MR neurography (MRN) has become a cornerstone in diagnosing and managing plexus and peripheral nerve disorders. This review explores recent advancements in MRN, emphasizing 3T imaging, coil selection, fat and vascular suppression strategies, and deep learning-based reconstruction for enhanced image resolution. This review focuses particularly on the technical considerations of imaging different anatomic regions including the brachial plexus, lumbosacral plexus, and peripheral nerve of the extremities. Looking ahead, the implementation of 7T MR imaging, the integration of quantitative diffusion imaging, and further standardized protocols promises to refine MRN’s role in clinical practice.
Key points
- •
High-resolution imaging with 3T MR imaging, advanced coils, proper combination of 2 dimensional (2D) and 3D imaging, and effective fat and vascular suppression techniques are essential for detailed nerve visualization in MR neurography.
- •
MR neurography of brachial plexus benefits from tailored 3D imaging protocols using fast spin-echo (FSE) short inversion time inversion recovery (STIR) sequence and black blood preparation pulse.
- •
MR neurography of lumbosacral plexus requires 3D imaging protocol with robust vascular suppression techniques including dual-echo steady-state sequence and FSE STIR sequence with black blood preparation pulse.
- •
MR neurography of peripheral nerve in extremities is limited in vascular suppression due to stagnant blood flow and has benefits in 2D imaging to evaluate the fascicular structure of the nerve.
| BP | brachial plexus |
| CHESS | chemical shift (spectral) selective |
| 2D | 2 dimensional |
| 3D DW-PSIF | 3D diffusion-weighted reversed fast imaging with steady state precession |
| 3D | 3 dimensional |
| DANTE | delay alternating with nutation for tailored excitation |
| DESS | dual-echo steady-state |
| DLR | deep learning reconstruction |
| DTI | diffusion tensor imaging |
| DWI | diffusion-weighted imaging |
| FOV | field of view |
| FSE | fast spin-echo |
| LSP | lumbosacral plexus |
| MIP | maximum intensity projection |
| MRN | MR neurography |
| MSDE | motion-sensitized driven equilibrium |
| MSI | multispectral imaging |
| SHINKEI | sheath signal increased with inked rest-tissue RARE imaging |
| SNR | signal-to-noise ratio |
| SPAIR | spectral adiabetic inversion recovery |
| STIR | short inversion time inversion recovery |
| T1wI | T1-weighted imaging |
| T2wI | T2-weighted imaging |
Introduction
MR neurography (MRN) is an imaging technique designed to augment the signal intensity of peripheral nerves while suppressing signals from surrounding tissues. It was first described by Howe and colleagues in the early 1990s. Since then, MRN has evolved into a valuable diagnostic tool for patients with neuropathies, gaining broader clinical adoption over time. , In the early 2010s, with the widespread availability of 3T MR imaging systems, detailed visualization of peripheral nerves and their pathologies became possible. However, challenges such as inhomogeneous fat suppression, vascular contamination, long scan times, and blurring persisted.
The recent resurgence of interest in MRN has been driven by substantial technological advancements addressing these challenges, leading to superior image quality and broader clinical and research applications. Central to this progress are improvements in MR imaging hardware. Advancements in gradient and radiofrequency systems, along with enhanced shimming techniques, have enabled a more homogeneous magnetic field and effective fat suppression. The development of flexible, anatomically adaptable coils with high-density elements have further contributed to improve image quality. These hardware developments are complemented by faster acceleration techniques, optimized flip angle design, and improved vascular suppression methods, collectively improving the visibility of nerve signal while suppressing background tissue signal.
This article discusses sequence possibilities and recent advances fueling the renewed focus on MRN. It aims to establish a technological foundation for subsequent discussions of disease-specific and anatomy-specific applications of this powerful imaging modality.
General imaging techniques
Signal-to-Noise Ratio and Resolution
MRN is essential for evaluating complex nerve structures such as the brachial plexus (BP), lumbosacral plexus (LSP), and extremity nerves. Nerves, composed of small fascicles with elongated courses, require high spatial resolution imaging over a wide field of view (FOV) to assess various pathologic conditions. Imaging at 3.0T is routinely recommended for MRN due to its approximately 1.4 fold higher signal-to-noise ratio (SNR) compared to 1.5T MR imaging, enabling higher spatial resolution. Additionally, optimal coil selection is crucial for maintaining SNR across a broad FOV. Dedicated multichannel-phased array surface coils are preferred, though coil selection can still be challenging for BP imaging due to the anatomic complexity of the BP region.
Pathologic nerve changes are assessed in 2 ways: fascicular structure assessment in the orthogonal plane and nerve course evaluation in the longitudinal plane. , Two dimensional (2D) fast spin-echo (FSE) T2-weighted imaging (T2wI) provides high in-plane spatial resolution for detailed fascicular evaluation, while T1-weighted imaging (T1wI) delineates nerve anatomy from surrounding fat ( Fig. 1 ). Proton density-weighted imaging offers improved SNR while providing contrast resolution between nerves and surrounding fat, serving as an alternative to T1wI, particularly for BP imaging. Additionally, 2D imaging is valuable for identifying muscle denervation changes. In contrast, isotropic 3 dimensional (3D) MRN provides superior through-plane resolution, minimizing partial volume averaging artifacts and allowing a detailed evaluation of focal morphologic changes like hourglass-like constrictions. It also enables multi-planar reformation and maximum intensity projection (MIP) for an overview of the nerve course and preoperative planning.

MRN usually demands prolonged scan times to achieve spatial resolution over a wide FOV while incorporating fat and vascular suppression techniques. Acceleration techniques such as parallel imaging and compressed sensing, have been utilized to reduce scan time, yet result in SNR penalties. Recently, deep learning reconstruction (DLR) has been increasingly applied to various MR imaging sequences to overcome the limitations of conventional acceleration techniques. In MRN, DLR has also been successfully implemented in 2D FSE extremity nerve imaging, 3D FSE BP imaging, and 3D FSE and 3D dual-echo steady-state (DESS) LSP imaging.
Fat Suppression
Fat suppression is important in MRN because fat appears hyperintense on T2wI due to its longer T2 relaxation time compared to nerves, which can obscure nerve pathologies if not suppressed. Fat suppression techniques are categorized into 3 types: chemical shift (spectral) selective (CHESS) fat saturation, inversion recovery pulse sequences (eg, short inversion time inversion recovery [STIR]), and the chemical shift-based, Dixon technique. CHESS, which relies on the resonance frequency difference between fat and water, is less effective under conditions of high B0 inhomogeneity. This limitation makes CHESS generally less favored for imaging large FOVs and the complex structure of the plexi.
In contrast, STIR is the most robust fat suppression method in MRN. , , It nullifies fat signal using inversion recovery time optimized for T1 relaxation time of fat, making it relatively insensitive to B0 inhomogeneities. However, STIR has drawbacks, including low SNR and long scan time. Spectral adiabetic inversion recovery (SPAIR) offers an alternative, maintaining higher SNR despite inferiority in homogeneous fat suppression compared to STIR.
Dixon is also a widely implemented fat suppression method, using the difference in precession frequencies between fat and water. It is largely insensitive to B0 and B1 field inhomogeneities, providing homogenous fat suppression without SNR loss.
Lastly, water excitation technique is based on using 2 chemically selective radiofrequency (RF) pulses with an intervening time lag, to selectively stimulate the water protons by the second pulse. , It is commonly used in gradient echo (GRE)-based sequences, due to high SNR and resistance to B1 inhomogeneity.
Vascular Suppression
In non-contrast-enhanced MRN, vascular suppression relies on diffusion gradients to suppress the signals from moving protons. Steady-state sequences, such as 3D diffusion-weighted reversed fast imaging with steady state precession (3D DW-PSIF) and 3D DESS, are effective for improved nerve delineation by reducing vascular signal interference. 3D DW-PSIF sequence enhances nerve visibility by preferentially sampling spin-echo-like components containing heavily T2-weighted signal due to the prolonged TE. Moreover, the combination of diffusion gradients further suppresses vascular signal. , In contrast, the 3D DESS sequence utilizes 2 echoes, free induction decay and spin-echo-like component, to generate a single image. In DESS, vascular signals are suppressed as moving blood spins experience phase mismatches between 2 echoes, while static nerve tissue maintains phase coherence. Additionally, the short T2∗ relaxation of deoxyhemoglobin in venous blood contributes to signal intensity reduction, as seen in GRE-based sequences.
Black blood preparation techniques, such as motion-sensitized driven equilibrium (MSDE) technique, have been used to dephase vascular flow signal in 3D FSE STIR sequence. , MSDE technique employs symmetric motion-sensitizing gradient pairs around a refocusing pulse of diffusion preparation to dephase vascular flow signals, while amplifying nerve signals via a flip-back pulse that restores stationary magnetization. Improved MSDE technique, in which a second refocusing pulse is added to optimize vascular suppression, has been incorporated into nerve-sheath signal increased with inked rest-tissue RARE imaging (SHINKEI) protocol with SPAIR as a fat suppression technique. , Crusher gradients in FSE readouts are often used to suppress stimulated echoes formed after the second refocusing radiofrequency pulse increasing vascular signal suppression when combined with MSDE technique. Delay alternating with nutation for tailored excitation (DANTE) is another block blood preparation technique, which uses trains of low flip angle pulses along the direction of flow with short interpulse repetition times, resulting in significant attenuation of flowing spins. , However, despite the potentials for improved suppression of slow vascular flow, MSDE and crusher gradient utilization face challenges, including increased sensitivity to B1 inhomogeneities, reduced SNR, motion artifacts, and image blurring from increased FSE echo spacing.
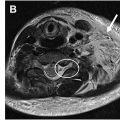
Contrast-enhanced MRN provides more robust vascular suppression. Intravascular gadolinium shortens the T2 relaxation time of vessels to levels similar to that of fat. As a result, 3D FSE STIR after contrast administration simultaneously suppresses signals from both fat and vessels. An additional advantage of contrast-enhanced 3D FSE STIR is its ability to nullify gadolinium-enhanced lymph nodes, which significantly improves the quality of MIP images, particularly in BP MRN. However, the value of using gadolinium should be carefully considered, as gadolinium-enhanced 2D FSE T1wI may not be consistently helpful in detecting nerve pathology or denervation myopathy. Also, careful interpretation is required as pathologic nerves with blood–nerve barrier breakdown in case of severe damage or tumor infiltration may become invisible on gadolinium-enhanced 3D FSE STIR ( Fig. 2 ). Ferumoxytol, a supraparamagnetic iron oxide nanoparticles, offers a strong T2 shortening effect and prolonged intravascular retention time compared to gadolinium. It allows robust vascular suppression, flexible MR acquisition, and compatibility with various fat suppression techniques. , Due to its delayed extravasation, the suppression of enhancing pathologic nerves is likely less pronounced than that with gadolinium-enhanced 3D FSE STIR. In a recent BP MRN study using ferumoxytol, low-dose injection was sufficient to acquire high nerve-to-vessel contrast ratio without additional crusher gradient. However, this remains an off-label use for MR imaging contrast media, and slow infusion is necessary to minimize the rare risk of anaphylaxis.

Metallic Artifact Reduction
Metal artifacts are induced by strong magnetic susceptibility of metallic hardware. When planning MRN for patients with metallic implants, it is important to review the type and location of the hardware relative to the target nerve. Alternative imaging modalities, such as ultrasound, should also be considered. While 1.5T MR imaging is generally preferred to a 3.0T MR imaging to reduce the metal artifact, 3.0T MR imaging remains a better option for MRN due to its sufficient SNR and high spatial resolution required to assess nerve. , Dixon and STIR are suitable fat suppression techniques in the presence of metal, whereas vascular suppression techniques using GRE sequences should be avoided. Conventional metal artifact reduction strategies using high receiver bandwidth can reduce artifacts but may decrease SNR. Advanced approaches include 3D multispectral imaging (MSI) techniques like slice-encoding for metal artifact correction and multiacquisition variable resonance image combination, which effectively reduce through-plane artifacts. However, 3D MSI techniques should be used in caution, because it often results in lower image resolution and lengthens scan time.
Special technical considerations in different anatomic regions
Brachial Plexus
The BP typically originates from the ventral C5–T1 spinal nerve roots and branches into peripheral nerves, traversing certain anatomic landmarks, including the interscalene triangle and the first rib. Due to its circuitous course through the neck, shoulder, and axilla, BP MRN poses a few challenges. First, there is no dedicated receiver coil to yield the sufficient SNR to image the BP. Second, inherent B0 and B1 magnetic field inhomogeneity in the region of the BP causes inhomogenous fat suppression. Third, chest wall motion during respiration leads to image degradation.
Unilateral BP imaging is generally preferred over bilateral imaging unless bilateral disease involvement is suspected, as unilateral FOV allows for a more targeted assessment of nerve pathologies extending to the proximal terminal branches. To address B0 and B1 magnetic field inhomogeneities in unilateral BP MRN, coil optimization is essential. While a neurovascular coil combined with anterior semi-flexible body and posterior spine coils is recommended for bilateral BP MRN, it has insufficient lateral coverage for unilateral BP imaging to its terminal branches. Instead, placing a smaller semi-flexible coil over the shoulder and the neck has an advantage of improved SNR for unilateral BP MRN ( Fig. 3 ). However, maintaining coil position during the scan can be challenging, requiring the use of straps and cushions to secure the coils. If extra flexible array coils are available, a conformal setup tailored to the BP region can further improve image quality.

Regarding fat suppression for 2D FSE T2wI, the Dixon technique provides more uniform fat suppression than STIR, particularly under B0 and B1 inhomogeneities. A multiecho FSE-modified Dixon technique, which captures in-phase and opposed-phase echoes within a single repetition time, can further reduce scan time compared to conventional FSE Dixon. However, for 3D FSE T2wI, STIR remains preferable due to the long scan time and echo train length of Dixon. , For vascular suppression, non-enhanced 3D FSE STIR sequences with MSDE preparation with crusher gradients has shown improved nerve conspicuity compared to sequences without these techniques ( Fig. 4 ). A recent study using the 3D SHINKEI sequence demonstrated high accuracy and specificity in diagnosing traumatic BP injuries. Contrast-enhanced 3D FSE STIR offered superior nerve delineation and resolution in BP MRN compared to non-enhanced sequences, suppressing vessels and cervical lymph nodes. ,

To minimize respiratory motion artifacts, prone positioning and prospective respiratory triggering can be beneficial, particularly when evaluating nerves near the thoracic wall, such as the long thoracic nerve. , Prospective respiratory triggering has been shown to improve nerve conspicuity and especially advantageous for imaging the infraclavicular segment of the BP. , Our recommended 3.0T BP MRN protocol is outlined in Table 1 .
| Sequence | 2D T2w-FSE | 2D T2w-FSE | 2D PDw-FSE | 3D T2w-FSE | 2D T1w-FSE |
|---|---|---|---|---|---|
| Orientation | Coronal | Axial | Oblique sagittal | Coronal | Oblique sagittal |
| TR/TE/TI (ms) | 3500/94/- | 4610/97/- | 3500/7.2/- | 2600/170/250 | 692/11/- |
| FOV (cm) | 30.0 | 26.0 | 26.0 | 30.0 | 26.0 |
| Matrix size (FE/PE) | 512×256 | 512×256 | 400×280 | 384×384 | 512×256 |
| Slice thickness/gap (mm) | 3/- | 4/- | 4/- | 1/- | 4/- |
| Slices | 35 | 45 | 40 | 120 | 40 |
| Echo train length | 15 | 15 | 9 | 174 | 4 |
| Bandwidth (Hz/pixel) | 514 | 514 | 298 | 330 | 362 |
| Fat suppression technique | Dixon | Dixon | – | IR | Dixon |
| Parallel imaging factor | 3 | 3 | 3 | 4 | 2 |
| Gadolinium contrast | N | N | N | N/ a Y | a Y |
| Vascular suppression | – | – | – | b MSDE | |
| Crusher gradient | – | – | b 893/0/0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree