A variety of nonatherosclerotic diseases affect the arteries of the pelvis and lower extremities. Chronic repetitive traumatic conditions, such as popliteal entrapment and external iliac artery fibroelastosis, vasculitis and connective tissue diseases, and noninflammatory vascular diseases, are a few of the more commonly encountered nonatherosclerotic peripheral vascular diseases. Ultrasound, computed tomography angiography, and magnetic resonance angiography are essential in the initial assessment and management of patients with peripheral vascular disease.
Key points
- •
Cross-sectional imaging with ultrasound, computed tomography angiography, and magnetic resonance angiography has an essential role in the evaluation of patients with nonatherosclerotic peripheral vascular disease.
- •
Magnetic resonance angiography with stress maneuvers can detect popliteal entrapment syndrome accurately.
- •
External iliac arterial wall thickening, stenosis, and kinking are features of external iliac artery endofibrosis.
- •
In advanced stages of thromboangiitis obliterans, corkscrew collateral vessels can be apparent on imaging.
- •
Visceral artery dissections are a hallmark of segmental arterial mediolysis.
Introduction
Although atherosclerosis, varicose veins, and deep venous thrombosis are the most common vascular disease affecting the lower extremities, a wide variety of other chronic diseases also can affect the lower extremity arteries. This article presents examples of the more commonly encountered of these, including popliteal arterial entrapment syndrome, external iliac endofibrosis, vasculitis, connective tissue disease, and noninflammatory vascular diseases. Imaging has an essential role in the diagnosis and management of these entities. Keys to imaging nonatherosclerotic vascular diseases include visualization of the vessel wall and surrounding soft tissues in addition to imaging the vessel lumen. Cross-sectional imaging, including ultrasound (US), computed tomography angiography (CTA), and magnetic resonance angiography (MRA), are fundamental in assessing patients suspected of having one of these syndromes and for preoperative planning. ,
Popliteal artery entrapment syndrome
Patients with popliteal artery entrapment syndrome (PAES) frequently present with lower extremity claudication, paresthesia, or swelling with exertion. PAES commonly occurs in young adults. Complications of PAES include distal thromboembolism and formation of aneurysms. , PAES can be due to anatomic variants or functional entrapment that occurs during plantar flexion. There are 6 types of PAES ( Table 1 ). Anatomic PAES (types 1–5) can be due to abnormal course of the vessel (type 1) or due to an abnormal course of the muscles or fibrous band within the popliteal fossa (types 2–4). When an anatomic type also involves the popliteal vein, it is considered type 5. Type 6 of PAES is known as functional PAES due to compression of the popliteal artery between the medial and lateral heads of the gastrocnemius muscle. The etiology of functional PAES remains uncertain, but it occurs when there is popliteal artery compression despite normal anatomy. A diagnosis of PAES relies on a combination of ankle-brachial index, US, MRA, and CTA.
| Type | Description |
|---|---|
| 1 | Popliteal entrapment due to an abnormal popliteal artery course, usually medially to the medial head of the gastrocnemius muscle |
| 2 | Popliteal entrapment due to the medial head of the gastrocnemius muscle compressing the normally located popliteal artery |
| 3 | Popliteal entrapment due to and accessory slip of the medial head of the gastrocnemius muscle compressing the normally located popliteal artery |
| 4 | Popliteal entrapment due to the popliteus muscle or fibrous band compressing the normally located popliteal artery |
| 5 | When types 1–4 involve the popliteal artery and vein |
| 6 | Functional compression of the popliteal artery (and vein) between the medial and lateral heads of the gastrocnemius |
For the initial evaluation of patients with suspected PAES, US with duplex Doppler frequently is used because it allows for real-time visualization of popliteal artery compression. Occasionally, the popliteal artery is completely compressed. During plantar flexion, Doppler pressure measurements increase in the affected extremity and are essential in establishing the diagnosis. , In patients with functional PAES ( Figs. 1 and 2 ), detection of these changes in pressure with provocation can be crucial in making a diagnosis because this may be the only finding in the absence of anatomic abnormalities on CTA and MRA.


The need to apply pressure with the transducer during the evaluation, which can artificially increase velocities, is a limitation of US for the evaluation of PAES. Furthermore, the popliteal vessels can move out of the region of interest of the Doppler during plantar flexion resulting in an apparent occlusion. , Athletes are a particular group of patients in whom duplex Doppler US can have a high false-positive rate in the initial assessment of PAES. In patients with a positive duplex Doppler US examination or in patients with a negative duplex Doppler US examination with a high pretest probability of PAES, MRA should be performed for confirmation.
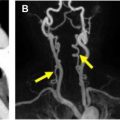
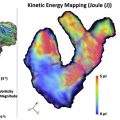
As with duplex Doppler US, contrast-enhanced MRA with time-resolved acquisitions ( Fig. 3 ) can be performed without and with dynamic plantar flexion. Although MRA frequently is used as a confirmatory test after duplex Doppler US, the long MRA acquisitions during plantar flexion can lead to motion artifacts that lower the quality of the study. , , Even with these potential limitations, MRA recently was shown superior to digital subtraction angiography (DSA) for PAES diagnosis. This is probably because the assessment of the anatomy within the popliteal fossa is an essential component of the evaluation and is best accomplished using a combination of T1-weighted and T2-weighted sequences. ,

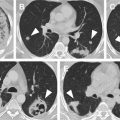
CTA can be used to confirm the presence of PAES in a similar fashion as MRA, with dynamic acquisitions during plantar flexion and at rest (see Fig. 2 ). CTA can be performed with a single, long contrast bolus administration. Abnormal muscular and tendinous structures within the popliteal fossa also can be detected with CTA. , Due to the ionizing radiation with CTA, MRA and duplex Doppler US remain the preferred imaging studies in patients with PAES.
Invasive catheter x-ray angiography (XA) is considered the reference standard for identifying the dynamic vascular deviation and obstruction in patients with PAES. , , XA, however, is not able to assess the extravascular anatomy and determine the exact type of PAES.
External iliac artery endofibrosis
External iliac artery endofibrosis (EIAE) is an uncommon cause of lower extremity claudication. As implied by its name, the external iliac artery affected is most commonly. The common iliac artery also can be involved, however, in up to 15% of patients. EIAE frequently is associated with long-distance cycling but has been reported in other types of high-performance endurance athletes. Patients with EIAE suffer from performance-limiting lower extremity pain and weakness that is relieved with rest. The exact cause of EIAE is not known but may be related to the repetitive trauma the hypertrophied psoas muscles exert on the external iliac artery during flexion, causing vasospasm and arterial kinking. The initial evaluation of patients with EIAE includes assessment of ankle-brachial pressure indices at rest and during exercise. Patients with EIAE have decreased ankle-brachial pressure indices with exercise.
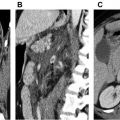
US, CTA ( Figs. 4 and 5 ), and MRA can be used to assess the patency of the external iliac arteries in patients with EIAE. Findings of EIAE include arterial wall thickening, stenosis, and kinking. US duplex Doppler US has the advantage of being able to assess flow and vessel morphology in real time during provocative maneuvers in patients with suspected EIAE. , duplex Doppler US should be performed with the hip flexed and extended to try to detect changes in anatomy and flow typical of EIAE. Catheter angiography can be used to measure pressure changes in the external iliac artery during maneuvers , and to treat EIAE noninvasively with stent placement.