Plantar Fasciitis and Other Abnormalities of the Plantar Fascia
Anatomic Considerations
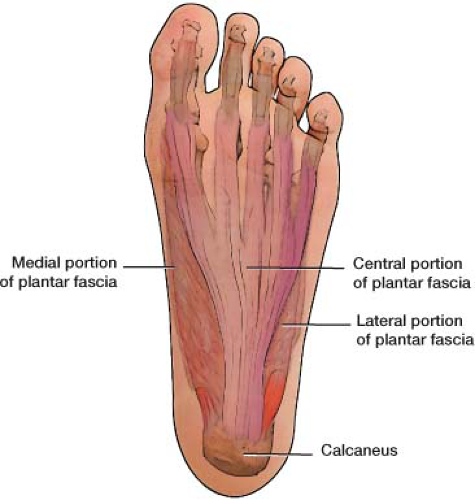
The plantar fascia is made up of thick, longitudinally oriented connective tissue that is tightly attached to the plantar skin (Fig. 16.1). It attaches to the medial calcaneal tuberosity and then runs forward, dividing into five bands, one going to each toe (Fig. 16.2). The plantar fascia provides dynamic support to the arch of the foot, tightening as the foot bears weight.
Clinical Correlates
Plantar fasciitis is a clinical syndrome characterized by pain and tenderness over the plantar surface of the calcaneus made immediately worse by dorsiflexion of the toes. Occurring twice as often in women, plantar fasciitis is thought to be caused by an inflammation of the plantar fascia. Inflammation of the plantar fascia can occur alone or be part of a systemic inflammatory condition, such as rheumatoid arthritis, Reiter syndrome, or gout. Obesity also seems to predispose to the development of plantar fasciitis, as does going barefoot or wearing house slippers for prolonged periods. High-impact aerobic exercise also has been implicated.
Pain on palpation of the insertion of the plantar fascia on the plantar medial calcaneal tuberosity is a consistent finding in patients with plantar fasciitis as is exacerbation of pain with active resisted dorsiflexion of the toes. Patients suffering from plantar fasciitis will also exhibit pain on deep palpation of the plantar fascia, especially when the toes are dorsiflexed pulling the plantar fascia taunt. The pain of plantar fasciitis is most severe on taking the first few steps after having not borne weight and is made worse by prolonged standing or walking.
Plantar fibromatosis, which is also known as Ledderhose disease, is a common cause of heel and foot pain and functional disability (Fig. 16.3). It is caused by a progressive fibrosis of the plantar fascia and was first described by Dr. George Ledderhose in 1894. Early symptoms of plantar fibrosis are tender fibrotic nodules along the course of the plantar fascia with the initial nodules first appearing at the medial aspect of the arch of the foot (Figs. 16.4 and 16.5). Frequently, the painful, fibrotic nodules of the plantar surface that are seen early in the course of the disease are misdiagnosed as plantar warts, corns, or ganglion cysts (Fig 16.6).
As the disease progresses, these isolated nodules begin to coalesce. Untreated, flexion contractures of the toes in a manner analogous to Dupuytrens contraction will develop. The pain of plantar fibrosis tends to burn itself as the disease progresses.
The exact cause of Dupuytren contracture remains unknown although the disease seems to have a genetic basis with an autosomal dominant inheritance pattern with variable penetrance. A biochemical pathogenesis has been hypothesized which suggests that excess deposition of Type I collagen combined with abnormal myofibroblast formation and increased levels of beta-catenin are responsible for the disease. Dupytren contraction occurs with increased frequency in individuals of European descent with a gender predilection approaching ten males for every female affected. The disease rarely occurs before the fourth decade. Diabetes, smoking, cirrhosis of the liver, chronic barbiturate use, trauma to the palmar fascia, and alcoholism are risk factors.
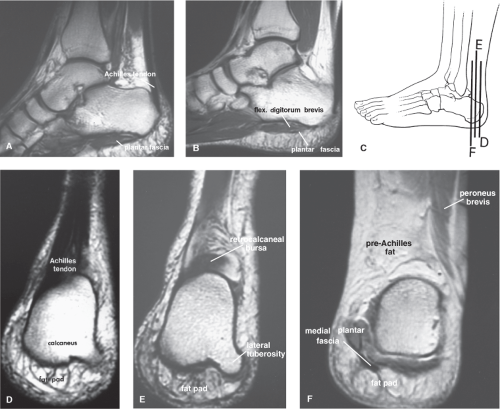
Plain radiographs are indicated in all patients who present with heel and foot pain (Fig. 16.7). Based on the patient’s clinical presentation, additional testing may be indicated, including complete blood cell count, sedimentation rate, and antinuclear antibody testing. MRI and/or ultrasound imaging of the ankle is indicated if plantar fasciitis, rupture, or joint instability is suggested or the diagnosis is in question (Figs. 16.8 to 16.15). Radionuclide scanning is useful to identify stress fractures of the calcaneus and foot not seen on plain radiographs and may aid in the diagnosis of plantar fasciitis as there may be increased uptake of radionucleotide at the insertion of the plantar fascia at the calcaneus (Fig. 16.16).
Ultrasound Technique
To perform ultrasound evaluation of the plantar fascia, the patient is placed in the prone position with the patient’s ankle hanging off the edge of the table. With the patient in the above position, a high-frequency linear ultrasound transducer is placed in a longitudinal plane with the inferior portion of the
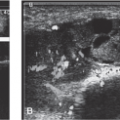
ultrasound transducer over plantar surface of the foot with the superior end of the transducer centered on the anterior portion of the calcaneus. An ultrasound survey scan is then taken (Fig. 16.17). The calcaneus and linear plantar fascia is identified at its insertion on the calcaneus (Fig. 16.18). When the insertion of the plantar fascia is identified, the insertion is evaluated for tendinopathy and then the plantar fascia is evaluated along its length for tears, rupture, and fibromatosis, and tumors that may produce symptoms that may mimic plantar fasciitis (Figs. 16.19 to 16.34). Recent reports suggest that ultrasound elastography may improve the diagnostic accuracy of plantar fasciitis (Figs. 16.35 and 16.36).
ultrasound transducer over plantar surface of the foot with the superior end of the transducer centered on the anterior portion of the calcaneus. An ultrasound survey scan is then taken (Fig. 16.17). The calcaneus and linear plantar fascia is identified at its insertion on the calcaneus (Fig. 16.18). When the insertion of the plantar fascia is identified, the insertion is evaluated for tendinopathy and then the plantar fascia is evaluated along its length for tears, rupture, and fibromatosis, and tumors that may produce symptoms that may mimic plantar fasciitis (Figs. 16.19 to 16.34). Recent reports suggest that ultrasound elastography may improve the diagnostic accuracy of plantar fasciitis (Figs. 16.35 and 16.36).
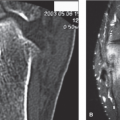
 FIGURE 16.7 Stippled calcifications in the plantar fascia seen on a lateral radiograph. (From Monto RR. Platelet-rich plasma and plantar fasciitis. Sports Med Arthrosc 2013;21(4):220–224.) |
 FIGURE 16.8 Lateral radiograph of the calcaneus demonstrates an avulsed osteophyte (arrow) in a patient with chronic heel pain with a recent acute exacerbation. (From Berquist TH. Imaging of the Foot and Ankle. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:174.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|