Robert A. Morgan, Anna-Maria Belli, Joo-Young Chun
Peripheral Vascular Disease Intervention
Since the first edition of this textbook, vascular radiology has changed beyond recognition. It was only 30 years ago that the role of radiology in the vascular system was mainly to provide diagnostic images using invasive angiography. Since the development of interventional techniques in the late 1980s, interventional radiologists have assumed a major role not only in the diagnosis of vascular disorders but also in their treatment.
The other main advance in vascular radiology has been the development of non-invasive imaging such as duplex ultrasound, multidetector computed tomographic angiography (MDCTA) and magnetic resonance angiography (MRA). The current range of diagnostic and interventional techniques is too extensive to be described fully in a general textbook of radiology. The aim of this chapter is to provide a brief overview of salient features of diagnostic angiography and to describe the role of the main interventional techniques in the vascular system. A description of non-invasive angiographic imaging is described in Chapter 84 and a discussion of aortic and renal arterial disease is covered in Chapter 85 and Chapter 90.
Interventional Radiology Techniques
The following are brief descriptions of the main therapeutic procedures used by vascular interventional radiologists.
Angioplasty
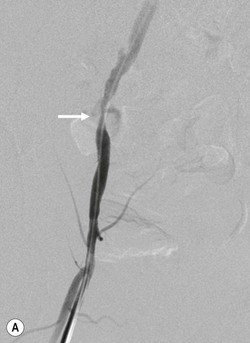
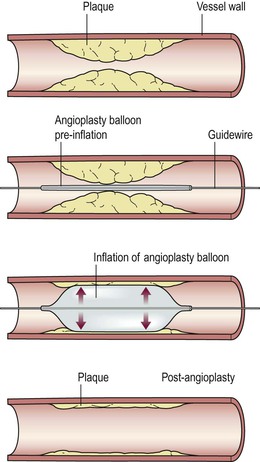
Percutaneous transluminal angioplasty (PTA) refers to treatment of a vascular stenosis or occlusion with a balloon catheter, which is introduced into the blood vessel and advanced to the site of the lesion. The balloon is inflated for a short period of time. After deflating the balloon, a check angiogram is performed to assess the success of the procedure (Fig. 86-1).
Stenting
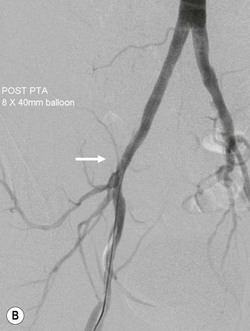
This refers to the placement of a metallic mesh tube across a vascular stenosis or occlusion. There are two main types of stent: balloon expandable stents are mounted on a balloon catheter and deployed by inflating the balloon; self-expanding stents are compressed on a delivery catheter and released by withdrawing an outer sheath, allowing them to expand by their own radial force (Fig. 86-2).
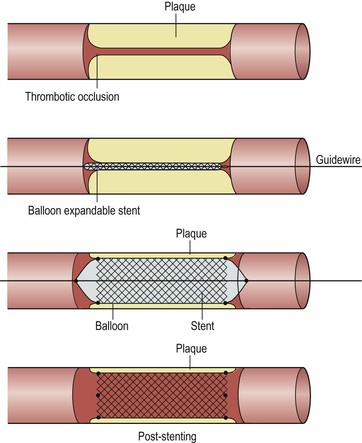
Stents may be used as the primary method of treatment or may be reserved for use if PTA is unsuccessful, depending on the location and type of lesion.
Embolisation
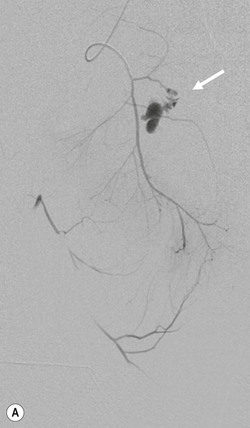
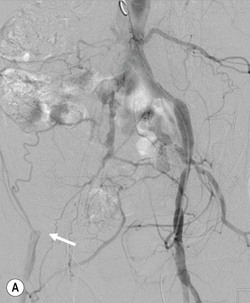
Embolisation refers to the occlusion of a blood vessel by delivery of embolic material through a catheter. Embolisation has a wide range of applications, including the treatment of haemorrhage, aneurysms, vascular malformations and the treatment and palliation of cancer, particularly primary and secondary hepatic malignancy.
There are a large variety of embolic agents, including metallic springs (coils), particulate matter, gelatin sponge, glue and liquids such as absolute alcohol. The choice depends on the anatomical site, the nature of the lesion and the personal preference of the operator.
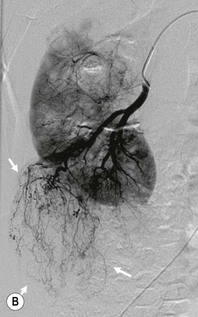
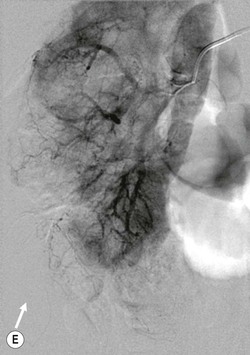
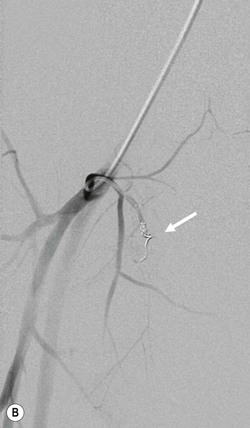
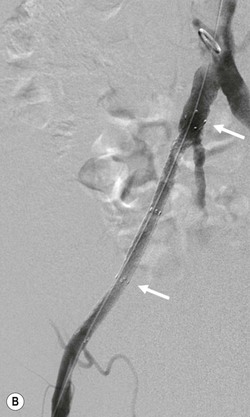
Some embolic agents, such as gelatin sponge, are considered temporary, and can be used to control haemorrhage when recanalisation of the parent vessel may be desirable once the ‘acute’ lesion has healed, e.g. traumatic injury to the internal iliac artery following pelvic trauma. Permanent particulate emboli are made from various agents, but polyvinyl alcohol (PVA) is the best known example. These agents are not radio-opaque and must be suspended in contrast medium. They cause occlusion by ‘silting up’ the blood supply. The level of occlusion depends on the size and type of particles chosen. Particulate emboli are used in the treatment of benign and malignant tumours, such as uterine leiomyoma and renal angiomyolipoma (Fig. 86-3). They may be used in combination with chemotherapeutic agents (drug-eluting beads) in hepatic chemoembolisation. Coils are used in situations analogous to tying of a vessel surgically, but knowledge of vascular anatomy is important for avoiding retrograde filling of a lesion from collateral vessels. They are used widely in the embolisation of haemorrhage (Fig. 86-4) and the exclusion of aneurysms and pseudoaneurysms.
Liquid embolic agents include sclerosants such as absolute alcohol, sodium tetradecyl sulphate (STD), glue (e.g. n-butyl-2-cyanoacylate) and newer agents such as Onyx. Sclerosants are useful in venous embolisation, e.g. varicoceles and low-flow vascular malformations. Glue and Onyx are particularly useful in dealing with high-flow arteriovenous malformations and visceral artery aneurysms.
Thrombolysis
This refers to the dissolution of blood clots within an artery or vein by the injection or infusion of a thrombolytic (clot-dissolving) drug directly into the thrombus through a catheter, which has been advanced directly into the thrombus. Although successful thrombolysis may be achieved within a short time, it is not uncommon for the lytic agent to be infused over 24–48 h. Patients undergo periodic check angiography to assess the progress of the treatment. In most cases, successful clearance of the thrombus reveals an underlying causative lesion, which should be treated by angioplasty or stenting during the same procedure. Thrombolysis was a very popular technique for the treatment of acute lower limb ischaemia about 10–15 years ago. It is less often used now but it is still performed in selected cases.
Arterial System
Pelvic and Lower Extremity Arteries
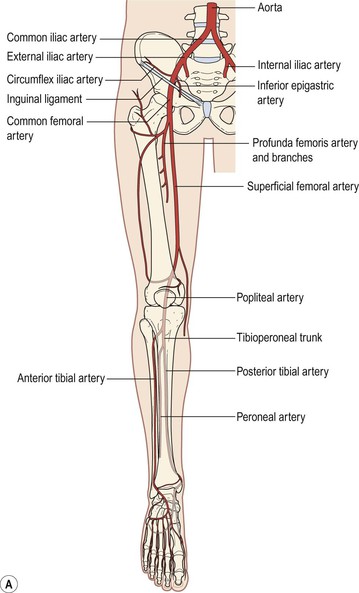
Angiographic Anatomy (Fig. 86-5)
At the level of L4, the aorta divides into the common iliac arteries, which pass in front of the iliac veins and give off no major branches. At the level of the mid sacrum, they divide into the external and internal iliac arteries. The internal iliac arteries supply the pelvis and surrounding musculature. They divide into anterior divisions, which supply the viscera, and posterior divisions, which mainly supply the musculature. The external iliac artery has no major branches, although it gives rise to the inferior epigastric artery at the junction with the common femoral artery. At the level of the inguinal ligament, the external iliac artery becomes the common femoral artery—a short vessel that gives rise to the profunda femoris (or deep femoral artery), which supplies the muscles of the thigh; and the superficial femoral artery (SFA), which has no major branches and passes distally. At the level of the adductor canal, the SFA becomes the popliteal artery, which gives rise to the vessels of the calf, which are the anterior and posterior tibial arteries and the peroneal artery. At the level of the ankle, the anterior tibial artery becomes the dorsalis pedis artery and the posterior tibial artery becomes the medial and lateral plantar arteries. The anterior tibial artery is the most lateral calf vessel, whereas the posterior tibial artery is the most medial. In the forefoot, the plantar arch is formed by the lateral plantar branch of the posterior tibial artery and the dorsalis pedis artery. Anatomical variations of the lower extremity arteries are outside the scope of this chapter.
Arterial Disease Affecting the Lower Extremity
The most common condition affecting the arteries of the lower extremity is tissue ischaemia due to occlusive disease. Occlusive disease may be acute, acute-on-chronic (where acute occlusion occurs in the presence of a previous chronic stenosis or occlusion) or chronic occlusion. Most patients present with symptoms of chronic occlusive disease, usually caused by atherosclerosis. Less common causes include thromboembolism, acute thrombotic occlusion, microembolism, entrapment syndromes, cystic adventitial disease, trauma and vasculitis, including vasospastic disorders and Buerger’s disease.
The clinical presentation varies, depending on the type, location and number of the arterial lesions. Patients may be asymptomatic, may suffer from pain on walking (intermittent claudication), pain while at rest, or tissue loss in the form of either ulceration or gangrene. In general, patients with intermittent claudication are not treated with invasive procedures unless their claudication distance is very short or their symptoms substantially limit their lifestyle. Patients with rest pain and tissue loss are at risk of limb loss and must be treated by angioplasty, stenting or surgery.
Angiographic Diagnosis
Most pathological processes affecting the lower extremity arteries cause stenosis, occlusion or dilatation, i.e. aneurysm formation. Atherosclerosis may affect the arteries at any level, from the iliac arteries to the small vessels of the foot. While it is true that a stenosis or occlusion is almost always due to atherosclerosis, it is important to consider other possible causes. The clinical history may often be of help in this respect. For example, a patient who develops acute severe pain in the lower leg with no previous history or symptoms has probably sustained an acute embolus in the femoral or popliteal arteries, rather than a long-standing atherosclerotic occlusion. Patients with diabetes develop arterial occlusive disease, which involves mainly the distal vessels of the calf and feet. Patients with a history of radiotherapy to the pelvis for the treatment of carcinoma of the cervix may develop occlusive lesions of the common and external iliac arteries due to ischaemic vasculitis induced by the radiation.
Treatment of Chronic Limb Ischaemia
Iliac Artery Disease
Stenosis.
In the treatment of stenotic lesions, PTA has a technical success rate approximating 100% (Fig. 86-6). Stents are used when PTA is immediately unsuccessful or when lesions recur soon after a previous angioplasty. There is no evidence that primary stenting is better than a policy of angioplasty with selective stenting for PTA failure.1,2 Five-year patency rates are around 64–75%,3 which, although lower than those of surgical aortobifemoral bypass, are acceptable considering the minimally invasive nature of this treatment.
Patients with diffusely stenosed iliac arteries respond less well to PTA. These patients are often treated with stents, although there is no definite evidence to support this policy.
Occlusions.
Occlusions of the iliac artery are usually amenable to endovascular treatment, with a technical success rate of recanalisation of around 80% (Fig. 86-7). Most operators favour primary stent insertion because angioplasty carries a 7–24% risk of significant distal embolisation.4 The durability of endovascular treatment of iliac artery occlusion is similar to that for iliac artery stenosis.
Common Femoral Artery and Profunda Femoris
Stenoses of the common femoral artery are amenable to PTA. Access to these lesions is usually gained from the contralateral groin involving catheter and guidewire manipulation across the aortic bifurcation. However, common femoral endarterectomy is a straightforward procedure and may be performed under local anaesthesia. Surgery is considered a better option than PTA at this site when lesions are calcified and eccentric. If the SFA is patent or salvageable by intervention, PTA of a stenosis in the profunda artery is usually not carried out. However, if the SFA is occluded, then any stenosis of the main profunda trunk should be treated by PTA or at the time of endarterectomy. The success and durability rates of PTA are similar to those for the SFA (see below).
Occlusions of the common femoral artery and profunda femoris are generally treated surgically.
Superficial Femoral Artery
Stenosis.
Angioplasty is the first-line treatment for stenosis of the superficial femoral artery. Patency is around 55% at 5 years,3 which is lower than for surgical bypass using vein grafts. However, most patients are treated by PTA because of the lower rate of complications compared with surgery. Angioplasty can be repeated if lesions recur. An additional advantage of angioplasty is that it spares the long saphenous vein, which is commonly used for femoropopliteal bypass, but which is also used for coronary artery bypass. The results of angioplasty are less satisfactory if the vessel is diffusely stenosed or if the number of calf run-off vessels is reduced. The technical success of stenting is higher than for angioplasty, but studies have found no convincing long-term benefit for stents versus PTA. More recently, drug-eluting balloons and stents have been introduced. These devices are coated with immunosuppressive and anti-proliferative drugs (e.g. sirolimus and paclitaxel) that have been shown to limit neointimal hyperplasia, and therefore inhibit vessel restenosis. Early evidence suggests improved patency of femoropopliteal lesions after treatment using either of these devices when compared with standard PTA balloons and bare metal stents.5–7
Occlusions.
SFA occlusions are usually treated by PTA (Fig. 86-8) followed by selective stent placement in cases where angioplasty is unsuccessful. Many radiologists use a technique called subintimal angioplasty in which a catheter and guidewire are manipulated outside the lumen of the vessel underneath the intima and into the subintimal space. Unless the vessel is heavily calcified, it is usually easy to advance the catheter and guidewire down the occluded vessel via the subintimal space. When the guidewire reaches the level of the patent vessel below the occlusion, it re-enters the lumen. After replacing the catheter with a balloon catheter, the subintimal space is dilated in the usual manner. Overall, the results for endovascular management of SFA occlusions are lower than for stenoses.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree