Head and neck cancers are a diverse group of cancers with high morbidity and mortality within an area of complex anatomy. High-quality anatomic and functional imaging is essential for preoperative, chemotherapeutic, and radiotherapy planning. Early studies show that hybrid PET–MR imaging offers great potential for improving the imaging of head and neck cancers. Furthermore, advanced MR imaging techniques may also be incorporated to further enhance the diagnostic value of the combined modality.
Key points
- •
Hybrid PET–MR imaging offers high sensitivity and specificity for head and neck cancers, enabled by the functional imaging of PET and soft tissue discrimination by MR imaging.
- •
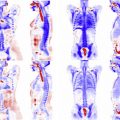
Whole-body imaging enabled by PET–MR imaging offers the ability to evaluate the primary tumor, local nodal, and distant metastases.
- •
Advanced MR imaging techniques, such as diffusion-weighted imaging and permeability imaging, can also add value to head and neck imaging.
Introduction
Head and neck cancers are a complex set of neoplasms that involve the nasal-oral-digestive tract, extending from the nose to the mediastinum, with a worldwide incidence of approximately 6.8%. There is significant geographic variability in causative agents including genetic susceptibility, cultural risk factors, smoking, alcohol, and infectious agents but ultimately there is significant morbidity and mortality from these cancers. The anatomic region in which these cancers occur is complex with multiple small structures that push the limits of conventional imaging resolution. Distant metastases are also common in these cancers, including metastases to the bone and lungs. Secondary cancers also occur at a high rate in survivors, reported as 3% to 7%.
Ultrasound, computed tomography (CT), MR imaging, and PET are commonly used imaging modalities for the evaluation of head and neck cancers, but each of these modalities has significant specific weaknesses. One of the strongest clinical indications for PET–MR imaging is likely the evaluation of cancers in this region, because of the limitations of the other modalities and importance of high-quality imaging on patient outcome. Furthermore, because of frequent distant metastases the whole-body approach of hybrid PET–MR imaging may be an advantage over conventional modalities.
A few factors point to the potential benefit of PET–MR imaging over conventional PET-CT or MR imaging for head and neck cancers. First, effective head and neck imaging requires high resolution and functional information. Second, staging of cancers in this region requires local and distant evaluation, for which PET–MR imaging offers distinct advantages. Finally, surgical and radiotherapy treatment planning is complex given the anatomy and structures at risk, and dual-modality approaches that include functional information may offer substantial benefits. Fig. 1 shows a patient with a primary tonsillar cancer and local nodal metastases imaged with PET–MR imaging.
Squamous cell carcinoma is the most important tumor entity of this area (also, Fig. 1 ). In recent years, PET-CT has broadly been applied for this indication and has been shown to be more accurate than CT alone for tumor detection and precise anatomic localization.
Previously, the most reliable data on the diagnostic performance of combined PET–MR imaging comes from studies using retrospective fusion of MR imaging and PET datasets. When compared with MR imaging and PET separately, the fused PET–MR imaging images have offered higher sensitivity and specificity to the presence of malignancy. Huang and colleagues investigated the diagnostic value of fluorodeoxyglucose (FDG) PET coregistered to anatomic MR imaging compared with PET-CT, CT, and MR imaging in advanced buccal squamous cell carcinoma. The authors found that fused PET–MR imaging images have the highest sensitivity and specificity of the four approaches. Furthermore, tumor size as measured by PET–MR imaging had a higher correlation coefficient ( r 2 = 0.96) with pathologic tumor size than CT ( r 2 = 0.55), MR imaging ( r 2 = 0.58), or PET-CT ( r 2 = 0.74).
The first report on integrated PET–MR imaging on patients with head and neck cancer showed that PET images obtained with the PET–MR imaging system exhibited better-detailed resolution and greater image contrast in comparison with those from the PET-CT system. The authors concluded that simultaneous PET–MR imaging of the head and upper neck area is feasible, and within a reasonable imaging time. These initial results are particularly important for demonstrating feasibility, because the interfaces between bone, air, and soft tissues in nasopharynx, oropharynx, and hypopharynx are considered major challenges for PET–MR imaging. Practically, however, many of these interfaces are evaluated by direct observation through endoscopy, and it not necessarily anticipated that PET–MR imaging would be responsible for the evaluation of a mucosal surface. It is worth noting that all modalities have somewhat limited sensitivity to the detection of head and neck cancers, particularly these small mucosal based lesions. Patients with head and neck cancers may present with nonhealing ulcers, difficulty swallowing, or neck masses representing primary or metastatic disease.
Accurate staging is essential for the treatment planning and prognostication in head and neck cancers, and staging is based on the tumor-metastasis-nodal system. PET-CT has been shown to offer additional diagnostic information that more appropriately stages patients in several studies. The early fusion work laid the ground work for the simultaneous imaging modality, but limitations to fusion remain because of differences in patient positioning. PET-MR offers different benefits for each staging component ( Box 1 ).
- •
T-staging by PET–MR imaging is more precise than other modalities because of its increased sensitivity in the evaluation of osseous involvement and perineural spread.
- •
N-staging by PET–MR imaging is improved through complimentary information offered by the different modalities.
- •
M-staging by PET–MR imaging relies on the ability of both modalities to perform whole-body imaging.
Introduction
Head and neck cancers are a complex set of neoplasms that involve the nasal-oral-digestive tract, extending from the nose to the mediastinum, with a worldwide incidence of approximately 6.8%. There is significant geographic variability in causative agents including genetic susceptibility, cultural risk factors, smoking, alcohol, and infectious agents but ultimately there is significant morbidity and mortality from these cancers. The anatomic region in which these cancers occur is complex with multiple small structures that push the limits of conventional imaging resolution. Distant metastases are also common in these cancers, including metastases to the bone and lungs. Secondary cancers also occur at a high rate in survivors, reported as 3% to 7%.
Ultrasound, computed tomography (CT), MR imaging, and PET are commonly used imaging modalities for the evaluation of head and neck cancers, but each of these modalities has significant specific weaknesses. One of the strongest clinical indications for PET–MR imaging is likely the evaluation of cancers in this region, because of the limitations of the other modalities and importance of high-quality imaging on patient outcome. Furthermore, because of frequent distant metastases the whole-body approach of hybrid PET–MR imaging may be an advantage over conventional modalities.
A few factors point to the potential benefit of PET–MR imaging over conventional PET-CT or MR imaging for head and neck cancers. First, effective head and neck imaging requires high resolution and functional information. Second, staging of cancers in this region requires local and distant evaluation, for which PET–MR imaging offers distinct advantages. Finally, surgical and radiotherapy treatment planning is complex given the anatomy and structures at risk, and dual-modality approaches that include functional information may offer substantial benefits. Fig. 1 shows a patient with a primary tonsillar cancer and local nodal metastases imaged with PET–MR imaging.
Squamous cell carcinoma is the most important tumor entity of this area (also, Fig. 1 ). In recent years, PET-CT has broadly been applied for this indication and has been shown to be more accurate than CT alone for tumor detection and precise anatomic localization.
Previously, the most reliable data on the diagnostic performance of combined PET–MR imaging comes from studies using retrospective fusion of MR imaging and PET datasets. When compared with MR imaging and PET separately, the fused PET–MR imaging images have offered higher sensitivity and specificity to the presence of malignancy. Huang and colleagues investigated the diagnostic value of fluorodeoxyglucose (FDG) PET coregistered to anatomic MR imaging compared with PET-CT, CT, and MR imaging in advanced buccal squamous cell carcinoma. The authors found that fused PET–MR imaging images have the highest sensitivity and specificity of the four approaches. Furthermore, tumor size as measured by PET–MR imaging had a higher correlation coefficient ( r 2 = 0.96) with pathologic tumor size than CT ( r 2 = 0.55), MR imaging ( r 2 = 0.58), or PET-CT ( r 2 = 0.74).
The first report on integrated PET–MR imaging on patients with head and neck cancer showed that PET images obtained with the PET–MR imaging system exhibited better-detailed resolution and greater image contrast in comparison with those from the PET-CT system. The authors concluded that simultaneous PET–MR imaging of the head and upper neck area is feasible, and within a reasonable imaging time. These initial results are particularly important for demonstrating feasibility, because the interfaces between bone, air, and soft tissues in nasopharynx, oropharynx, and hypopharynx are considered major challenges for PET–MR imaging. Practically, however, many of these interfaces are evaluated by direct observation through endoscopy, and it not necessarily anticipated that PET–MR imaging would be responsible for the evaluation of a mucosal surface. It is worth noting that all modalities have somewhat limited sensitivity to the detection of head and neck cancers, particularly these small mucosal based lesions. Patients with head and neck cancers may present with nonhealing ulcers, difficulty swallowing, or neck masses representing primary or metastatic disease.
Accurate staging is essential for the treatment planning and prognostication in head and neck cancers, and staging is based on the tumor-metastasis-nodal system. PET-CT has been shown to offer additional diagnostic information that more appropriately stages patients in several studies. The early fusion work laid the ground work for the simultaneous imaging modality, but limitations to fusion remain because of differences in patient positioning. PET-MR offers different benefits for each staging component ( Box 1 ).
- •
T-staging by PET–MR imaging is more precise than other modalities because of its increased sensitivity in the evaluation of osseous involvement and perineural spread.
- •
N-staging by PET–MR imaging is improved through complimentary information offered by the different modalities.
- •
M-staging by PET–MR imaging relies on the ability of both modalities to perform whole-body imaging.
T-staging
T-staging is mainly based on morphology and size of the tumor, including local osseous invasion. This staging level predicts the ability to surgically resect the primary lesion. MR imaging is known to be more accurate than CT alone for T-staging, with CT requiring PET to perform more accurate staging. Even within the PET-CT literature, there is some debate over the necessity of iodinated contrast-enhanced CT imaging with the use of FDG. However, FDG itself may underestimate disease presence, or the presence of a mildly standardized uptake value (SUV) change may be classified as nonspecific. Fusion studies of PET-CT with MR imaging suggest that a higher diagnostic accuracy was found with fusion images than conventional PET-CT. Subsequent studies with the simultaneous PET–MR imaging acquisitions demonstrate that there is good agreement between PET-CT and PET–MR imaging derived staging.
CT may offer a slight benefit in discriminating the highest stages because it directly evaluates osseous destruction, but MR imaging is more likely to demonstrate marrow or infiltrative involvement. Improved delineation of osseous structures using PET–MR imaging could be achieved using ultra short TE sequences; however, the early work that has explored this has suggested that significant shortcomings remain.
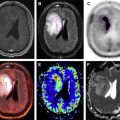
One of the advantages of PET–MR imaging is the relative high sensitivity of MR imaging to perineural spread. It is well known that PET-CT has poor sensitivity to perineural spread, and that other modalities should be sought when it is suspected. Clinically, the presence of perineural spread upstages tumors and reduces resectability. MR imaging is known to show higher sensitivity to perineural spread (100% vs 88%) compared with CT. Furthermore, as manufacturers have typically integrated 3-T MR imaging systems for the simultaneous modality, the advantages of higher field MR imaging will also be apparent. Further work with larger numbers of cases is required to more accurately evaluate the specificity of the dual modality. Fig. 2 demonstrates an extreme case of perineural spread where the disease has extended and enlarged the left optic nerve. The nerve enlargement is apparent by both PET and MR imaging in this case, but the combined modality reinforces involvement of the left cavernous sinus.
N-staging
The nodal and metastases staging levels determine the treatment and surgical plan for patients. Distant disease reduces the utility of surgery and treatment approaches shift to focus on systemic disease.
Early studies that compared simultaneous FDG PET–MR imaging with just MR or PET demonstrated good concordance at the primary site with mediocre sensitivity of nodal metastases with whole-body PET (55%) or whole-body gadolinium-enhanced MR imaging (40%), but high sensitivity with regional PET (98%) or the combined modality (100%). Subsequent studies by other groups have directly explored the role of PET–MR imaging for evaluating metastatic lymph nodes, with a review by Kim and colleagues discussing the ongoing concerns of how to interpret FDG nonavid but MR imaging–positive cases and the potential for treatment response monitoring. In Fig. 3 , the value of the combined modality is demonstrated in a patient in two lymph nodes that are equal in size by MR imaging evaluation. One node is FDG avid, suggesting malignant spread, whereas the other node is not FDG avid. Findings were subsequently confirmed by surgery. Short tau inversion recovery sequences are particularly useful for delineating lymph nodes.
Compared with whole-body MR imaging, FDG PET-CT was reported to have a significantly higher accuracy when staging lymph nodes for metastatic spread. Regarding the detection of metastasis in regional lymph nodes (N-staging), a sensitivity, specificity, and accuracy of 85%, 92%, and 89%, respectively, were reported in a prospective study with PET and MR imaging fusion. These results are slightly less than the diagnostic performance found in prospective PET-CT studies, which showed a sensitivity of 94% and a specificity of 84% for lymph node staging. The same PET–MR imaging prospective study showed an overall sensitivity of MR alone of 67% for assessment of tumor recurrence, compared with a sensitivity of 92% achieved by fused MR imaging and PET images. The earliest head-to-head comparisons of PET-CT with simultaneous PET–MR imaging suggest that there may not be statistical differences between the two combined modalities. In these studies the MR imaging criteria to differentiate benign from malignant lymph nodes were based on nodal size, contour, and presence of necrosis (heterogeneous contrast enhancement). Clearly, additional work is needed to better elucidate the potential differences, but the potential for novel development of new approaches on the MR imaging side may favor PET–MR imaging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree