A. Type I hiatal hernia
B. Type II hiatal hernia
C. Type III hiatal hernia
D. Type IV hiatal hernia
2 A 63-year-old female presents with epigastric pain and nausea. A double-contrast upper GI study was performed. What is the correct diagnosis?


A. Type I hiatal hernia
B. Type II hiatal hernia
C. Type III hiatal hernia
D. Type IV hiatal hernia
3 A 50-year-old male presents with 10-year history of intermittent substernal chest pain. An esophagram is performed.

What is the most likely diagnosis?
A. Varices
B. Caustic ingestion
C. Gastroesophageal reflux disease (GERD)
D. Pill esophagitis
4 On these barium esophagram studies, which of the following findings is least likely to be associated with gastroesophageal reflux disease (GERD)?
A.

B.

C.

D.

5 A 56-year-old male presents to a primary care physician to establish care. He notes a history of weight gain over the past 5 years with increasing substernal burning chest pain and belching. The patient is placed on an acid suppression treatment plan, and a barium esophagram is performed 1 month later, at which point he reports improvement of symptoms. The following image is obtained. What is the next best step?

A. Follow the patient clinically as he is improving on medical therapy.
B. Recommend endoscopic evaluation with biopsy.
C. Refer to a surgeon for findings concerning for malignancy.
D. Obtain a 24-hour pH monitoring test to confirm suspicion of gastroesophageal reflux.
6 A 45-year-old male with a long history of heartburn has an esophagram. The following finding is persistent and unchanged on multiple views. What is the appropriate next step in management?

A. A CT of the abdomen should be performed to evaluate for evidence of cirrhotic liver disease and portal hypertension.
B. The finding is likely benign, the patient should continue acid suppression medical therapy, and no further workup is needed.
C. The finding is likely benign, but endoscopic evaluation is still indicated.
D. The finding is very concerning for malignancy and endoscopy with polypectomy is warranted.
A. Caustic ingestion
B. Esophageal carcinoma
C. Schatzki ring
D. Esophageal web
8a A 67-year-old man presents with a 10-year history of dysphagia and regurgitation. What is the most likely diagnosis?



A. Peptic stricture from GERD
B. Achalasia
C. Caustic ingestion
D. Progressive systemic sclerosis
E. Pseudoachalasia from esophageal cancer
8b A similar pattern to the findings in the previous example may be seen in infection with
A. Helicobacter pylori
B. Trypanosoma cruzi
C. Treponema pallidum
D. Wuchereria bancrofti
9 A 44-year-old female presents with several-month history of worsening substernal chest discomfort. A barium esophagram demonstrates loss of the peristaltic stripping wave from the level of the aortic arch inferiorly. The gastroesophageal junction is widely patulous, and free gastroesophageal reflux is noted. What diagnosis may be suggested?

A. Progressive systemic sclerosis
B. Achalasia
C. Presbyesophagus
D. Myasthenia gravis
11 A 32-year-old male with poorly controlled diabetes and dysphagia has a barium esophagram. What is the most likely diagnosis?

A. Cytomegalovirus esophagitis
B. Herpes simplex virus esophagitis
C. Glycogenic acanthosis
D. Candida esophagitis
E. Squamous papillomatosis
12 A 45-year-old man who has undergone allogenic bone marrow transplantation now presents with odynophagia. What is the most likely infectious etiology?


A. Cytomegalovirus
B. Herpes simplex virus
C. Candidiasis
D. Epstein-Barr virus
E. Human papillomavirus
13a A 40-year-old man suffered blunt trauma to the neck from a cap propelled off a high-pressure gas can. For respiratory distress, endotracheal and right chest tubes were emergently placed. Selected axial images from contrast-enhanced CT are shown.




What the most likely origin of pneumomediastinum in this patient?
A. Laryngeal fracture
B. Macklin phenomenon
D. Esophageal perforation
E. Traumatic intubation
13b The patient subsequently underwent this exam with water-soluble contrast injected via enteric tube. What is the next step?

A. Repeat injection with barium contrast
B. Bronchoscopy
C. Diagnostic endoscopy
D. Endoscopic stent placement
E. Thoracotomy
14 A 42-year-old male presents with chest pain after severe vomiting. He undergoes a fluoroscopic esophagram with water-soluble contrast followed by a CT. What portion of the esophagus is typically involved in this syndrome?


A. Left posterolateral wall of the midesophagus
B. Left posterolateral wall of the distal esophagus
C. Right posterolateral wall of the midesophagus
D. Right posterolateral wall of the distal esophagus
15 A 40-year-old woman was shot in the neck just above the sternal notch. The wound was explored and a surgical drain placed at the left aspect of the base of the neck. Small bullet fragments in the right neck base were not removed. Spot images from subsequent swallow study are shown below.


Which of the following statements is TRUE?
A. Esophageal injuries are seen at a rate comparable to vascular injuries following penetrating trauma.
B. Gunshot wounds are less common than iatrogenic causes of penetrating esophageal trauma in the neck.
C. Contrast swallow studies for intrathoracic esophageal perforation are associated with a 10% false-positive rate.
D. The next step would be to rotate the patient 90 degrees to right posterior oblique and repeat the exam with Gastrografin.
E. Endoscopic esophageal stent placement is the preferred treatment method for this hemodynamically stable patient.
A. Chronic indwelling nasogastric tube
B. Gastroesophageal reflux and Zollinger-Ellison syndrome
C. Caustic ingestion
D. Eosinophilic esophagitis
17a A 36-year-old male with history of hematemesis and abdominal distention presents for evaluation with a double-contrast upper GI study and contrast-enhanced abdominal MRI. What is the salient finding that may be contributing to his symptoms?


A. Esophageal carcinoma
B. Gastroesophageal varices
C. Mediastinal lymphadenopathy
D. Ménétrier disease
17b When performing an esophagram, which technique will make the varices more apparent?
A. Upright double-contrast view
B. Semiprone (right anterior oblique) full column esophagus with full distention
C. Semiprone (right anterior oblique) collapsed esophagus with mucosal relief
D. Upright collapsed esophagus
18a A 67-year-old male with a recent diagnosis of cancer in the midesophagus (squamous cell) on endoscopy undergoes staging studies. What is the main role of CT in the staging of his cancer?



A. The CT helps distinguish between invasion of the submucosa and muscularis propria.
B. The CT assesses invasion of local mediastinal structures.
C. The CT identifies a malignant distal esophageal node.
D. The CT identifies a potential percutaneous approach to a nodal biopsy.
18b A PET-CT scan was also performed. What is the main role of the PET-CT in the staging of his cancer?



A. The PET-CT identifies uptake in mediastinal nodes adjacent to the primary tumor.
B. The PET-CT assesses depth of tumor invasion into the wall of the esophagus.
C. The PET-CT identifies a potential distant metastatic focus in the pleural space.
D. The PET-CT distinguishes between left gastric and celiac nodal disease.
19 A 22-year-old male presents with long history of solid-food dysphagia and occasional food impaction. He undergoes a barium esophagram. What is the most likely diagnosis?

A. Peptic strictures from GERD
B. Caustic ingestion
C. Pill esophagitis
D. Eosinophilic esophagitis
20a A 75-year-old male with a 50-pack-year history of smoking and alcoholic liver disease presents with a 2-month history of dysphagia to solid foods. A barium esophagram is performed. What is the most likely diagnosis?

A. Food impaction
B. Esophageal leiomyoma
C. Esophageal squamous cell carcinoma
D. Esophageal varices
20b The most significant risk factors for development of esophageal adenocarcinoma are:
A. Obesity, GERD, and cigarette smoking
B. Alcohol and cigarette smoking
C. High-fat consumption and alcohol
D. Helicobacter pylori infection, alcohol, and cigarette smoking
21 A 29-year-old male with a history of dysphagia has a double-contrast barium esophagram. What is the most likely diagnosis?

A. Granular cell tumor
B. Fibrovascular polyp
C. Gastrointestinal stromal tumor (GIST)
D. Leiomyoma
22 An 82-year-old female has symptoms of severe dysphagia to liquids and solids. The patient undergoes a single-contrast esophagram. Which antecedent history may be associated with the findings seen?

A. Prolonged ICU stay with indwelling nasogastric tube
B. History of bullous skin disorder
C. Chronic severe GERD
D. Radiation therapy for lymphoma
E. Zollinger-Ellison syndrome
23 A 31-year-old female complains of cervical dysphagia. She is otherwise healthy. A pharyngogram is performed, and manometric measurements demonstrate increased upper esophageal sphincter (UES) pressure at rest and failure of the UES to completely relax. What additional condition is likely to be present?

A. Zenker diverticulum
B. Gastroesophageal reflux disease
C. Cranial nerve dysfunction
D. Recurrent pneumonias from aspiration
24 An 85-year-old female presents with a history of dysphagia and regurgitation of undigested material. She undergoes a barium pharyngoesophagram. What is the most likely diagnosis?


A. Killian-Jamieson diverticulum
B. Lateral pharyngeal pouch
C. Lateral pharyngeal diverticulum
D. Zenker diverticulum
25 A 45-year-old male presents with a history of chronic dysphagia to liquids and solids. In classic primary achalasia, what will be the most typical finding on esophageal manometry?

A. Hyperperistalsis in the lower two-thirds of the esophagus
B. Abnormally low resting pressure at the lower esophageal sphincter
C. Simultaneous contractions in multiple segments of the esophagus
D. Incomplete relaxation of the lower esophageal sphincter
26a A 65-year-old female with recent stroke presents with dysphagia. A barium swallow is requested by the clinician, and an esophagram is performed with thin barium. The following spot films obtained after the initial swallow of barium. What do the findings represent?


A. High cervical esophageal stricture
B. Cricopharyngeal achalasia
C. Lateral pharyngeal pouches
D. Aspiration
26b Label the following structures A to H. Each answer may be used once, more than once, or not at all.


A. Esophagus
B. Laryngeal ventricle
C. Laryngeal vestibule
D. True cord
E. False cord
F. Trachea
G. Pyriform sinus
H. Epiglottis
I. Vallecula
26c Which action listed below is not involved in the pharyngeal phase of a normal swallow?
A. Elevation of the soft palate
B. Depression of the hyoid bone with posterior and inferior movement of the larynx
C. Epiglottic inversion
D. Adduction of the vocal cords
E. Relaxation of the upper esophageal sphincter
27 A 79-year-old female with 80-pack-year history of smoking and stroke presents for a modified swallow study to evaluate for aspiration. The following image is obtained:

An endoscopic examination and CT scan of the neck performed following the swallow study fails to reveal a mass. What is the most likely explanation?
A. The finding represents a pseudomass due to patient head positioning.
B. The mass likely represented retropharyngeal abscess that responded by the time of the follow-up imaging.
C. The pseudomass represents the normal side of the pharynx.
D. The lesion was missed on endoscopy.
ANSWERS AND EXPLANATIONS
1 Answer A.Spot image from a double-contrast esophagram demonstrates upward herniation of the stomach into the chest with superior migration of the gastroesophageal junction. This is compatible with a type I hiatal hernia, also called a sliding hiatal hernia. Type I hiatal hernias account for 85% to 95% of all hiatal hernias and are associated with diffuse weakening of the phrenoesophageal membrane, which normally fixes the distal esophagus near the hiatus. This laxity allows the upward displacement of the gastroesophageal junction and stomach into the chest through the diaphragmatic hiatus. Patients with type I hiatal hernias can also have diminished lower esophageal sphincter tone and therefore often present with symptoms of gastroesophageal reflux.
The other types of hernias listed (types II to IV) are paraesophageal hernias and will be discussed in a later question.
References: Abbara S, Kalan MM, Lewicki AM. Intrathoracic stomach revisited. AJR Am J Roentgenol 2003;181(2):403–414.
Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol 2008;22(4):601–616.
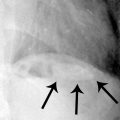
2 Answer B.Spot image from double-contrast upper GI study demonstrates a normally positioned gastroesophageal (GE) junction (image on left) with adjacent herniation of the gastric fundus above the diaphragm (image on the right). This is compatible with a type II paraesophageal hiatal hernia. Paraesophageal hernias result from a focal defect in the phrenoesophageal membrane that provides a small opening for upward gastric herniation, generally beginning with the gastric fundus.
In the surgical literature, hiatal hernias are generally classified into two major groups: sliding and paraesophageal hernias.
Types of Hiatal Hernias

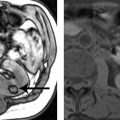
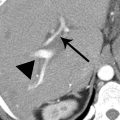
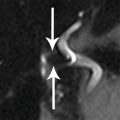
The above example of the type III hernia demonstrates elevation of the GE junction above the level of the diaphragmatic hiatus as well as herniation of a segment of the fundus adjacent to the GE junction and distal esophagus. The type IV hernia images show a large hernia containing fat and a portion of the colon.

Type III hiatal hernia (mixed).

Type IV hernia coronal.

Type IV hernia axial.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree