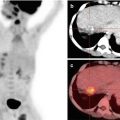
Fig. 7.1
FDG PET/CT in staging of pancreatic adenocarcinoma: MIP image (a) shows large area of tracer concentration in the mid-abdomen with focal tracer uptake in the liver. Axial PET/CT (b) shows FDG-avid large soft tissue mass in the body of pancreas with encasement of superior mesenteric artery on venous phase CT component (c–arrow) of PET/CT. There is intense desmoplastic reaction (c–arrowhead) with FDG uptake (b) delineating the actual tumor. Axial PET/CT (d–arrow) shows FDG-avid lesion in the liver which is seen as subtle hypodensity on CT (e–arrow) image suggestive of metastatic involvement
PET, with its metabolic dimension, provides the actual site of disease, since PACs are often accompanied by a dense desmoplastic reaction (Fig. 7.1b, c—arrowheads). This, in addition, provides accurate site for biopsy and tissue sampling [15]. In actual clinical practice, most patients undergo triphasic CT for diagnosis and are further referred for PET/CT imaging in locally advanced or borderline respectable scenarios to rule out the liver and other sites of distant metastases.
7.3.3 Nodal Staging
Some studies reported modest improvement in the performance of FDG PET compared with CECT in patients with pancreatic masses, with sensitivity and specificity ranging from 30% to 49% and 63% to 93%, respectively, for evaluation of lymph nodes. Lesser tumor volume in affected lymph nodes and strong photon scatter from the primary tumor (penumbra effect) may partially explain the poor performance of FDG PET for lymph node staging [16, 17]. Metabolic information of FDG PET may complement that of CT for nodal staging, because even low-grade metabolic activity on fused imaging in a rounded centimeter-or-more-sized node may be indicative of nodal metastases.
7.4 Liver Metastases
FDG uptake in hepatic lesions strongly favors metastatic involvement; also the absence of FDG uptake in suspicious liver lesions seen on conventional imaging rules out metastases [18]. This dilemma arises mostly in case of solitary focal liver lesion that appears suspicious on triphasic CT/ultrasonography; here FDG uptake is a clincher as the presence of uptake favors malignancy (Fig. 7.1d, e, arrows) and further can be managed by liver-specific interventions.
In a study comparing the performance of hepatobiliary contrast-enhanced MR imaging and FDG PET, MR imaging was more accurate in depicting small liver metastases, with a reported accuracy of 97.1% compared with 85.3% for FDG PET [19].
7.5 Other Distant Metastases
Small volume disease in the form of nodular peritoneal implants often seen as stranding and rarely as frank “caking” pose a diagnostic challenge on CT, with reported sensitivity of 65–88% and specificity of 38–63% [20]. Peritoneal implants were found at staging laparoscopy in 7% of patients with locally unresectable pancreatic cancer and no evidence of metastasis at CECT [21].
Since PET/CT imaging is a whole body study, it is the best modality for detecting distant metastases at any site.
Most of the centers incorporate breath-hold plain CT of chest in PET/CT protocol, for detection of metastatic lung nodules. This is because detection of subcentimeter-sized nodules is beyond the resolution of even modern-day PET scanners, and hence plain thin-section breath-hold CT serves the purpose.
Thus, PET/CT impacts management change in patients deemed “operable” on conventional imaging, by detecting distant metastases, thus avoiding the cost of futile surgery.
7.6 PET/CT to Detect Disease Recurrence
PACs are naturally aggressive cancers, and following the natural history, after surgery, 72–92% of pancreatic adenocarcinomas recur locally within 2 years [22]. Locally recurrent tumors are usually not resectable; however, radiation therapy or local ablation either with radiofrequency or cryoablation may be a palliative option. Postoperative changes in the surgical bed and early tumor recurrence have overlapping morphologic characteristics, as a result, differentiating between them is difficult on CECT. Moreover, it is often difficult to obtain an adequate tissue sample because desmoplastic reaction is known to be associated with pancreatic cancers. The use of FDG PET to depict tumor recurrence is promising, particularly when CT findings are equivocal [23, 24]. Increased FDG uptake in the surgical site at 3 months following surgery is usually indicative of recurrence (Fig. 7.2). The reported sensitivity of FDG PET for depicting tumor recurrence is 96% compared with 39% for CT and MR imaging [23]. Moreover, after resection, tumor relapse is depicted at FDG PET earlier than it is at CT, with higher sensitivity (98%) and specificity (90%) [24].


Fig. 7.2
FDG PET/CT for restaging. A 56-year-old female underwent Whipple’s procedure for pancreatic adenocarcinoma involving body, followed by adjuvant chemotherapy; 6 months later, presented with rising CA19.9 levels, and hence was referred for PET/CT imaging. MIP image shows focal tracer uptake in the mid-abdomen (arrow), which corresponds to FDG-avid soft tissue (b–arrow) at the level of SMA origin (c–arrow) from abdominal aorta, thus representing local recurrence, with this being a typical pattern of local site recurrence
7.7 PET/CT to Detect Treat Response
PET combined with CECT plays a role in monitoring response to chemo- and radiation therapy in patients with unresectable pancreatic cancer [25, 26]. Significant reduction in FDG uptake may precede volumetric reduction at CT and may be proportional to the change in tumor size at subsequent follow-up examinations (Fig. 7.3). Therefore, earlier depiction of tumor response to therapy at FDG PET could influence the continuation or withdrawal of treatment [27]. Moreover, some recently published studies reported that FDG PET/CT might have prognostic value because tumors with a higher baseline SUVmax are more likely to recur in the early post-operative period. SUVmax is also an independent predictor for overall survival in patients with locally advanced pancreatic cancer [28, 29]. Postoperative inflammatory changes in the pancreas, radiation therapy, or stent placement may also cause some FDG uptake. To minimize these false-positive results, it is recommended that follow-up PET or PET/CT be performed at least 6 weeks after surgery [30].


Fig. 7.3
FDG PET/CT in treatment response evaluation. A 46-year-old female patient presented with adenocarcinoma involving pancreatic head which was non-resectable received 6# chemotherapy; PET/CT study was performed to assess treatment response. MIP images (baseline-a, posttreatment-b) show regression in focal tracer uptake in mid-abdomen, which is seen as significant regression in size with near-complete metabolic regression at the primary pancreatic site (baseline, with no new lesions elsewhere, on axial PET/CT (c-baseline, d-posttreatment)
7.8 PET Tracers for Other Pancreatic Neoplasms
7.8.1 68Ga-DOTA-PET/CT
Neuroendocrine tumors represent 1–2% of all pancreatic neoplasms [31]; nonfunctioning tumors now account for 60–80% of such tumors [32]. Insulinoma and gastrinoma are the most common functioning islet cell tumors, accounting for about 32 and 9% of cases, respectively. Functioning tumors are detected earlier in their clinical course, when they are generally small in size.
As many as 90% of nonfunctioning tumors are malignant at the time of diagnosis, with more indolent biologic behavior than pancreatic adenocarcinoma [33]. Well-differentiated NETs, termed “carcinoids ,” often express somatostatin receptors (SSTR), whereas poorly differentiated variants express GLUT receptors making these tumors FDG avid. SSTR-specific radionuclides like Ga68-DOTA-TOC/NOC/TATE are the most sensitive radionuclides for this subset of tumors. Versari et al. [34] reported that 68Ga DOTA-TOC PET/CT has accuracy comparable to those of endoscopic US and multidetector CT for depicting primary neuroendocrine tumors in the duodenopancreatic area, with a sensitivity of 87% and specificity of 83%.
7.8.2 68Ga-DOTA-Exendin-4 PET/CT
The most common cause of endogenous hyperinsulinemic hypoglycemia in adults is an insulinoma. Endogenous hyperinsulinemic hypoglycemia is biochemically diagnosed by a prolonged supervised fasting test in an inpatient setting [35]. Small size of tumors is a limitation for localization by conventional imaging. Methods like intra-arterial calcium estimation and venous sampling are sensitive; however, their invasive nature poses risk of complications. Benign insulinomas have a high concentration of glucagon-like peptide-1 receptors (GLP R 1), which are good targets for in vivo imaging [36]. Early results with 68Ga-DOTA-exendin-4 PET/CT, which localizes to GLP-R-1, have shown good sensitivity for detection of these lesions [37].
7.8.3 18F–FDOPA PET/CT
The most frequent catecholamine-producing tumors are pheochromocytomas, which arise from chromaffin cells of the adrenal medulla (80–85%) or extra-adrenal paraganglia (15–20%). Imaging techniques are used to localize the primary tumor and to search for metastases. In case of pheochromocytomas, most tumors are benign, but 10–20% are malignant. The most specific agent which localizes to catecholamine precursor dopamine receptors is a F-18-labeled compound, fluoro-L-dihydroxyphenylalanine (F-DOPA) [38]. It has better resolution, imaging characteristics, and sensitivity than I-131 MIBG SPECT scintigraphy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree