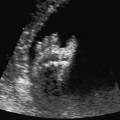
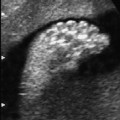
14 Placenta, Cord, and Amniotic Fluid Definition: Benign vascular tumors of the placenta, usually single, encapsulated and round-shaped tumors situated within the placenta. Incidence: This is the most frequent placenta tumor, detected histologically in 1% of all placentas. Clinical history/genetics: Sporadic occurrence. Ultrasound findings: The fetus usually shows normal development. Rarely, fetal hydrops may result secondary to arteriovenous shunting within the tumor, which causes increased volume overload to the fetal heart. The earliest signs are hepatosplenomegaly and pericardial effusion. Pleural effusion, ascites, and skin edema may also result. Hydramnios is frequently present. Subsequent fetal anemia often leads to growth restriction. Chorioangioma can be detected as a vascular tumor within the placenta, located mostly near the insertion of the umbilical cord, and protruding into the amniotic cavity. Chorioangiomas causing hemodynamic complications are usually larger than 6 cm. They may even develop in the later stages of pregnancy. Clinical management: Regular scans are recommended to detect the development of fetal hydrops and growth restriction as early as possible. Chorioangioma may even regress spontaneously during the course of pregnancy. The resulting hydramnios may lead to premature labor and delivery. Procedure after birth: Unexpected neonatal anemia may be due to chorioangioma. Prognosis: Most chorioangiomas do not have any pathophysiological relevance. Very rarely, vessel anastomosis within the tumor overload the fetal heart, causing fetal hydrops. Fig. 14.1 Chorioangioma. A large chorioangioma on the surface of placenta at 30 weeks’ gestation. References Bashiri A, Maymon E, Wiznitzer A, Maor E, Mazor M. Chorioangioma of the placenta in association with early severe polyhydramnios and elevated maternal serum HCG: a case report. Eur J Obstet Gynecol Reprod Biol 1998; 79: 103–5. Cardwell MS. Antenatal management of a large placental chorioangioma: a case report. J Reprod Med 1988; 33: 68–70. D’Ercole C, Cravello L, Boubli L, et al. Large chorioan-gioma associated with hydrops fetalis: prenatal diagnosis and management. Fetal Diagn Ther 1996; 11: 357–60. Gitsch G, Deutinger J, Bernaschek G. Prenatal diagnosis of placental tumor using Doppler sonography. Geburtshilfe Frauenheilkd 1990; 50: 986–8. Khong TY. Chorangioma with trophoblastic proliferation. Virchows Arch 2000; 436: 167–71. Lampe S, Butterwegge M, Krech RH. Chorioangiomatosis of the placenta: diagnosis and obstetrical management. Zentralbl Gynäkol 1995; 117: 101–4. Lopez HB, Kristoffersen SE. Chorioangioma of the placenta. Gynecol Obstet Invest 1989; 28: 108–10. Noack F, Germer U, Gembruch U, Feller AC, Horny HP. [Uteroplacental insufficiency in chorangiomatosis; in German]. Zentralbl Gynäkol 2002; 124: 116–9. Ogino S, Redline RW. Villous capillary lesions of the placenta: distinctions between chorangioma, chorangiomatosis, and chorangiosis. Hum Pathol 2000; 31: 945–54. Reinhart RD, Wells WA, Harris RD. Focal aneurysmal dilatation of subchorionic vessels simulating chorioan-gioma. Ultrasound Obstet Gynecol 1999; 13: 147–9. Definition: Increased amount of amniotic fluid: amniotic fluid index (AFI) above 25 cm, or largest depot above 8 cm. At the due date, the amniotic fluid volume is more than 2 L. Incidence: About 1% of all pregnancies. Clinical history/genetics: Diabetes mellitus. Etiology: Fetal anomalies are responsible in up to 20% of cases: atresia of the esophagus, duodenal stenosis, jejunal stenosis, disturbance of swallowing reflex due to muscular or neural causes, displacement of the mediastinum as in CCAM or diaphragmatic hernia, some fetal syndromes (Pena–Shokeir syndrome, and rarely Neu–Laxova syndrome). It may also occur in association with fetal hydrops and congenital infections. Ultrasound findings: Amniotic fluid index of above 25 cm, or the largest depot measuring above 8 cm. Development of hydramnios is rare prior to 24–25 weeks, even if fetal anomalies are present. Clinical management: Detailed scan is mandatory. Maternal diabetes mellitus should be excluded. Search for infections (TORCH), possibly karyotyping. Therapeutic amniocentesis for aspiration of amniotic fluid is recommended to relieve maternal abdominal pressure and prevent premature delivery, if there is dyspnea or premature contractions, which affect cervical competence. Prognosis: This depends on the causative factor. The perinatal mortality rate is increased due to premature birth and complications arising during labor (dystocia, umbilical cord prolapse). References
Chorioangioma

Hydramnios
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree