PET-CT and SPECT-CT of Benign Bone Tumors
Abbas Yousefi-Koma
Klaus Strobel
Benign bone tumors are commonly noted in children and young adults. They can be classified into bone-forming, cartilage-forming, connective tissue, and vascular lesions. Plain films often suffice for the characterization of nonaggressive benign bone lesions, and additional imaging and biopsy is superfluous. Discrimination between benign and malignant bone tumors is crucial because treatment is completely different: in most benign bone tumors, often no treatment or only follow-up imaging is performed; malignant bone tumors are treated with surgery, chemotherapy, radiation, or combined therapies. Unnecessary bone biopsies of benign lesions should be avoided.
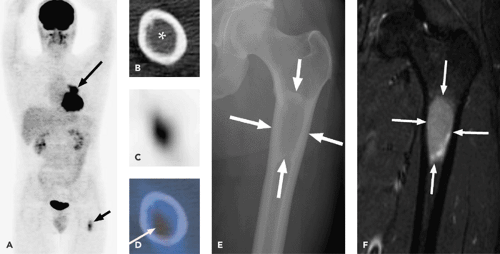
Data on the use of positron emission tomography (PET), integrated PET–computed tomography (CT), and integrated single-photon emission computed tomography (SPECT)-CT in this field are very limited. Increased fluorine 18 fluorodeoxyglucose (18F-FDG) uptake in benign bone tumors, such as giant cell tumor or fibrous dysplasia (see Fig. 65.1), can lead to misinterpretation and a diagnosis of malignancy. Although FDG-PET-CT can be useful for distinguishing benign from malignant bone tumors and for assessing the grade of musculoskeletal sarcomas (see Chapter 51), there is a considerable overlap of standard uptake values (SUVs) between the two groups. If the CT part of PET-CT studies is performed with a high-resolution technique on multi-slice scanners, the information obtained can be of great help in localizing and characterizing bone lesions. A special background in musculoskeletal radiology is useful for reaching the correct conclusions. In some situations, additional imaging with MRI should be considered.
SPECT and SPECT-CT have increased sensitivity and specificity compared with planar scintigraphy in conventional bone scanning. For the detection of osteoid osteoma or osteoblastoma, SPECT-CT seems to be the ideal imaging method.
General Considerations
Besides hemangiomas of the spine, osteochondromas, and enchondromas, most benign bone tumors are very rare. The primary aim of imaging bone lesions should be to reach a specific diagnosis in order to decide whether biopsy, surgery, or only observation is the best option for further management. Plain radiography is still the most important first-step imaging method in the diagnosis of bone tumors. In many locations with complex anatomy, like the spine or the pelvis, conventional radiographs fail to show the whole extension of a bone lesion. Multi-slice CT provides exact anatomic information about the center of a bone lesion (medullary, cortical, periosteal, parosteal), periosteal changes, sclerotic reactions, and cortical alterations (remodeling, endosteal scalloping, focal penetration).
PET-CT Imaging
PET-CT is a promising tool for evaluating the biological behavior and histopathological grade of primary bone lesions in a noninvasive manner (1,2,3). Little is known about FDG-PET-CT in benign bone tumors and tumor-like lesions. It is very important for reporting PET-CT studies to know that there are benign PET-positive bone tumors: fibrous dysplasia, giant cell tumors, chondroblastoma, sarcoidosis, Langerhans cell histiocytosis, aneurysmal bone
cysts, and nonossifying fibromas (4,5,6,7,8). It seems that, in particular, histiocytic and giant cell–containing lesions often have SUVs greater than 2.0. Although FDG-PET-CT can be useful for distinguishing benign from malignant bone tumors and for assessing the grade of musculoskeletal sarcomas (Chapter 51), there is a considerable overlap of standard uptake values (SUVs) between the two groups (4,9,10). First results show that PET cannot overcome the clinical problem of discriminating between benign enchondromas and low-grade chondrosarcomas.
cysts, and nonossifying fibromas (4,5,6,7,8). It seems that, in particular, histiocytic and giant cell–containing lesions often have SUVs greater than 2.0. Although FDG-PET-CT can be useful for distinguishing benign from malignant bone tumors and for assessing the grade of musculoskeletal sarcomas (Chapter 51), there is a considerable overlap of standard uptake values (SUVs) between the two groups (4,9,10). First results show that PET cannot overcome the clinical problem of discriminating between benign enchondromas and low-grade chondrosarcomas.
Dehdashti et al. evaluated 20 intraosseous lesions with FDG-PET and correctly diagnosed 14 of 15 malignant and 4 of 5 benign lesions with a cutoff value of 2.0 SUV. Thirteen of the malignant lesions were metastatic carcinomas. Aoki et al. investigated 52 primary bone lesions with FDG-PET and observed a statistically significant difference in SUV between benign and malignant bone tumors overall. However, a significant overlap of SUVs was observed in the two groups. SUVs greater than 2.0 were noted in all five giant cell tumors, all three chondroblastomas, three of six fibrous dysplasias, one sarcoidosis, one Langerhans cell histiocytosis, and one of three nonossifying fibromas. Schulte et al. investigated 202 bone lesions (70 high-grade sarcomas, 21 low-grade sarcomas, 40 benign tumors, 47 tumorlike lesions, 6 osseous lymphomas, 6 plasmacytomas, and 12 metastases of an unknown primary tumor). All lesions were biopsied. Using a tumor-to-background ratio cutoff level for malignancy of 3.0, the sensitivity of FDG-PET was 93.0%, the specificity was 66.7%, and the accuracy was 81.7% (11). Most cases of primary bone lymphomas, Ewing sarcomas, and osteosarcomas show a high uptake in FDG-PET. Chondrosarcomas are characterized by lower SUVs than possessed by other bone sarcomas. In general, cartilaginous tissue has a tendency to be hypovascular or avascular.
Cartilage tumors include enchondromas, osteochondromas, and chondrosarcomas. Histopathologic grades correlate well with the clinical outcome of the patients (12). Lee et al. evaluated 35 cartilage tumors preoperatively with FDG-PET. The mean SUVmax values were 1.1 for benign tumors, 0.9 for grade I chondrosarcomas, and 6.9 for high-grade chondrosarcomas (grades II and III). The authors calculated a positive predictive value of 82% and a negative predictive value of 96% for high-grade sarcomas with a cutoff SUV of 2.4 (13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree