13]. All perianal fistulas are divided into five subtypes (Table 20.2). Suprasphincteric and extrasphincteric fistulas are placed in the same category as grade V (supralevator disease). A grade 1 fistula is a simple linear intersphincteric fistula (Fig. 20.2) that travels in the intersphincteric space (not disturbing the external sphincter or the ischioanal fossa) and ends at the skin of the perineum or natal cleft. No extensions or abscesses are found in the intersphincteric space or in the ischiorectal and ischioanal fossae. Unlike simple fistulas, a grade 2 fistula is intersphincteric, with an abscess or secondary tracts (Fig. 20.3) that are also confined within the intersphincteric space. Secondary tracts of grade 2 fistulas may be of the horseshoe type (lying horizontally and crossing the midline) or they may be on the ipsilateral side of the intersphincteric space. A grade 3 fistula is transsphincteric, penetrating both layers of the sphincter complex and directed toward the skin, running through the ischioanal fossa (Fig. 20.4). This type of fistula is of high risk of causing anal incontinence because during surgery the external sphincter must be excised when the tract is opened. In a grade 4 fistula (transsphincteric fistula with abscess or secondary tract), the ischioanal fossa harbors an abscess and/or secondary tract, as well as the primary tract (Fig. 20.5). Suprasphincteric and extrasphincteric fistulas are grade 5 (Figs. 20.6, 20.7).




Grade 0: | Normal aspect |
Grade 1: | Simple linear intersphincteric fistula |
Grade 2: | Complex intersphincteric fistula with abscess or secondary tract (horseshoe fistula) |
Grade 3: | Transsphincteric fistula |
Grade 4: | Transsphincteric fistula with abscess or secondary tract within the ischioanal or ischiorectal fossa |
Grade 5: | Suprasphincteric and translevator fistulas |
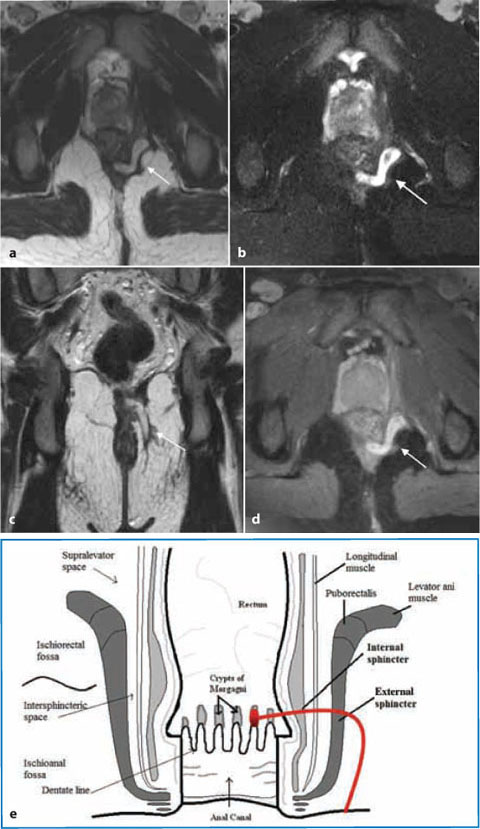
Fig. 20.4
Transsphincteric fistula grade 3 according to the St James University Hospital (SJUH) classification (Parks type II). a Axial high-resolution T2 sequence fat-suppressed showing a tubular hyperintense fluid collection (arrow) in the posterior anal region (at five-six o’clock) extending through the external sphincter into the ischioanal left fossa. b The hyperintense tract filled with fluid is more clearly detected on the axial high-resolution fat-suppressed T2 weighted image, (arrow). c Coronal high-resolution T2 sequence showing the tubular hyperintense tract extending through the external sphincter into the left ischioanal fossa (arrow). d Axial T1 turbo spin echo fat-suppressed image acquired after Gd IV injection: in the same area shows an enhancing transsphincteric fistula (arrow) (grade 3 SJUH). e Grade 3 fistula (arrow) according to the SJUH classification (Parks type II)
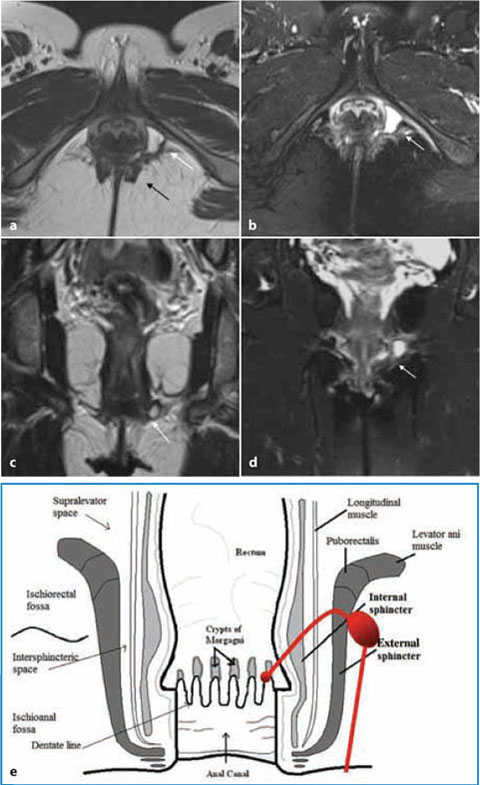
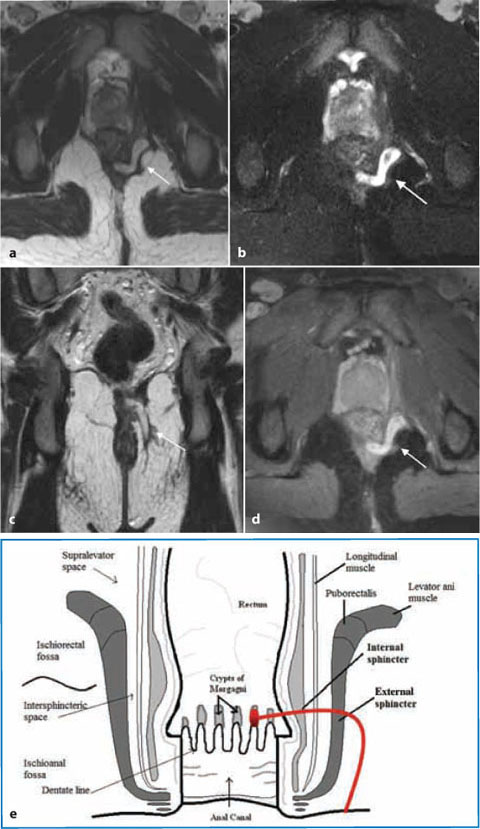
Fig. 20.5
Transsphincteric fistula complicated by an abscess, classified as grade 4 St James University Hospital (SJUH) system (Parks type II). a, b High-resolution T2 weighted plain (a) and fat-suppressed (b) axial images show a linear transsphincteric hyperintense left fistula (black arrow) extending into the ischioanal left fossa and complicated by an abscess (white arrow). c,d Coronal T2-weighted Hire BEST plain (c) and fat-suppressed (d) images show a transsphincteric abscess. e Scheme of a grade 4 fistula according to the SJUH classification (Parks type II)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree