Head and neck cancers are commonly encountered cancers in clinical practice in the United States. Fluorine-18-fluorodeoxyglucose ( 18 F-FDG) PET/CT has been clinically applied in staging, occult primary tumor detection, treatment planning, response assessment, follow-up, recurrent disease detection, and prognosis prediction in these patients. Alternative PET tracers remain investigational and can provide additional valuable information such as radioresistant tumor hypoxia. The recent introduction of 18 F-FDG PET/MR imaging has provided the advantage of combining the superior soft tissue resolution of MR imaging with the functional information provided by 18 F-FDG PET. This article is a concise review of recent advances in PET imaging in head and neck cancer.
Key points
- •
18 F-FDG PET/CT has value in the evaluation and management of head and neck cancers with advantages over conventional anatomic imaging.
- •
18 F-FDG PET/CT plays a significant role in the assessment of treatment response in head and neck cancers with high negative predictive value thereby reducing unnecessary invasive diagnostic procedures.
- •
Alternative PET tracers can provide additional information such as tumor hypoxia which can guide treatment planning.
Introduction
Head and neck cancers (HNCs) are a group of cancers involving the different structures in the head and neck region. In clinical practice, the most common location of these cancers is the oropharynx (34%), larynx (28%), and oral cavity (18%). Other locations include the hypopharynx, nasal cavity, nasopharynx, paranasal sinuses, salivary glands, and skin. Approximately 53,260 new cases of oral cavity and oropharynx cancer were estimated to be diagnosed in the United States in 2020, accounting for 2.9% of all new cancer diagnoses. The estimated number of deaths due to these cancers is approximately 10,750, accounting for 1.8% of all cancer deaths. In 2017, an estimated 383,415 people were living with oral cavity and pharyngeal cancers in the United States. The survival of these patients depends on the stage of disease, with 5-year survival ranging from 85.1% in patients with localized disease to 40.1% in those with distant disease. This variance in outcomes emphasizes the importance of accurate and timely diagnosis and staging, where imaging plays a crucial role. Most HNCs are squamous cell carcinoma by histopathology and termed head and neck squamous cell carcinomas (HNSCCs). This article focuses on the role of 18 F-FDG PET/CT and PET/MR imaging in the evaluation and management of HNCs. A brief discussion on alternative PET radiotracers and their potential role in HNC evaluation is also presented.
Staging head and neck cancers
With recent advances in the understanding of the biology of different tumors of the head and neck, there have been changes in the primary tumor (T), local lymph node disease (N), and metastasis (M) staging of these tumors, as proposed by the most recent (eighth) edition of the AJCC Cancer Staging Manual by the American Joint Committee on Cancer (AJCC). For example, the human papillomavirus (HPV) status of HNSCC tumors has been found to have a significant impact on the behavior of cancers, and the vast majority of HNSCCs in the United States are attributed to HPV-related cancers. These tumors are more susceptible to chemoradiation and have better outcomes than HPV-negative tumors. This factor is incorporated into the most recent staging system. When assessing these tumors, the important features to evaluate on imaging pertinent to the staging system include tumor size in the greatest dimension, maximum depth of invasion (evaluated primarily on MR imaging), invasion of tumor into adjacent structures, number of nodes involved, size of the involved node, features of extranodal extension, whether the nodes are ipsilateral or contralateral to the tumor, and findings of distant metastases, The depth of invasion, in addition to the tumor size, is included in the updated system, whereas prior versions included only the maximal tumor size. In routine anatomic imaging, size criteria and abnormal morphology are used to identify pathologic lymph nodes. Although diagnostic accuracy is lower in small lymph nodes that do not meet size criteria, 18 F-FDG PET/CT can be useful in identifying metastatic disease in these small nodes.
Role of PET in the evaluation of head and neck cancers
In the initial workup of the HNC primary site, CT of the soft tissues of the neck or MR imaging of the neck is indicated to delineate the primary tumor. MR imaging may be preferred over CT in certain specific indications, such as assessing skull base extension, cranial nerve involvement, bone involvement of tumor in patients with dental implants, and resultant artifact, that make CT evaluation suboptimal. CT can add useful information to MR imaging findings in evaluating bone or cartilage involvement. The imaging techniques should extend to the base of the neck for optimal nodal evaluation. In patients where no obvious primary tumor has been identified, 18 F-FDG PET/CT is recommended before further evaluation or biopsy to potentially identify the primary site for targeted tissue sampling. Sampling of metastatic nodes may be necessary for diagnostic purposes, and some of these nodes can be cystic. As with the nodes often commonly encountered with HPV-associated tumors, image-guided biopsy is recommended to increase the yield. In patients with extensive nodal disease or nodes involving the lower neck, aggressive tumor histology, and patients undergoing definitive radiation therapy, 18 F-FDG PET/CT can be useful in detecting additional nodal or distant disease. For surgical treatment planning, 18 F-FDG PET/CT is recommended for surgical planning of the contralateral neck in tumors that cross or are near the midline. In the evaluation of distant metastases in locally advanced HNCs, 18 F-FDG PET/CT is recommended. In the early follow-up of these patients, 18 F-FDG PET/CT can be performed in addition to or in place of anatomic imaging when evaluating recurrent, residual disease or second primary malignancy to guide treatment. Posttreatment response assessment with 18 F-FDG PET/CT following definitive radiation or chemoradiation therapy is recommended 3 to 6 months after treatment to reduce false-positive findings secondary to inflammation early in the follow-up. In late follow-up (>6 months), 18 F-FDG PET/CT is not routinely indicated unless there are clinical symptoms or concerning signs for recurrent disease. However, surveillance 18 F-FDG PET/CT can detect recurrent malignancy or a second primary tumor in approximately 10% of patients 1 year after treatment (NCCN guidelines v 2.2020).
Imaging findings
Staging
18 F-FDG PET/CT has been shown to be useful in pretreatment staging and evaluation, especially for detecting clinically negative metastases including clinically negative neck disease, with a significant impact on treatment strategies.
Staging: Primary Tumor
In HNC primary tumor evaluation, recent studies have shown that 18 F-FDG PET/CT may have advantages over CT and MR imaging with higher diagnostic accuracy. The limitations of primary tumor evaluation by 18 F-FDG PET/CT should be considered. Precise tumor size estimation, small-volume tumors, infiltration of surrounding soft tissues, depth of invasion, perineural spread, or bone marrow involvement may be better evaluated on MR imaging. However, in small tumors (T1-T2), a prospective study has shown that 18 F-FDG PET/CT demonstrates higher sensitivity than MR imaging (83% vs 63%) in identifying these small tumors, with good interobserver variability. It should be noted that the use of contrast-enhanced diagnostic CT studies of the head and neck performed with these PET/CT studies provides better evaluation, especially for small tumors. Streak or susceptibility artifact related to hardware or dental implants is commonly encountered in imaging HNCs and can have a significant impact on the accurate evaluation of these primary tumors. 18 F-FDG PET/CT has been shown to provide better evaluation of primary tumors in these patients than provided by MR imaging, with superior correlation with the pathologic tumor volume at resection. While reviewing images of these patients, careful evaluation of the non-attenuation-corrected PET images separately can provide a better picture of abnormal metabolic activity.
Staging: Nodal Disease
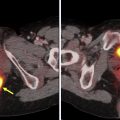
It has been well established that 18 F-FDG PET/CT provides added advantage to clinical examination and routine anatomic imaging in evaluating nodal metastases in HNC. An important finding published in the recent past is the advantage of 18 F-FDG PET/CT in the evaluation of clinically negative HNSCC (T2-T4) in a prospective multicenter trial (ACRIN 6685). Using an optimal maximum standardized uptake value (SUVmax) cutoff of 1.8, the negative predictive value was estimated to be 94%, resulting in changes in surgical management in 22% of the patients, with additional nodal-level dissection in 14% and fewer dissection in 5% of these patients. Approximately 10% of patients who undergo therapeutic or planned neck dissections can develop complications such as postoperative infection, seroma, flap-necrosis, etc. The advantage of 18 F-FDG PET/CT described above can lead to a decrease in perioperative morbidity, with higher morbidity often associated with more extensive neck dissections and radiation. Given these improved outcomes, the 18 F-FDG PET/CT approach has been found to be cost-effective per quality-adjusted life-year. The overall diagnostic performance of 18 F-FDG PET/CT in the detection of nodal metastases in HNC is good, with pooled sensitivity and specificity of 84% and 84%, respectively, per neck-side and 84% and 96% per nodal-level analyses, respectively, in a meta-analysis of 742 patients with HNC. The outcome and survival of patients with HNC are affected by the risk of lymph node metastases, and hence, accurate early detection of cervical nodal metastases is crucial in these patients ( Fig. 1 ).

Staging: Distant Metastasis
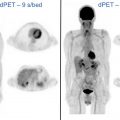
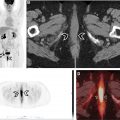
In addition to the advantages of using 18 F-FDG PET/CT for local tumor and nodal disease evaluation as described above, one of the most useful applications of this modality is detecting distant disease that is often not detected by conventional imaging techniques. Distant disease is associated with poor outcomes, and timely detection is extremely important for aggressive tailored treatment planning strategies to improve the prognosis in these patients. The risk of distant metastases is higher in certain HNCs than in others. For example, the highest rates of distant metastases at primary evaluation were associated with nasopharyngeal cancers (9%), followed by those of the hypopharynx (7%), oropharynx (4%), larynx (3%), and oral cavity (2%). In cancers excluding the nasopharynx, the overall rate of distant metastases was approximately 3%. Overall, the most common site of distant metastases appears to be the lung (54%), followed by bone. However, in nasopharyngeal cancers, the most common site of distant metastases is the bone (50%), followed by lung (33%) and liver (27%). Factors associated with distant metastases are nodal status, especially N3 disease, advanced T-stage, older age, poorly differentiated tumors, etc. In oropharyngeal cancers with known HPV status, HPV-negative tumors are associated with a higher chance of distant metastases than HPV-positive tumors (4% vs 2%; P <.05). In patients with risk factors of distant metastases and nasopharyngeal cancers with a higher risk of bone metastases, PET/CT is useful in the staging evaluation. A meta-analysis including 1147 patients with HNC demonstrated a sensitivity of 83% and specificity of 96% in detecting distant metastases. The corresponding values for conventional imaging methods were 44% and 96%, respectively. These results show the advantage of using 18 F-FDG PET/CT over conventional imaging methods to detect distant metastatic disease ( Fig. 2 ).

Treatment planning
In recent years, 18 F-FDG PET/CT findings have been increasingly used to plan image-guided radiation therapy for optimal tumor control and treatment response while maintaining minimal radiation to the adjacent normal background tissues, given the vital structures in the neck such as cranial nerves, blood vessels, salivary gland, spinal cord, etc. In up to 10% of patients, 18 F-FDG PET/CT findings can alter primary tumor and nodal disease volumes and detect additional metastatic disease or synchronous malignancies, resulting in changes in radiation treatment planning. , 18 F-FDG PET/CT-based nodal disease volume, in comparison with CT nodal volume, has shown improved regional disease control, and in turn, a positive impact on patient outcome. Image-guided radiation treatment planning techniques are constantly evolving, and newer methods are being proposed to improve tumor control. For example, 18 F-FDG PET/CT-based intensity-modulated arc therapy, compared with more widely used static intensity-modulated radiation therapy dose-based painting by numbers, has shown improved dose to surrounding normal tissues at risk with better treatment efficacy and shorter delivery time. In the recent past, integration and coordination of different medical specialties have improved the evaluation of oncologic patients. Comparing images of radiation treatment planning prior to treatment with follow-up, 18 F-FDG PET/CT has been suggested to improve the diagnostic accuracy of differentiating disease recurrence versus postradiation inflammation. An ongoing clinical trial (UPGRADE-RT) evaluates the implementation of 18 F-FDG PET/CT-guided de-escalation of radiation therapy dose to small lymph nodes that do not meet size criteria assessed by 18 F-FDG PET/CT in HNC patients to evaluate the risk of disease recurrence while improving quality of life with reduced complications related to radiation to important normal structures in the head and neck.
Treatment response assessment
18 F-FDG PET/CT plays an important role in the imaging evaluation of response to treatment within 6 months of completion of treatment, especially in patients undergoing organ-preserving systemic therapy alone or combined with radiation therapy. To reduce false-positive findings related to posttreatment inflammation, the optimal time for performing these scans is 3 to 6 months (NCCN guidelines v 2.2020). Posttreatment 18 F-FDG PET/CT performed up to 12 months after treatment completion in patients with OPSCC can detect residual or recurrent disease in almost half the patients. However, false-positive findings can also be seen in one-third of the patients. The greatest value appears to be a high negative predictive value in patients undergoing surgery (100%) or chemoradiation (97%). Lower positive predictive value and specificity is seen in patients undergoing chemoradiation in comparison with patients undergoing primary surgery, likely related to posttreatment inflammation. 18 F-FDG PET/CT with SUVmax values greater than 5 are associated with a higher rate of residual or recurrent disease. In a meta-analysis including 1293 HNSCC patients, the pooled sensitivity, specificity, positive predictive, and negative predictive values were 85%, 93%, 58%, and 98%, respectively. As shown by these results, a significantly higher negative predictive value has an impact on the clinical evaluation of these patients, resulting in fewer unnecessary diagnostic or therapeutic interventions. The authors found lower sensitivity (75% vs 89%; P = .01) and specificity (87% vs 95%; P <.005) in HPV-positive tumors. The reason behind these findings is not clearly understood, but proposed theories include better response to radiation therapy in comparison with HPV-negative tumors, resulting in longer duration for developing radioresistant tumor cells and increased inflammatory response secondary to T-cell-mediated immunity causing decreased specificity. The high negative predictive value is valuable with patients who have a negative scan showing superior progression-free and overall survival. A randomized controlled trial (PET-NECK trial) of 564 patients showed that 18 F-FDG PET/CT surveillance after primary chemoradiation therapy in HNSCC patients with N2 or N3 disease was associated with a reduction in neck dissections, which results in fewer surgical complications and lower treatment cost (approximately US$2190). There was no significant difference in the results based on the HPV status of the tumors.
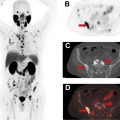
Qualitative Treatment Response Assessment Criteria
In the recent past, there have been multiple proposed qualitative treatment response assessment criteria in HNC patients. These include the Neck Imaging Reporting and Data System (NI-RADS), Hopkins, Porceddu, and Deauville criteria. , All these criteria use a proposed scoring system or categorization based on the qualitative assessment of the metabolic activity at the site of the primary tumor or cervical lymph nodes and some criteria comparing this uptake to reference blood pool and liver metabolic activity to suggest the presence or absence of recurrent disease. An example of one of these treatment response criteria (Hopkins criteria) is presented in Table 1 . This scoring system categorizes scores of 1, 2, and 3 as negative and scores of 4 and 5 as positive for residual disease. The authors reported a sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy of 68%, 92%, 71%, 91%, and 87%, respectively. The high negative predictive value favors using such criteria for treatment response assessment to prevent unnecessary invasive evaluations. These categories were also able to predict survival in these patients. Since introducing these criteria, there have been many validation studies and studies comparing the different criteria. In a prospective multicenter study (the ECLYPS study), Hopkins criteria for treatment response assessment in locally advanced HNSCC patients after primary chemoradiation indicated high negative predictive value (92%), specificity (91%), and accuracy (86%). The authors observed a time-dependent decrease in recurrent disease detection, with optimal performance approximately 12 weeks after completion of treatment. A similar high negative predictive value for this criteria was seen in other clinical trials (NRG-HN002). A recent study comparing the abovementioned different qualitative assessment criteria concluded that all 4 treatment response assessment criteria had similar diagnostic performance in detecting recurrent disease in a large (n = 562) study of HNSCC patients treated with chemoradiation or radiation therapy alone in the site of primary tumor and nodal disease. A significant difference in progression-free and overall survival was associated with all 4 criteria ( P <.0001). The highest number of overall indeterminate scores was associated with NI-RADS, while the least was associated with Hopkins criteria, likely related to the more subjective nature of the NI-RADS criteria. Marginal improvement in negative predictive value was observed with Deauville and Porceddu criteria while keeping the number of indeterminate scores low ( Fig. 3 ).
| Score | 18 F-FDG Uptake | Response Category |
|---|---|---|
| 1 | Less than IJV blood pool | Complete metabolic response |
| 2 | Focal uptake greater than IJV but less than liver | Likely complete metabolic response |
| 3 | Diffuse uptake greater than IJV or liver | Likely inflammation |
| 4 | Focal uptake greater than liver | Likely residual tumor |
| 5 | Focal and intense uptake | Residual tumor |

Occult primary detection
Metastatic cancer identified in cervical lymph nodes without a clinically evident primary head and neck tumor is a diagnostic dilemma requiring a streamlined evidence-based algorithm for optimal diagnosis and management of these patients. The workup of these patients often includes a comprehensive clinical evaluation, imaging, panendoscopy, tonsillectomy, etc, which improves the detection rate with improvement in the prognosis of these patients. The most common location of the unknown primary tumors is in the oropharynx, especially in the palatine tonsil, followed by the base of the tongue, nasopharynx, and hypopharynx. Identification of the occult primary tumor results in improved outcomes in these patients. Applying 18 F-FDG PET/CT has the added advantage of detecting occult primary tumors with high diagnostic accuracy (89%). However, some studies report lower sensitivity likely due to inflammatory radiotracer uptake similar to that of common conditions like tonsillitis. Overall, studies report that 18 F-FDG PET/CT can detect primary tumors in approximately 40% of patients. Using a simplified qualitative Likert scale of metabolic activity, sensitivity was 94% and specificity was 73% in detecting the primary tumor at a per-patient level. No significant difference was identified in comparison with diffusion-weighted MR imaging (DWI). The authors also found a significant difference in quantitative assessment (SUVmax) in detected primary tumor compared with unknown primary tumors (11.56 vs 6.43; P = .002). In quantitative assessment, 18 F-FDG PET/CT was superior to DWI. Given that the most common location of these occult head and neck tumors is the palatine tonsil, careful evaluation of tonsillar metabolic activity is important. An SUVmax cutoff ratio of 1.5 between the bilateral tonsils resulted in 100% sensitivity and specificity in detecting cancers. The mean SUVmax of cancers of the tonsils was significantly higher than for the contralateral normal side and control patients (9.4 vs 2.5 vs 3.0; P <.0001).
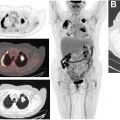
Second primary malignancy detection
In a prospective study of 248 patients with HNC, a second primary malignancy was detected in approximately 7% of patients. A meta-analysis of 12 studies demonstrated a pooled sensitivity of 88% and pooled specificity of 95% for detection of distant metastases and second primary malignancies by 18 F-FDG PET/CT. Physiologic metabolic activity in organs like the esophagus decreases the ability of 18 F-FDG PET/CT to detect a second primary malignancy, and hence, close attention while evaluating sites with normal background physiologic metabolic activity is crucial. Compared with a conventional workup, 18 F-FDG PET/CT also appears to assist in decreasing false-positive diagnoses. The most encountered locations of a second primary malignancy include esophagus, stomach, thyroid, lung, colon, and breast. A second primary malignancy diagnosis is associated with poor overall survival (HR = 3.07; P = .002) and progression-free survival (HR = 2.3; P = .016) ( Fig. 4 ).