Abstract
FDG avidity in the pleura may be malignant, such as metastases and mesothelioma, or benign, such as postpleurodesis inflammation. Corresponding CT findings, such as high attenuation from prior talc pleurodesis, may assist in making this distinction.
Keywords
FDG, PET/CT, pleura, pleural metastases, mesothelioma, pleurodesis
The pleura are the pair of membranous linings surrounding the lungs. The visceral pleura covers each lung surface, and the parietal pleura covers the inner surface of the thoracic cavity. Normally, the visceral and parietal pleura oppose each other, have negligible material between them, and are so thin as to be nearly imperceptible on computed tomography (CT). Thus, if you can see the pleura between lung and chest wall, it is abnormal. Pleural abnormalities are often associated with pleura effusions, which may obscure underlying solid pleural masses.
The differential for pleural abnormalities includes malignancies (metastases, lymphoma, mesothelioma) and benign (empyema, asbestos-related pleural disease, fibrous tumor, post-pleurodesis inflammation) etiologies.
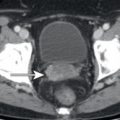
Postpleurodesis Inflammation
Patients with large volume pleural effusions may undergo pleurodesis to help prevent future pleura fluid accumulation. The effectiveness of pleurodesis derives from the pleuritis produced by chemical irritation from talc which is introduced between the parietal and visceral pleural layers. The talc has high attenuation and persists indefinitely following the procedure. If a pleural lesion shows high attenuation on CT in a patient with a history of pleurodesis, this is consistent with postpleurodesis reactive inflammation because less than 10% of pleural malignancies develop calcifications. The chemical irritation from talc also may persist indefinitely, resulting in markedly 18F-fluorodeoxyglucose (FDG)-avid pleural thickening with areas of high attenuation. This may persist for years or decades and should not be confused with FDG-avid pleural metastases. Postpleurodesis inflammation is normally not associated with a pleural effusion. Thus FDG-avid pleural thickening with areas of high attenuation on CT, but without associated pleural effusion, is consistent with benign postpleurodesis inflammation and may persist indefinitely ( Fig. 9.1 ). Follow-up imaging demonstrating new areas of pleural thickening or new pleural effusions is suspicious for recurrent malignancy.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree