The role of PET imaging with 11 C-choline and 18 F-fluciclovine in evaluating patients with prostate cancer (PCa) has become more important over the years and has been incorporated into the NCCN guidelines. A new generation of PET radiotracers targeting the prostate-specific membrane antigen (PSMA) is widely used outside the United States to evaluate patients with primary PCa and PCa recurrence. PET imaging influences treatment planning and demonstrates a significantly higher disease detection rate than conventional imaging such as computed tomography and MR imaging. Early data indicate that using PET radiotracers such as 18 F-fluciclovine and PSMA improves patient outcomes. 68-Ga-PSMA-11 and 18F-DCFPyL-PET/CT were recently approved by the US Food & Drug Administration (FDA) for clinical use. Other PSMA radiotracers, including fluorinated variants, will likely gain FDA approval in the not-too-distant future.
Key points
- •
18 F-fluciclovine and prostate-specific membrane antigen (PSMA) PET/CT have demonstrated high positive predictive value in detecting extraprostatic malignancy in patients with biochemical recurrence with diagnostic performance exceeding that of conventional imaging.
- •
Although 18 F-fluciclovine is not FDA approved for use in initial staging, both 18 F-fluciclovine and PSMA PET/CT may help identify patients with occult metastasis who may not benefit from curative surgery in primary prostate cancer.
- •
Early data indicate that the use of 18 F-fluciclovine and PSMA PET improves patient outcomes.
- •
18 F-fluciclovine excels in local disease detection because of limited urinary excretion, whereas PSMA has superior performance in extraprostatic disease detection.
- •
PSMA PET can serve as a means of selection for treatment with PSMA radioligand therapy.
Introduction
The role of PET imaging with 11 C-choline and 18 F-fluciclovine in evaluating patients with prostate cancer (PCa) has become more important over the years and has been incorporated into the NCCN guidelines. A new generation of PET radiotracers targeting the prostate-specific membrane antigen (PSMA) is widely used outside the United States to evaluate patients with primary PCa and PCa recurrence.
Choline PET
Choline is a component of phosphatidylcholine incorporated into the cell membrane. The enzyme choline kinase is upregulated in many cancers, including PCa. In September 2012, 11 C-choline was FDA approved for PET imaging of patients with suspected PCa recurrence. Choline radiotracers have been mostly replaced by PSMA PET worldwide and are not widely available in the United States compared with the FDA-approved synthetic amino acid PET radiotracer 18 F-fluciclovine.
18 F-fluciclovine PET
Pathophysiology and Biodistribution
18 F-fluciclovine is a fluorinated synthetic amino acid PET tracer approved by the FDA for imaging of patients with suspected PCa recurrence after prior treatment. In PCa cells, amino acid transport is significantly upregulated. 18 F-fluciclovine physiologic activity is most intense in the pancreas and liver. Variable mild to moderate physiologic uptake is seen in salivary glands, pituitary, adrenals, muscle, esophagus, bowel, and bone marrow; 18 F-fluciclovine has greater heterogeneity than seen with 18 F-fluorodeoxyglucose (FDG). Mild uptake is noted within the blood pool and brain parenchyma. 18 F-fluciclovine is only minimally excreted by the kidneys with little to no resulting bladder activity, though a minority of patients may exhibit an early excretion pattern.
Normal Variants/Pitfalls
18 F-fluciclovine is not prostate specific, as other benign and malignant neoplasia have upregulated amino acid metabolism and may have increased 18 F-fluciclovine uptake, such as lung, breast, and gynecologic cancers as well as meningioma and osteoid osteoma. , It is not uncommon to have mild to moderate symmetric 18 F-fluciclovine benign activity in inguinal, distal external iliac, and axillary nodes. Periurethral tissue may have mild to moderate activity, and therefore, sagittal images can help differentiate physiologic uptake from recurrence at the vesicourethral anastomosis. The early appearance of bladder or ureteral activity may mimic tumor or abnormal lymph nodes, respectively.
Degenerative uptake is less intense and less commonly described than with FDG PET. Though amino acid imaging demonstrates less inflammatory uptake than FDG, amino acid transport also occurs in benign inflammation, and therefore fluciclovine uptake not specific to malignancy can occur. For bone lesions, uptake is typically more intense with lytic or mixed sclerotic lesions. Indolent, dense sclerotic lesions may have little or no 18 F-fluciclovine uptake. Occasional 18 F-fluciclovine uptake seen in isolated red marrow in the pelvis or proximal femurs may stimulate metastasis. In these cases, bone-specific MR imaging, skeletal scintigraphy with agents such as sodium 18 F-fluoride or 99 m Tc-methylene diphosphate, or biopsy may be required.
Patient Preparation and Imaging Protocol
Patient preparation and imaging protocol for 18 F-fluciclovine PET have been described in detail. , In brief, the patient is advised to fast (except for medications) for 4 hours and avoid excessive physical activity starting 24 hours before the scan. If possible, patients should refrain from voiding 15 to 30 minutes before the study to mitigate early urine tracer excretion.
PET images should start at 4 minutes (3–5 min) postinjection of 10 mCi (370 MBq) 18 F-fluciclovine as an IV bolus. As the dynamic tracer washout is relatively fast, it is important not to delay the start of the PET images. The CT can be acquired within the 4-minute interval between 18 F-fluciclovine injection and PET acquisition. CT images with IV contrast should be performed after the PET, as the IV contrast may act as a diuretic and increase early urinary excretion.
Image Interpretation
18 F-fluciclovine image interpretation is based on the uptake compared with defined background regions such as bone marrow and blood pool. , Typical PCa recurrence patterns should be kept in mind when interpreting 18 F-fluciclovine PET. , Overall, any lesion with increased uptake equal to or higher than bone marrow (level of normal L3 vertebrae) should be considered suspicious for malignancy. Lesions smaller than 1 cm may demonstrate lower activity due to partial volume artifact, and therefore the threshold for positivity is lower. Hence, subcentimeter structures should be considered suspicious when uptake is significantly above the adjacent visualized blood pool uptake and approaches the bone marrow uptake. , For bone lesions, focal activity should be clearly seen on the maximum intensity projection (MIP) image.
Primary Disease and Staging
Neither characterization of the primary lesion nor initial staging are FDA-approved indications for 18 F-fluciclovine. While primary malignant lesions have higher uptake versus normal prostate tissue, there is a significant overlap in uptake between PCa and nonmalignant processes such as benign prostatic hypertrophy. , Multiple studies have demonstrated a correlation between Gleason grade and 18 F-fluciclovine uptake. Approximately 28% of patients are undergraded on biopsy compared with prostatectomy. The possibility of using 18 F-fluciclovine to help direct biopsy to more aggressive occult lesions, especially with the addition of multiparametric PET/MR to refine characterization, is intriguing.
A multicenter Phase 2 trial for initial staging of primary PCa with 18 F-fluciclovine PET/CT in 28 patients reported sensitivity and specificity of 66.7% and 86.4%, respectively, for extraprostatic nodal disease. Another study of 28 patients with high-risk PCa in patients who underwent 18 F-fluciclovine PET/MR imaging before surgery reported patient-based and region-based sensitivity of 40% and 30%, respectively, with 100% specificity for the detection of regional lymph node metastases with a higher PPV of PET versus MR imaging alone.
A prospective study using 18 F-fluciclovine PET for preoperative staging in patients with intermediate-risk to high-risk primary PCa of 57 patients who subsequently underwent robotic radical prostatectomy with extended pelvic lymph node dissection reported a sensitivity and specificity for malignant nodal detection of 55.3% and 84.8% per patient, respectively, and 54.8% and 96.4% per region, respectively. The sensitivity was significantly higher than conventional imaging both on a patient-based (55.3% vs 33.3%, P <.01) and region-based (54.8% vs 19.4%, P <.01) analysis with similar high specificity. Metastasis detection correlates to the size of metastatic deposits within lymph nodes and overall metastatic burden. , Hence, 18 F-fluciclovine PET can be useful to guide lymph node dissection because of its high specificity and to help identify patients with occult metastasis who may not benefit from curative surgery.
Recurrence/Restaging
18 F-fluciclovine PET/CT demonstrated promising initial results in detecting malignancy in patients with biochemical recurrence (BCR). In a prospective clinical trial in which there was a 96.1% level of histologic proof, the detection rate was related to the prostate-specific antigen (PSA) level: 37.5% at a PSA of less than 1 ng/mL, 77.8% at 1 to 2 ng/mL, 91.7% at >2 to 5 ng/mL, and 83.3% at greater than 5 ng/mL, which was significantly better than CT. The sensitivity and specificity in the treated prostate or prostate bed were 90.2% and 40.0%, respectively; sensitivity and specificity for extraprostatic disease were 55.0% and 96.7%, respectively. Confounding uptake due to inflammation or prostatic hypertrophy was likely responsible for the lower specificity in the treated prostate. A subsequent study using 18 F-fluciclovine-guided transrectal ultrasound-guided biopsies reported that using a higher threshold of intensity minimizes false-positive results in the treated prostate. A multisite study of 596 patients reported a sensitivity of 88.1%, specificity of 32.6%, and PPV of 71.8% for local recurrence. Thus, histologic confirmation of findings in the treated prostate is recommended, yet there is high specificity for extraprostatic disease detection mirrored by the multisite study that reported a PPV of 92.3%.
In the prospective multicenter intention-to-treat LOCATE trial enrolling 213 patients with BCR, detection rate varied with PSA level: 31%, 79%, and 81% with a PSA (ng/mL) of 0 to 0.5, greater than 1.0, and greater than 2.0, respectively. A postscan change in management occurred in 59% of patients. The FALCON prospective trial enrolled 104 patients and reported a 64% change in management with detection rates of 29.5% and 93% in PSAs of less than and greater than 2.0 ng/mL, respectively. Interestingly, there was a 28.9% patient-level detection rate with PSA less than 0.5 ng/ml. A retrospective report of 152 patients from clinically performed 18 F-fluciclovine PET/CT demonstrated positivity rates of 58%, 87%, 100%, and 92% for PSA (ng/mL) levels of less than 1, 1 to 2, 2 to 5, and greater than 5, respectively.
A final analysis of patients from a randomized prospective trial of 165 patients (NCT01666808) in a postprostatectomy setting with BCR reported a 35.4% change in therapy approach in patients who underwent standard of care imaging (abdominopelvic CT or MR imaging) followed by 18 F-fluciclovine PET/CT. Upon examining outcomes from salvage radiotherapy planning with standard imaging only versus those whose planning was based on the additional 18 F-fluciclovine PET/CT, a significant improvement in failure-free survival at 3 years (75.5% vs 63.0; P = .003) and 4 years (75.5% vs 51.2%; P <.001) was reported. A second similar randomized clinical trial (NCT03762759) will compare 18 F-fluciclovine and 68 Ga-PSMA in patients with BCR post-prostatectomy.
The detection of recurrent disease at low PSA levels has assumed importance as salvage radiotherapy is being offered at increasingly lower PSA levels. The reported detection rate of 18 F-fluciclovine at low PSA levels has varied widely. In the randomized salvage therapy outcomes trial above, there was a 72% detection rate with PSA less than 1 ng/mL while Wang and coworkers reported a 33% detection rate at this level. , Others have reported values in between 46.4% and 58% for PSA< or ≤1 ng/mL. , These differences in detection rates are likely related to specifics of trial populations, such as aggressiveness of disease.
Therapy Response Assessment with 18 F-Fluciclovine PET
Preliminary studies suggested that 18 F-fluciclovine could be used to assess response to therapy. , A small prospective study of patients with primary PCa undergoing androgen-deprivation therapy (ADT) reported a significant decrease in standardized uptake values (ie, SUVmax) of detected local and metastatic lesions on a subsequent PET/MR imaging scan. A second small retrospective study in patients with BCR found a correlation between PSA and the number of lesions to findings on post-therapy PET/CT scans. However, this needs to be further evaluated in larger prospective clinical trials.
Prostate-specific membrane antigen-targeted PET
Introduction to Prostate-Specific Membrane Antigen-Targeted PET
PSMA radiotracers are widely used throughout the world for PCa imaging and therapy. PSMA is a type II transmembrane glycoprotein with folate hydrolase activity and an extracellular domain that includes the enzyme active site. Expression of PSMA is seen in approximately 95% of PCa tumors. At the histologic level, aggressive and advanced PCa shows increased levels of PSMA expression. The accessibility of the active site to high-affinity ligands, combined with rapid internalization of PSMA from the cell surface, allows for high-contrast imaging.
Early in the clinical adoption of PSMA PET agents, 68 Ga-labeled radiotracers proliferated because of several factors including facile synthesis and the ability to make such compounds without access to a cyclotron. 68 Ga-PSMA-HBED-CC, later more commonly known as 68 Ga-PSMA-11 or simply 68 Ga-PSMA, became the dominant agent in the field. However, parallel to the development of 68 Ga-labeled radiotracers, PSMA-targeted agents labeled with fluorine-18 were also being explored, initially 18 F-DCFBC and other first-generation compounds, and later more widely used radiotracers such as 18 F-DCFPyL, 18 F-PSMA-1007, and 18 F-rhPSMA-7. ,
Patient Preparation and Imaging Protocol
Patient preparation and imaging protocol for PSMA-directed imaging PET were previously described. , Patients do not fast and are encouraged to be well hydrated. Voiding before imaging may decrease the frequency of halo artifacts. The dose range from 1.8 to 2.2 MBq (0.05–0.06 mCi) per kilogram for 68 Ga-labeled PSMA radiotracers, and 200 to 370 MBq (5–10 mCi) for the 18 F-labeled counterparts. After bolus injection, an uptake time of 1 h is recommended, although delayed acquisition or the use of furosemide may improve lesion detection. Field of view includes the base of the skull to midthigh with 3 to 4 min per bed position and images.
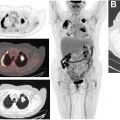
Normal Variants/Pitfalls
For most PSMA radiotracers, biodistribution includes the lacrimal glands, salivary glands, liver, spleen, kidneys, small bowel, ganglia, and urinary tract due to renal excretion. There are some variations among radiotracers. 18 F-DCFPyL has higher hepatic uptake than 68 Ga-PSMA-11, whereas 68 Ga-PSMA-11 has increased accumulation in the kidneys. 18 F-PSMA-1007 has less renal excretion, which can increase the lesion detection rate for small pelvic lymph node lesions or local recurrence. With increasing clinical availability of PSMA-directed imaging, the number of reported pitfalls is steadily increasing ( Fig. 1 ). Multiple benign pathologies with increased PSMA expression can be misinterpreted as malignant, for example, sympathetic ganglia, benign tumors (meningioma, schwannoma), soft tissue lesions (desmoid tumors, myxoma), or lung lesions (sarcoidosis, tuberculosis, or anthracosilicosis). Nonprostatic malignant tumors, however, may also have substantial PSMA expression; these include medullary thyroid carcinoma, renal cell carcinoma, breast cancer, and lung cancer.

Interpretative Criteria
Multiple standardized frameworks for image interpretation have been introduced for PSMA PET. For instance, Eiber and coworkers recently introduced the “PROMISE” system, which is based on a molecular imaging TNM classification (‘‘miTNM,’’ version 1.0). Using the “miPSMA expression score,” different uptake levels are considered relative to normal uptake in the blood pool, liver, and parotid glands. The local tumor is classified, which refers to extent and organ confinement ranging from “miT0” to “miT4”. In addition, a sextant segmentation of the prostate is used for intraprostatic tumor extension. Pelvic lymph node lesions are categorized (from “miN0” to “miN1b”). Last, the extrapelvic nodes (“miM1a”) and distant metastases (“miM1b” referring to bone or “miM1c” to other organ involvement) are also evaluated. In a prospective trial applying PROMISE to 68 Ga-PSMA-11 PET/CT in 635 men afflicted with PCa, interreader reproducibility was substantial, with a Fleiss κ of 0.65 to 0.78. Also providing reliable standards in PSMA PET/CT interpretation, the PSMA Reporting and Data System (RADS) framework has been recently introduced. In brief, a 5-point scale is applied to a maximum of 5 target lesions, with increasing numbers indicating a higher likelihood of malignancy. PSMA-RADS ranges from 1 = no evidence of disease and definitively benign to 5 = high certainty that prostate carcinoma is present and refers to the site of disease and the intensity of radiotracer uptake. Depending on the derived RADS score, PSMA-RADS also triggers further clinical workup—for example, by recommending biopsy or follow-up imaging. Taken together, this framework should increase the level of reader confidence, should facilitate communication with other specialists, and may guide the reader in determining whether radioligand therapy for PCa should be recommended. In a prospective setting enrolling 50 18 F-DCFPyL PET/CTs, the interobserver agreement rate using PSMA-RADS was excellent.
Prostate-Specific Membrane Antigen-Targeted PET in Primary Prostate Cancer and Initial Staging
Identification of primary PCa is ongoing research with PSMA PET. An early study with the first-generation agent 18 F-DCFBC noted that PET had an improved specificity for high-grade disease than MR imaging, although with a lower sensitivity. Other studies have been more promising. Eiber and colleagues found that 68 Ga-PSMA-11 PET had a significantly higher area under the receiver-operating-characteristic curve (AUC, 0.83) than multiparametric MR imaging (0.73). The combination of both modalities led to the highest AUC (0.88). Similarly, Hicks and colleagues found that 68 Ga-PSMA-11 PET/MR imaging sensitivity was superior to multiparametric MR imaging at the anatomic-region level. These findings suggest that PSMA PET may be appropriate to incorporate into biopsy planning.
PSMA PET is a useful staging modality for patients at risk of occult locoregional nodal involvement or distant metastatic disease. In single-center retrospective and prospective studies in men with intermediate-risk or high-risk PCa, PSMA PET has demonstrated moderate sensitivity and very high specificity for identifying pelvic lymph node involvement. The first published study on this topic reported a relatively low patient-level sensitivity of 33.3%, which is in line with larger multicenter trials, such as OSPREY (sensitivity 30.6%–41.9% among three readers) or a study with 68 Ga-PSMA-11 that reported sensitivity of 40%. The apparently low sensitivity of PSMA PET in multicenter trials suggests that there may be heterogeneity between centers and that care will need to be taken in translating PSMA PET beyond large tertiary care medical centers with specific expertise.
PSMA PET can predict biochemical persistence (BCP) after radical prostatectomy with lymph node dissection. Van Leeuwen and colleagues found that BCP was noted in 50% of men in whom lymph node involvement was seen on PSMA PET and confirmed histologically, whereas only 16.7% BCP was noted in men with lymph node involvement histologically but not identified on PSMA PET.
The recently published proPSMA trial found that PSMA PET outperformed conventional imaging for the systemic staging of men with high-risk PCa. Therefore, despite limitations in sensitivity, PSMA PET may become a clinical standard for staging patients being considered for curative-intent local therapy.
Prostate-Specific Membrane Antigen-Targeted PET for Recurrence, Restaging, and Metastatic Disease
The most widely studied aspect of PSMA PET imaging is detection efficiency in recurrent disease, as identifying the site of recurrence influences the approach to salvage therapy. Early studies on PSMA PET in the recurrence population varied in the reported detection efficiencies, which may have been due in part to the retrospective nature of many of the studies and differences in the degree of inclusion of patients with visible lesions on conventional imaging. However, the limitations from early studies have begun to be addressed by improved study designs. For example, Fendler and colleagues reported in a two-center prospective trial that sites of PCa were localized in 75% of men with recurrent disease and that the PPV of PSMA PET findings was 0.84 on a per-patient basis with histologic validation. Another recent prospective study that specifically excluded patients with evidence of disease on conventional imaging found a detection rate of 67.7%. Although detection efficiency generally tracks with serum PSA level, the rates of lesion localization are still moderate at low PSAs, and there are no current recommendations to exclude patients from imaging based on PSA level.
Phillips and colleagues reported the results of the ORIOLE trial, in which patients were randomized to either stereotactic ablative body radiation (SABR) or observation for oligometastatic disease identified on conventional imaging. SABR improved progression-free survival, particularly in a post hoc analysis that showed that inclusion of all PSMA-positive sites of disease in the treatment plan was beneficial. We can expect that the high sensitivity of PSMA PET will popularize metastasis-directed therapy in oligometastatic patients.
Therapy Response Assessment with Prostate-Specific Membrane Antigen-Targeted PET
There is a complex interplay between androgen signaling and PSMA expression, making interpretation of response assessment difficult. Hope and coworkers demonstrated that short-term ADT led to a flare phenomenon with increased uptake in known lesions and the appearance of new lesions. Longer-term ADT generally leads to decreased conspicuity of lesions. The initiation of second-generation anti-androgen therapy can also confuse patterns of changes in uptake on PSMA PET. Due to the apparent complexity of response assessment with PSMA PET, interest has arisen in developing response criteria. However, prospective data are needed to evaluate systemic therapy effects on PSMA expression.
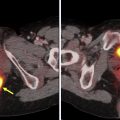
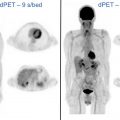
Prostate-Specific Membrane Antigen Ligands Versus 18 F-Fluciclovine
18 F-fluciclovine is a metabolic radiotracer, whereas PSMA is targeted to receptors. Thus, each radiotracer reflects a different aspect of PCa biology. Intrapatient comparisons of 18 F-fluciclovine and 68 Ga-PSMA-11 reported superior performance for 68 GA-PSMA-11 in detecting metastatic lymph nodes and skeletal disease, particularly for patients with PSAs less than 2 ng/mL. , For detecting local recurrence, 18 F-fluciclovine is reported to be superior to 68 Ga-PSMA-11 because of much lower urinary excretion, which could interfere with the detection of recurrence adjacent to the bladder ( Figs. 2 and 3 ).