KEY FACTS
Terminology
- •
Portal hypertension: Pressure gradient > 12 mm Hg between main portal vein (PV) and IVC &/or hepatic veins
Imaging
- •
Ultrasound for 1st-line evaluation of portal hypertension
- ○
Best tool for dynamic evaluation of portal venous system
- ○
- •
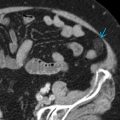
Large main PV
- ○
> 16 mm in maximal diameter
- ○
- •
Presence of portosystemic collateral vessels
- •
May also see slow flow in main PV, to-and-fro or bidirectional PV, or reversal of flow in PVs
- •
Coronary vein, a.k.a. left gastric vein, can become dilated in portal hypertension
- •
PVs including main portal, left portal, and anterior and posterior branches of right PV evaluated with both grayscale and color Doppler in longitudinal plane; spectral Doppler waveform analysis also performed on all vessels in longitudinal plane
Pathology
- •
Increased portal pressures causes portal blood flow to divert into portosystemic collaterals, eventually resulting in increased resistance and reversal of flow in PVs
- •
Intrahepatic etiologies most common cause of portal hypertension
Clinical Issues
- •
Patients often asymptomatic; clinical manifestations can include splenomegaly, abdominal wall collateral vessels, and thrombocytopenia
- •
Pathophysiology unclear, but thought to arise from hepatic inflammation with cellular regeneration, resulting in increased pressure in portal venous system
- •
Treatment of underlying cause of portal hypertension, if possible (i.e., infection)
Scanning Tips
- •
PV diameter on deep inspiration higher than on expiration; thus PV diameter measured during deep inspiration may overestimate true diameter