Chapter Outline
In this chapter, we discuss fluorine-18-deoxyglucose positron emission tomography (FDG PET) and positron emission tomography/computed tomography (PET/CT) of the solid parenchymal organs of the abdomen and highlight in particular the advantages and pitfalls of hepatopancreatobiliary, splenic, and adrenal PET imaging.
Gallbladder and Biliary Tract
The gallbladder and biliary tract are essentially indistinguishable from the liver because of minimal physiologic FDG activity in these structures.
Cholangiocarcinoma
Several studies have shown that FDG PET has a 90% or greater sensitivity for primary cholangiocarcinoma. However, the accuracy of FDG PET for detection of cholangiocarcinoma appears to be dependent on the anatomic location, growth pattern, and pathologic characteristics. Studies have shown that the sensitivity of FDG PET for detection of intrahepatic cholangiocarcinoma is relatively higher than that for perihilar and extrahepatic tumors ( Fig. 68-1 ). For example, Corvera and associates found that the sensitivity of PET for detecting intrahepatic cholangiocarcinoma was 95% compared with only 69% for extrahepatic cholangiocarcinoma. Petrowsky and colleagues and Lee and coworkers also found that the sensitivity for detecting intrahepatic cholangiocarcinoma was higher than that for extrahepatic cholangiocarcinoma (93% vs 55% and 100% vs 78%, respectively). Furthermore, Moon and colleagues found that the site of the primary tumor affected sensitivity of FDG PET; the sensitivity of FDG PET was lower for perihilar tumors compared with intrahepatic and common bile duct cancers (83% vs 91%, 91%). Moreover, in cases of perihilar tumors, the sensitivity of PET was lower than that of CT (83% vs 92%). Yamada and coworkers also concluded that the sensitivity for the detection of hilar cholangiocarcinomas was less than that for the detection of intrahepatic and extrahepatic cholangiocarcinoma (78% vs 100% and 84%, respectively). However, Reinhardt and associates were able to differentiate 12 patients with extrahepatic cholangiocarcinoma from 8 patients without cholangiocarcinoma by PET/CT with a delayed timing of FDG uptake and a maximum standardized uptake value (SUV max ) cutoff of 3.6.
The diagnostic accuracy of FDG PET in cholangiocarcinoma is also related to the growth pattern of the tumor. Anderson and coworkers reported a sensitivity of 85% for nodular morphology but only 18% for infiltrating morphology. Kato and associates similarly found that 11 of 13 tumors (85%) found to be a tumoral mass in the bile duct on CT were identified on PET, whereas only 4 of 11 infiltrating-type tumors (36%) were detected by PET. The diagnostic accuracy of FDG PET may also differ on the basis of the histopathologic findings. Fritscher-Ravens and coworkers found that whereas all true-positive PET results were seen in the tubular type of cholangiocarcinoma with a high amount of tumor cells and only low production of mucus, false-negative PET results were observed in three patients with mucinous adenocarcinoma.
Cholangiocarcinoma is a well-documented malignant complication of primary sclerosing cholangitis (PSC). The average prevalence of cholangiocarcinoma in PSC is approximately 10%. The detection of cholangiocarcinoma in patients with PSC remains challenging, despite improvements in morphologic imaging. Alkhawaldeh and colleagues found that by using the SUV max cutoff of more than 3.9 in patients with PSC and suspected cholangiocarcinoma, FDG PET/CT had a sensitivity, specificity, and accuracy of 94%, 83%, and 91%, respectively. However, an earlier study by Fevery and coworkers found that PET is not reliable in the diagnosis of cholangiocarcinoma in patients with PSC as there were two false-positive and one false-negative results in the 10 patients in their study.
The resectability of cholangiocarcinoma depends on its regional and distant spread. Advances in surgery have increased the likelihood of achieving local disease control. Accurate staging is critical for surgical planning and also to prevent unnecessary surgical intervention in those with advanced disease. Compared with CT, PET has been found to have a higher specificity but lower sensitivity in the diagnosis of regional lymph node metastases. Another study found that FDG PET could detect lymph node metastases undetected by CT and changed the treatment plan in a significant number of cases. With regard to distant metastases, several studies have demonstrated the high accuracy of FDG PET in the detection of unsuspected distant metastasis. This revealing of otherwise undetected distant metastases has also been shown to play a significant role in clinical decision-making.
For the detection of recurrent cholangiocarcinoma, PET/CT may be beneficial in detecting disease recurrence for which anatomic imaging can be limited because of distortion and fibrotic changes after surgery. Jadvar and colleagues assessed the role of PET/CT in detecting recurrence after surgery and found a sensitivity and specificity of 94% and 100% for PET/CT compared with 82% and 43% for CT alone.
PET/CT may have a role in predicting survival in patients with cholangiocarcinoma undergoing treatment. Zhu and associates found that a decrease in SUV max after treatment of advanced biliary tract cancers with combined gemcitabine, oxaliplatin, and bevacizumab was associated with disease control and an increase in progression-free and overall survival. Furthermore, Haug and coworkers found that changes in SUV max , SUV mean , and metabolically active tumor volume at 3 months after yttrium 90 ( 90 Y) radioembolization for intrahepatic cholangiocarcinoma were able to predict patient outcome.
Gallbladder Carcinoma
FDG PET has been found useful in the characterization of gallbladder lesions ( Fig. 68-2 ). Koh and associates, in a study of 16 patients, found that FDG PET had a sensitivity of 68% and a specificity of 88%. In another case series of 16 patients by Rodriguez-Fernandez and coworkers, in which SUV in the gallbladder of more than 2.5 was considered positive for neoplasm, FDG PET was found to have a sensitivity of 80% and a specificity of 82%. In a study by Oe and colleagues, PET had a sensitivity of 75% and a specificity of 100% in distinguishing between malignant and benign gallbladder wall thickening.
Nishiyama and coworkers found that delayed FDG PET was more helpful than early FDG PET for evaluating malignant lesions because of increased lesion uptake and increased lesion-to-background contrast. When a threshold of SUV early of 4.5, SUV delayed of 2.9, and retention index of −8 were chosen as arbitrary cutoffs for differentiating between malignant and benign conditions, sensitivity increased from 83% to 96% and 100% for delayed imaging and combined early and delayed imaging, respectively. However, few centers perform delayed FDG PET scanning, in large part because of workflow logistics.
Lee and coworkers found that in 16 patients with gallbladder cancer, PET/CT detected 14 cases (88%), whereas multidetector CT identified 15 cases (94%). In a study by Corvera and associates, FGD PET/CT identified 100% of the 15 primary gallbladder carcinomas left in situ. In a study by Petrowsky and colleagues, PET/CT detected each primary or recurrent gallbladder cancer (100%), whereas contrast-enhanced CT identified tumor in only 10 of 14 patients (71%).
In patients diagnosed with incidental gallbladder cancer after cholecystectomy for presumed benign disease, PET/CT may be a useful tool for the selection of patients for potentially curative treatment and may help reduce the number of patients undergoing nontherapeutic reexploration.
The presence of distant metastases in biliary tract cancers is associated with poor survival, regardless of treatment. It is therefore important to detect distant metastases so that surgery is offered only to those who may benefit from it. A study by Albazaz and colleagues on the clinical impact of FDG PET/CT in management decisions found that PET/CT had a major impact on management in 39% of cases in patients with gallbladder cancer, including upstaging of 27% of the scans performed for initial staging. Corvera and associates also found that among patients with gallbladder cancer, PET changed management in 23% by showing metastatic disease not seen on other imaging, preventing futile and unnecessary explorations.
FDG PET/CT has a role to play in the detection of recurrent gallbladder carcinoma. Kumar and colleagues found that FDG PET/CT had a sensitivity of 98% and a specificity of 90% in detecting tumor recurrence. They also concluded that when comparable conventional imaging (contrast-enhanced CT, MRI) was available, PET/CT had a better sensitivity for the detection of recurrence.
Interestingly, FDG PET/CT may also have a role in risk stratification of patients with gallbladder polyps. A study by Lee and colleagues found that visual grading, polyp SUV max cutoff of 2.14, and polyp-to-liver ratio cutoff of 1.14 yielded accuracy of 80%, 78%, and 84%, respectively, in diagnosis of malignant gallbladder polyps in the 1- to 2-cm size range.
Pitfalls
FDG PET must be interpreted carefully in patients with PSC and patients with other biliary strictures as biliary stents, known granulomatous disease, or other benign inflammatory conditions may accumulate FDG. In the cases of gallbladder cancer, false-positive FDG PET results have been reported with xanthogranulomatous cholecystitis, tuberculoid granulomatosis of the gallbladder, and adenomyomatosis.
Liver
At the standard image acquisition of approximately 1 hour after FDG administration, hepatic activity is usually mildly intense with a relatively uniformly mottled appearance.
Hepatocellular Carcinoma
Well-differentiated hepatocellular carcinoma (HCC) has a high level of glucose-6-phosphatase, which results in dephosphorylation of FDG-6-phosphate and thus low FDG accumulation compared with poorly differentiated HCC, which has a low level of glucose-6-phosphate and tends to be FDG avid. Because of the variable glucose metabolism of HCC, FDG PET has shown mixed utility in the detection of HCC. Initial studies on PET-only scanners reported a detection rate of primary untreated HCC of 50% to 70%. A more recent study on PET/CT for the detection of primary HCC reported a sensitivity of 61%. The investigators also found that advanced tumor stage, portal vein thrombosis, large tumors, and multiple tumors were significantly associated with positive FDG PET/CT results. With respect to the size of the lesion, the sensitivity was 27%, 48%, and 93% for index lesions measuring 1 to 2 cm, 2 to 5 cm, and more than 5 cm, respectively.
Even though the sensitivity of FDG PET has been found to be lower than that of other imaging modalities, it still plays an important role in management and prognosis. The detection of extrahepatic metastases, although rare, can significantly affect management. Kawaoka and associates compared the efficacy of PET/CT with CT for the detection of extrahepatic metastases (lung, lymph node, and bone) and found that CT was more sensitive than PET/CT for the detection of lung metastases and performed equally well for nodal metastases; however, bone metastases were more accurately detected by PET/CT. The three PET false-negative lung metastases in the study were less than 8 mm. Sugiyama and coworkers found a similar pattern, in which the detection rate of FDG PET was 83% for extrahepatic metastases larger than 1 cm but only 13% for lesions of 1 cm or less.
Shiomi and coworkers found that the SUV ratio (SUV ratio of tumor to nontumor in the liver) correlated with tumor volume doubling time and that the cumulative survival rate could be predicted on the basis of the SUV ratio. Kawamura and associates also found that the SUV ratio was associated with survival, with people with SUV ratio of more than 1.6 having a lower survival rate. Another study found that patients with tumor SUV of more than 7 had a significantly lower median survival time (4 vs 15 months). Hatano and colleagues evaluated the role of preoperative PET in predicting the prognosis of patients after resection. In patients with SUV ratio of more than 2, the overall survival was significantly shorter than in those with a lower SUV ratio (182 vs 2310 days). Seo and coworkers had similar results, concluding that the overall survival and disease-free survival were significantly lower in the high SUV ratio group (>2) compared with the low SUV ratio group.
HCC is one of the major indications for liver transplantation; however, appropriate patient selection can be difficult. A study of 43 patients with HCC who underwent PET before liver transplantation found that patients with advanced PET-negative tumors and patients with HCC meeting the Milan criteria had a comparable 3-year survival rate (80% vs 94%). The HCC recurrence rate in this study was 50% in the PET-positive group compared with 3.8% in the PET-negative group. Another study by Lee and colleagues attempted to evaluate FDG PET as a prognostic factor in predicting HCC recurrence after liver transplantation. They found that the ratio of tumor SUV max to normal liver SUV max was the most significant parameter for the prediction of tumor recurrence, with a cutoff value of 1.15. Among the tumor recurrence patients, 93% had a value of 1.15 or more, whereas just 18% of the nonrecurrence patients had a value of 1.15 or more. The 1- and 2-year recurrence-free survival rates were significantly different between the two groups.
Patients with HCCs that are nonresectable or those awaiting transplantation can be treated with ablation or embolization. PET has been shown to play a role in monitoring response to such treatments. Torizuka and coworkers found that after transarterial chemoembolization, increased or similar FDG uptake relative to normal liver was suggestive of residual viable tumor, whereas decreased or absent FDG uptake indicated more than 90% necrosis. Paudyal and coworkers found that after radiofrequency ablation, PET detected recurrence earlier than CT and had a higher overall detection rate (92% for PET vs 75% for CT). Han and colleagues found that PET/CT was valuable in patients who had unexplained serum α-fetoprotein elevation after either transarterial chemoembolization or radiofrequency ablation and a normal multiphasic CT scan.
For patients with advanced-stage HCC or with disease progression after locoregional therapy, treatment options are limited. However, studies have recently demonstrated survival benefit with sorafenib for patients with advanced HCC. PET/CT may have a role in monitoring of patients treated with sorafenib and for predicting response to treatment. A report of two patients with positive FDG PET at baseline found that a PET scan early after the start of treatment seemed to be a promising technique for monitoring early response. A more recent study by Lee and colleagues concluded that the degree of FDG uptake on baseline PET scan significantly correlated with overall survival and progression-free survival for such patients receiving sorafenib treatment.
Metastases
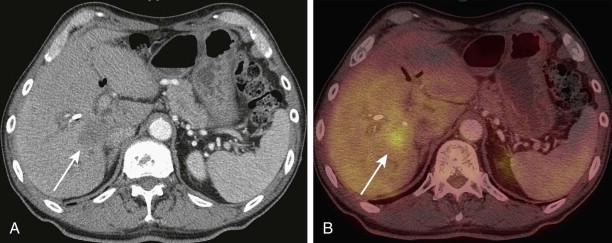
Metastatic disease accounts for the majority of malignant hepatic lesions. The presence of liver metastases often guides the management of patients and is one of the main determinants of survival. FDG PET has been shown to be highly sensitive in detecting liver metastases ( Fig. 68-3 ). Delbeke and coworkers found that FDG PET detected all liver metastases larger than 1 cm from a number of different primary tumors. A meta-analysis by Kinkel and associates found that at equivalent specificity, FDG PET was the most sensitive noninvasive imaging modality for the diagnosis of hepatic metastases from cancers of the gastrointestinal tract. Another meta-analysis by Bipat and colleagues concluded that FDG PET had significantly higher sensitivity on a per-patient basis compared with CT and MRI, but not on a per-lesion basis, in patients with colorectal liver metastases.

Hepatic resection is the most effective therapy for a subset of patients with liver metastases; however, strict selection criteria are paramount as there is no survival benefit if residual disease remains after hepatectomy. Arulampalam and colleagues found that preoperative FDG PET in patients with colorectal liver metastases altered management in 39% of patients, with avoidance of unnecessary surgery being the most common change. A study by Fernandez and colleagues found that use of FDG PET to assess patients with colorectal liver metastases being considered for partial hepatectomy was associated with excellent postresection 5-year survival.
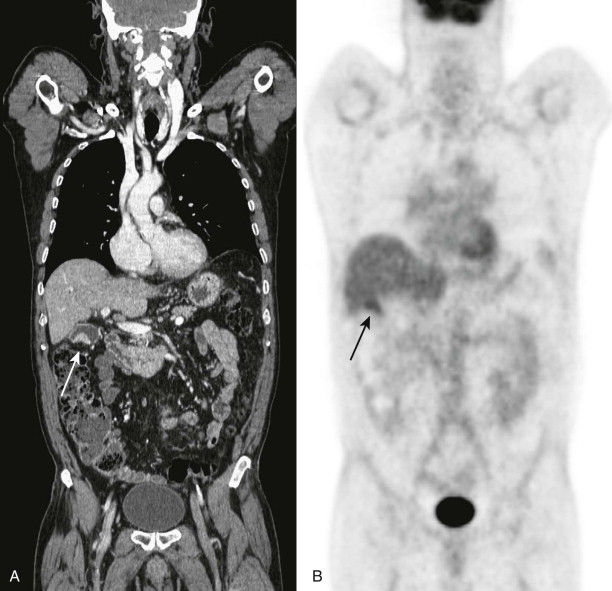
Complete surgical resection is the best chance of cure in patients with liver metastases. However, in some patients, this is not feasible because of location of the tumor, multifocality, or insufficient functional liver reserve. In these cases, local ablative techniques may have a role to play. PET may have a role in follow-up of patients who underwent ablation ( Fig. 68-4 ). Donckier and coworkers compared PET and CT in 28 metastatic tumors 1 week, 1 month, and 3 months after radiofrequency ablation. The PET scan performed at 1 week found residual disease in 4 cases that was not identified on any of the CT scans at 1 week, 1 month, and 3 months.

Radioembolization with 90 Y microspheres has emerged as a palliative treatment for hepatic metastases of various tumors. Szyszko and colleagues performed a study evaluating the role of PET compared with Response Evaluation Criteria in Solid Tumors (RECIST) in early response assessment after 90 Y radioembolization in 21 patients. They found that 86% of patients demonstrated decreased PET activity at 6 weeks, whereas only 13% showed a partial response in the size of tumor on CT scan. A study by Haug and coworkers in 58 patients with breast cancer metastases treated with 90 Y radioembolization found that PET/CT performed 3 months after treatment was the strongest predictor of survival (67 weeks in responders vs 43 weeks in nonresponders). Furthermore, they found that a pretreatment SUV max of more than 20 was associated with a significantly shorter median survival than was SUV max of 20 or less (21 vs 52 weeks). Another study comparing FDG PET/CT with RECIST and tumor density criteria found that PET/CT significantly predicted progression-free survival (the median progression-free survival in patients with a partial response was 12 months compared with 5 months in those with stable disease), whereas RECIST and tumor density criteria did not.
During the last few years, the addition of biologic agents (anti–epidermal growth factor receptor antibodies and anti–vascular endothelial growth factor antibodies) to conventional chemotherapy has increased overall survival in patients with metastatic colorectal cancer; it also has improved response rates and can render unresectable liver metastases resectable. A report by Bertolini and coworkers found that patients with nonoptimally resectable colorectal metastases treated with FOLFOX (folinic acid, fluorouracil, oxaliplatin) and bevacizumab who achieved at least 1 unit reduction in SUV max had longer progression-free survival (median progression-free survival of 22 vs 14 months). Another study found that low follow-up SUV max and complete metabolic response were favorable prognostic factors in patients with metastatic colorectal cancer who underwent liver surgery with curative intent after neoadjuvant chemotherapy with bevacizumab.
Lymphoma
Primary hepatic lymphoma is defined as a lesion or lesions confined to the liver only without the involvement of any other organ or lymph nodes; it is extremely rare, representing less than 1% of all extranodal lymphomas. It usually is manifested as a solitary mass ( Fig. 68-5 ) or as multiple discrete masses. Rarely, the disease is manifested as diffuse involvement of the liver. Case reports have found the lesions to be hypermetabolic on PET/CT.

Pitfalls
Causes of false-negative FDG PET findings include small size of lesion, underestimation of uptake, misregistration of foci, and recent completion of chemotherapy. Underestimation of FDG uptake and misregistration of foci are caused by the physiologic motion of the liver during emission scans. False-positive findings for malignant changes on PET have also been reported. Causes include intrahepatic abscess and benign inflammatory lesions, such as regenerative nodules in a cirrhotic liver.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








