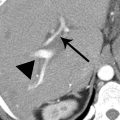
2 A patient presented with gastrointestinal bleeding. A finding was noted on the CT shown below. After further workup, the patient did not require treatment, and findings were stable at 3 years. This condition may be seen as part of a multisystemic process in association with which of the following diseases?

A. Retroperitoneal fibrosis
B. Tuberous sclerosis
C. Whipple disease
D. Graft versus host disease
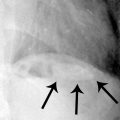
3a A 72-year-old woman presents to the emergency department with abdominal pain. What finding is suggested by the supine radiograph below?

A. Pneumoperitoneum
B. Small bowel obstruction
C. Ascites
D. Bladder outlet obstruction
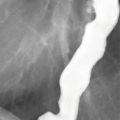
3b A CT scan was performed on the patient from the previous question. What is the most likely etiology of the ascites?

A. Tuberculous peritonitis
B. Malignant peritoneal mesothelioma
C. Spontaneous bacterial peritonitis
D. Peritoneal carcinomatosis
4 An 84-year-old woman presents with nausea and vomiting. What is the finding on the following abdominal radiograph and CT scan?

A. Chilaiditi sign
B. Small bowel obstruction
C. Colonic perforation
D. Morgagni hernia
5 A 55-year-old man with a history of a Whipple procedure for resection of ampullary carcinoma was evaluated with CT scans. The CT on the left was obtained 3 weeks after surgery, and the CT on the right was obtained 18 months later. What is the abnormality in the left anterior abdomen?

A. Omental infarction
B. Liposarcoma
C. Peritoneal carcinomatosis
D. Jejunal diverticulitis
6 A 60-year-old woman presents with abdominal pain, distention, and constipation. Images from a CT scan are shown below. No malignant cells were identified in the fluid obtained at paracentesis. What is the most likely etiology of the imaging findings?

A. Cirrhosis with portal hypertension
B. Appendiceal neoplasm
C. Intraperitoneal bladder rupture
D. Sclerosing encapsulating peritonitis
7 On this CT image from a 47-year-old woman with resolving acute pancreatitis, match each labeled retroperitoneal structure (A to F) with the corresponding anatomic description (1 to 6). Each option may be used only once.
A. Anterior renal fascia
B. Posterior renal fascia
C. Lateroconal fascia
D. Anterior pararenal space
E. Perirenal space
F. Posterior pararenal space

8 A 74-year-old man presents with abdominal pain and vomiting for 1 week. What is the diagnosis based on the CT image?

A. Ruptured aortic aneurysm
B. Lymphoma
C. Type II endoleak
D. Leiomyosarcoma
A. Ascites
B. Dilated colon
C. Pneumoperitoneum
D. Loculated pleural effusion
10a A 55-year-old man with a history of total colectomy and J-pouch reconstruction for ulcerative colitis is now 4 days status post surgery for ileostomy takedown. Which statement is most likely TRUE about the appearance of the abdomen on the following radiograph?

A. The patient requires surgical exploration.
B. The patient requires percutaneous drainage.
C. Findings are within expectations for the postoperative state.
D. Findings are most likely related to mechanical ventilation.
10b What sign is demonstrated in the right upper quadrant on the following supine AP abdominal radiograph?

A. Rigler sign
B. Falciform ligament sign
C. Football sign
D. Inverted V sign
11 A 67-year-old woman presents with a palpable concern. What is the most likely diagnosis based on the following CT image?

A. Renal angiomyolipoma
B. Retroperitoneal liposarcoma
C. Perirenal abscess
D. Omental infarction
12 The CT images below are from a 45-year-old woman with abdominal pain. What is the most likely diagnosis?

A. Colon carcinoma
B. Ovarian carcinoma
C. Prior bacterial peritonitis
D. Hyperparathyroidism
13 Images from a CT scan in a patient with lower abdominal and back pain are shown below. No malignancy was found on subsequent evaluation. This disease process most commonly affects which group of patients?

A. Men aged 20 to 30
B. Women aged 20 to 30
C. Men aged 40 to 60
D. Women aged 40 to 60
14 For the finding associated with the IVC in patients 1 to 3, select the most likely diagnosis (A to E). Each option may be used once, more than once, or not at all.
A. Mixing artifact
B. Pseudolipoma
C. Bland thrombus
D. Tumor thrombus
E. Primary IVC sarcoma
Patient 1. Axial and coronal images from contrast-enhanced CT.

Patient 2. Axial and coronal images from contrast-enhanced CT.

Patient 3. Axial, coronal, and axial images from multiphase contrast-enhanced CT.

15 A 44-year-old man underwent contrast-enhanced CT of the abdomen after a motor vehicle crash. A small amount of intraperitoneal fluid was detected, with densities indicated on the images. What is the most likely explanation of this fluid?

A. Rupture of the bladder
B. Rupture of the duodenum
C. Hemoperitoneum most recently from liver
D. Hemoperitoneum most recently from spleen
Match the images for the patients in Questions 16 to 19 with the most likely diagnosis (A to D). Each option may be used only once.
A. Testicular carcinoma metastases
B. Lymphoma
C. Extra-adrenal pheochromocytoma
D. Lymphangioma
20 A 53-year-old man complains of 2 weeks of right lower quadrant pain. Based on the CT image shown below, which additional sign or symptom may the patient have at presentation?

A. Edema in the lower extremity
B. Fluid draining from the abdominal wall
C. Pain exacerbated by hip extension
D. Numbness in the saddle area
21 A 74-year-old woman undergoes a CT urogram for the evaluation of recurrent urinary tract infection. What is the most likely diagnosis of the finding on the following CT image?

A. Desmoid tumor
B. Liposarcoma
C. Lymphoma
D. Sclerosing mesenteritis
22 A 31-year-old woman with history of inflammatory bowel disease and Caesarean section presents with pelvic and back pain. An MRI was performed. What is the most likely diagnosis?

Axial FS T2W, axial T1W, and coronal FS T2W MRI.
A. Colonic duplication cyst
B. Peritoneal inclusion cyst
C. Congenital mesothelial cyst
D. Mature cystic teratoma
23 A 74-year-old man remains hospitalized several days after aortobifemoral bypass graft surgery, which was complicated by a large hemorrhage. The patient has acutely developed renal failure. A CT scan was performed with enteric contrast administered through the gastrostomy tube but no IV contrast. What is the most likely diagnosis?

A. Splenic laceration
B. Gastric perforation
C. Pseudomyxoma peritonei
D. Abdominal compartment syndrome
ANSWERS AND EXPLANATIONS
1 Answers: A5; B8; C6; D4; E1; F3; G2; H7.The peritoneum is the longest and most complex serous membrane in the body. The peritoneal cavity is a potential space that is surrounded by parietal peritoneum along the abdominopelvic body wall and by visceral peritoneum around the abdominopelvic organs. It is open in women at the ostia of the fallopian tubes and closed in men. The abdominal peritoneal cavity can be subdivided into the supramesocolic and inframesocolic compartments, which are located superior and inferior to the transverse mesocolon, respectively. The supramesocolic compartment can be subdivided into the subphrenic spaces, subhepatic spaces, and lesser sac, whereas the inframesocolic compartment can be subdivided into the infracolic and paracolic spaces. The subphrenic, subhepatic, infracolic, and paracolic spaces together comprise the greater sac of the abdominal peritoneal cavity.



A5: The falciform ligament is a peritoneal reflection that extends between the umbilicus and liver and contains the ligamentum teres, the obliterated remnant of the umbilical vein.
B8: The small bowel mesentery is a fold of peritoneum that suspends the small bowel from the posterior abdominal wall and extends from the ligament of Treitz to the ileocecal junction.
C6: The hepatoduodenal ligament extends from the duodenum to the hepatic hilum and contains the main portal vein, proper hepatic artery, and extrahepatic bile duct. It forms the anterior margin of the foramen of Winslow (the site of communication between the greater and lesser sacs of the peritoneal cavity) and comprises a portion of the lesser omentum.
D4: The paracolic spaces are located inferior to the transverse mesocolon. The right and left paracolic spaces are located lateral to the ascending and descending colon, respectively, and deep to the parietal peritoneum.
E1: The subphrenic spaces are separated by the falciform ligament anteromedially. The right subphrenic space surrounds the right hepatic lobe and medial segment of the liver deep to the right diaphragm/body wall. The left subphrenic space surrounds the lateral segment of the liver, proximal stomach, and spleen deep to the left diaphragm/body wall.
F3: The lesser sac is bounded by the stomach, proximal duodenum, lesser omentum (hepatoduodenal and gastrohepatic ligaments), and gastrocolic ligament anteriorly, the pancreas posteriorly, the gastrosplenic and splenorenal ligaments on the left, and the transverse mesocolon and greater omentum inferiorly. The foramen of Winslow is located along its right side.
G2: The subhepatic spaces are located inferior to the liver. The right subhepatic space includes the hepatorenal space, or Morison pouch, and is contiguous with the right subphrenic space. The left subhepatic space, also called the gastrohepatic recess, is located between the lateral segment of the liver and the stomach, to the left of the gastrohepatic ligament, and is contiguous with the left subphrenic space. The left subhepatic space is separated from the left paracolic space by the phrenicocolic ligament.
H7: The gastrocolic ligament is a portion of the greater omentum that extends between the greater curvature of the stomach and the transverse colon.
The infracolic spaces are located inferior to the transverse mesocolon. The right infracolic space is located between the ascending colon and small bowel mesentery, and the left infracolic space is located between the descending colon and small bowel mesentery.
References: Meyers MA, Charnsangavej C, Oliphant M. Intraperitoneal spread of infections and seeded metastases. In: Meyers MA, Charnsangavej C, Meyers OM (eds). Dynamic radiology of the abdomen—normal and pathologic anatomy, 6th ed. New York, NY: Springer-Verlag, 2011:69–108.
Torigian DA, Kitazono MT. Peritoneal cavity. In: Torigian DA, Kitazono MT (eds). Netter’s correlative imaging: abdominal and pelvic anatomy. Philadelphia, PA: Elsevier, 2013:109–206.
2 Answer A.Retractile mesenteritis is in the spectrum of sclerosing mesenteritis, a condition characterized by chronic mesenteric inflammation. It can be seen as part of the multisystemic IgG4-related inflammatory diseases, which includes retroperitoneal fibrosis, the correct answer choice in this question. There is a lobulated mass (arrows) with dense calcifications and spiculated margins tethering the ileal mesentery. The two primary considerations with these features are carcinoid tumor metastasis and retractile (fibrosing) mesenteritis. Both can occur with or without calcifications. The two entities are frequently indistinguishable with other malignancies also in the differential diagnosis, so further evaluation and/or biopsy is usually required. A clue to the diagnosis of carcinoid instead of retractile mesenteritis would be a hypervascular mass representing the primary neuroendocrine neoplasm within the adjacent small bowel, often a subtle finding. In this case, further evaluation was negative for neuroendocrine tumor or other malignancy, and subsequent stability for years without treatment was consistent with retractile mesenteritis.

The spectrum of sclerosing mesenteritis at pathology includes:
- Mesenteric panniculitis (inflammation)
- Mesenteric lipodystrophy (fat necrosis)
- Retractile mesenteritis (fibrosis), considered late stage with more invasive behavior
Patients are commonly asymptomatic, or occasionally present with abdominal pain, weight loss, intestinal obstruction/ischemia, mass, or diarrhea.
The differential diagnosis for mesenteric calcification also includes benign and malignant entities. Calcifications can be seen in ovarian cancer and mucinous tumors as well as treated lymphoma. Granulomatous infection or inflammation, such as tuberculosis or sarcoidosis, may be seen as calcified mesenteric lymph nodes.
Tuberous sclerosis, Whipple disease, and graft versus host disease have not been associated with sclerosing mesenteritis. Tuberous sclerosis is a genetic neurocutaneous disorder with thoracoabdominal findings of lymphangioleiomyomatosis (LAM, with lung cysts), renal angiomyolipomas, renal cysts, and renal cell carcinomas. Whipple disease is an infection with the Whipple bacillus Tropheryma whipplei classically presenting with arthralgias and abdominal symptoms. Patients with Whipple disease may have nodular bowel wall thickening and low-density adenopathy. Graft versus host disease is an immune response in the recipient of an allogeneic hematopoietic cell transplant to donor cells. It can involve the gastrointestinal tract with diffuse bowel wall thickening.
References: Horton KM, Lawler LP, Fishman EK. CT findings in sclerosing mesenteritis (panniculitis): spectrum of disease. Radiographics 2003;23(6):1561–1567.
Levy AD, Rimola J, Mehrotra AK, et al. From the archives of the AFIP: benign fibrous tumors and tumorlike lesions of the mesentery: radiologic–pathologic correlation. Radiographics 2006;26(1):245–264.
3a Answer C.The abdominal radiograph shows the bowel gathered toward the center of the abdomen, suggesting a large volume of surrounding ascites. There is no evidence of small bowel obstruction with scattered gas in nondilated small bowel and colon. No extraluminal lucencies to indicate pneumoperitoneum are shown, with the caveat that a single supine AP view is insensitive for pneumoperitoneum. There is increased density and absence of bowel gas in the pelvis, which can be seen with a distended bladder. However, in this case, the increased density is generalized and related to the large volume of ascites throughout the abdomen and pelvis.
3b Answer D.Axial contrast-enhanced CT images confirm a large volume of ascites. There is thickening and nodularity of the peritoneum (short black arrows) including nodularity at the liver surface. There is confluent enhancing soft tissue in the greater omentum (long white arrows) consistent with omental caking. In the United States, findings most likely represent peritoneal carcinomatosis.

Tumors of ovarian and gastrointestinal origin are the most common causes of carcinomatosis. CT findings of peritoneal carcinomatosis include subtle infiltration of the omental or mesenteric fat; frank peritoneal, mesenteric, or omental soft tissue nodules; diffuse peritoneal nodular thickening and enhancement; complex ascites; and abdominopelvic organ invasion. Lymphomatosis (peritoneal involvement by lymphoma) is uncommon but may have the same appearance as carcinomatosis.
CT is the study of choice for the evaluation of peritoneal and mesenteric pathology. Common sites of peritoneal implants are in the dependent aspects of the pelvis (pouch of Douglas in women or retrovesical space in men), ileocecal region, paracolic gutters, subhepatic space, subphrenic space, and root of the mesentery. Patients can develop small bowel obstruction from tumor implants, which may be multifocal. Peritoneal carcinomatosis is incurable and predominantly treated with chemotherapy. In patients with ovarian and primary peritoneal carcinomatosis, cytoreductive surgery has been shown to increase survival.
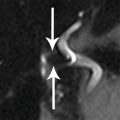
Peritoneal tuberculosis may present with similar findings as peritoneal carcinomatosis, but is less common in the United States. Malignant peritoneal mesothelioma is a rare and often rapidly fatal malignancy, with the main risk factor being prior asbestos exposure. Spontaneous bacterial peritonitis (SBP) usually occurs in patients with cirrhosis. SBP typically demonstrates smooth peritoneal thickening and enhancement (arrows on the following image) along with ascites. Clinical correlation is important as smooth enhancement does not exclude peritoneal malignancy.

Smooth peritoneal thickening in peritonitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree