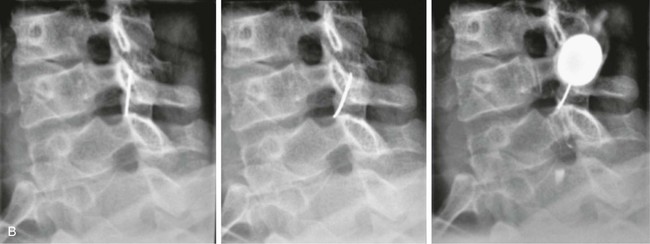
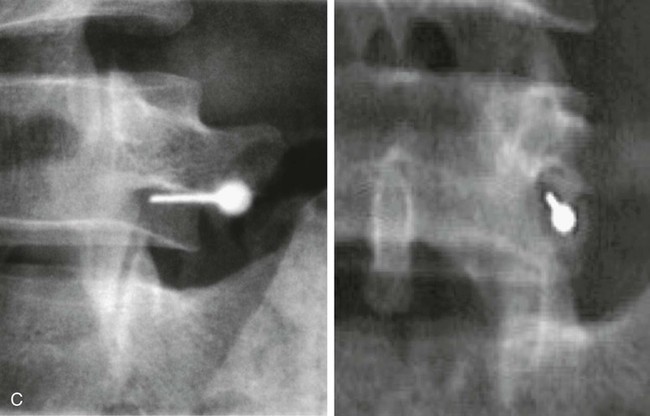
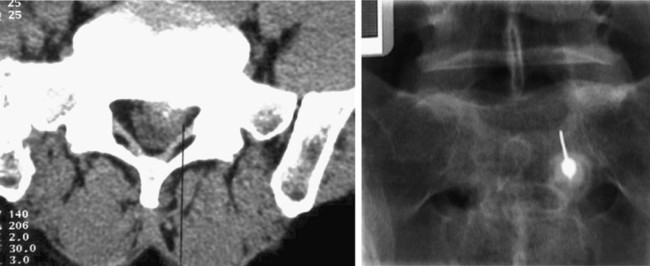
Chapter 167 Gianluigi Guarnieri, Roberto Izzo and Mario Muto These techniques can be performed under CT, CT-fluoroscopy, or fluoroscopy guidance (digital subtraction angiography [DSA] or C-arm) with the patient in prone position and under local anesthesia. The intention is to selectively inject 1 to 2 mL of an analgesic steroid drug (Depo-Medrol 20-40 mg or Solu-Medrol 20 mg) at a specific level correlated with the patient’s clinical symptoms to obtain an analgesic effect. Local anesthetic must never be injected into the cervical spine because of the risk of cervical epidural block or intrathecal injection, with resultant cardiorespiratory arrest.2 • LBP with or without radicular symptoms • An MRI showing evidence of degenerative disk disease or herniated disk refractory to 2 to 3 weeks of medical therapy • In the cervical region, we suggest treating only patients with clinical signs of radiculopathy and herniated disk. There is no correlation between clinical symptoms and herniated disk dimension. • Patients with edematous nerve roots due to inflammatory reaction in degenerative disk disease; these can be seen on MRI. Intravenous access is always required for emergencies in case of a vagal reaction with hypotension. For the lumbar level treatment, if fluoroscopy guidance is used, it is important to perform a CT scan prior to the procedure to exclude a retro-psoas bowel loop. CT-fluoroscopy is the best guidance, but there is a potentially higher radiation dose exposure to the patient. The technique is performed with a 17- to 20-gauge (for thoracic or lumbar level) or 19- to 21-gauge (for cervical level) Chiba needle. A postero-oblique approach is used for the epidural, perigangliar, or foraminal space at the lumbar or thoracic level; for the cervical level, a posterior or anterolateral approach with manual dislocation of the carotid axis is required (Fig. e167-1, A). For epidural injection, the needle is advanced into the epidural space by a dorsal oblique (20-30 degrees caudal and lateral to midline) paramedian approach up to the superior margin of the spinal lamina, just subjacent to the interlaminar gap. The needle can then be pushed over the lamina, through the ligamentum flavum into the dorsal epidural space at the midline. For foraminal injection, one uses a lateral angle greater than that used for the interlaminar technique, generally 35 to 45 degrees from the midline. The drug should be injected slowly to avoid reflux near the needle. An injection of therapeutic oxygen-ozone (10 mL of 30 µg/mL at lumbar area; 3-4 mL at cervical area) can be performed after steroid injection to increase the antiinflammatory and analgesic action. At the lumbar level, addition of a local anesthetic (just 1 mL of lidocaine 1%) is suggested, but this is never performed at the cervical level because epidural diffusion and consequent respiratory distress could be the consequence. Patients do not need hospitalization and can stand up after the procedure without the need for any other medical treatment. Good short-term results (up to a rate of 40%-65%) are typically achieved, but the results at long-term follow-up are lower.2–3 The transforaminal approach is target specific and requires the smallest volume to reach the primary site of pathology, specifically the anterior-lateral epidural space and the dorsal root ganglion for the cervical level, while the posterolaterale epidural space for the lumbar level (Fig. e167-1, B-C). The interlaminar entry can be directed more closely to the assumed site of pathology, requiring less volume than the caudal route (Fig. e167-2). The caudal entry is achieved fairly easily with minimal risk of inadvertent dural puncture, but it requires a relatively high volume (10-20 mL) of injectate to reach the site of pathology. The mechanism of action of epidurally administered steroid with or without local anesthetic injections is well understood. The resultant neural blockade alters or interrupts nociceptive input, reflex mechanisms of the afferent fibers, self-sustaining activity of the neurons, and the pattern of central neuronal activities. Local anesthetics interrupt the pain/spasm cycle and reverberating nociceptor transmission, and corticosteroids reduce inflammation by inhibiting either the synthesis or release of a number of proinflammatory mediators and by causing a reversible local anesthetic effect. A radiopaque marker is used to identify the skin entry point, and sterile technique is recommended. For an epidural approach at lumbar level, the patient is placed in prone position, and under fluoroscopic or CT guidance, a 22-gauge spinal needle is advanced into the epidural space via a dorsal oblique paramedian approach. The puncture site is typically 2 to 4 cm from the midline and 2 to 3 cm caudal to the intended point of entry into the dorsal epidural space. An 18-gauge venipuncture needle is placed from a puncture site 2 to 3 cm from the midline and without caudal offset over the desired interlaminar gap. An epidural needle with a blunt tip and side hole is then passed through the introducer needle to the midline dorsal epidural space. After the needle is placed, contrast material could be injected for epidurography, followed by therapeutic injection.
Periradicular Therapy
Perineural, Epidural, and Foraminal Pain Injections
General Inclusion, Exclusion, and Contraindications Criteria
Inclusion Criteria
Equipment and Technique
Epidural Injection
Periradicular Therapy