SONOGRAM ABBREVIATIONS
E, EP Epididymis
H Hydrocele
M Mass
MT Mediastinum testis
S Spermatocele
T Testis
V Varicocele
KEY WORDS
Appendix Epididymis. Embryologic remnant projecting off of the epididymis.
Appendix Testis. Embryologic remnant of the Müllerian duct. Small ovoid structure seen just beneath the head of the epididymis. Both the appendix testis and the appendix epididymis are best seen in the presence of a hydrocele.
Cryptorchidism (Undescended Testicle). Condition in which the testes have not descended and lie either in the abdomen or in the groin. The latter is the site in 95% of cases. The cryptorchid testicle and, to a lesser extent, the normally descended opposite testicle have an increased risk of malignancy.
Epididymis. “C”-shaped organ that lies posterolateral to the testicle in which the spermatozoa accumulate before passing out the vas deferens. It has three parts, the head (globus major), body (corpus), and tail (globus minor).
Epididymitis. Inflammation of the epididymis. Often associated with orchitis, inflammation of the testicle.
Hematocele. Blood filling the sac that surrounds the testicle.
Hydrocele. Distention of the sac that encloses the testicle with straw-colored fluid.
Mediastinum Testis. Linear fibrous structure in the center of the testicle.
Pampiniform Plexus. Group of veins that drain the testicle. They dilate and become tortuous when a varicocele is present.
Rete Testis. The tubules at the hilum of the testicle may become so large that they are visible as cylinders or cysts. This is a normal variant finding.
Scrotum. Sac in which the testes and epididymides lie.
Seminal Vesicles. Paired comma-shaped organs located posterior to the bladder that add fluid necessary for reproduction to the sperm arriving from the vas deferens.
Serous. Term used to describe thin, straw-colored fluid present within a cyst regardless of location (e.g., renal, thyroid, or ovarian cysts or hydrocele).
Spermatic Cyst (Spermatocele). Cyst along the course of the vas deferens containing sperm.
Testicle (Testis). Male gonad enclosed within the scrotum; it produces hormones that induce masculine features and spermatozoa.
Tunica Albuginea. White membrane surrounding the testicle within the scrotum; may be the source of a cyst or adenoma.
Tunica Vaginalis. Membrane skirting the inner wall of the scrotum. It has two parts: the inner or tunica vaginalis, and the outer or tunica albuginea. Hydroceles form between the two layers of the tunica vaginalis.
Varicocele. Dilated veins caused by obstruction of the venous return from the testicle. Varicoceles may be associated with infertility or tumors in the renal hilar regions.
Vas Deferens. Tube that connects the epididymis to the ejaculatory duct.
The Clinical Problem
MASS
The testicle is superficial and therefore easily examined with high-frequency ultrasound. The detection of a small mass within the testicle is important because such a mass may be malignant. Most intratesticular masses should be considered to represent cancer until proven otherwise; however, benign masses in the testicle occur. Although fluid within the scrotal sac is usually easily detected clinically, identification is difficult if the scrotal wall is thickened. An additional mass may be missed on palpation but revealed by ultrasound.
TESTICULAR PAIN
Ultrasound helps in the differential diagnosis of acute pain in a testicle. One can reliably differentiate between the two most common causes: epididymo-orchitis and associated complications (abscess), and testicular torsion. Doppler and color flow are particularly useful in making this distinction. Acute epididymitis is often followed by infection of the testicle (orchitis). Infarction of the testicle can also occur after severe epididymitis.
TESTICULAR TRAUMA
Trauma to the testicle is an ultrasonic emergency—rupture of the testicle requiring surgical repair has to be distinguished from a paratesticular hematoma (a hematocele). An unrepaired ruptured testicle atrophies and will not function.
INFERTILITY
A common cause of male infertility is a varicocele. Most varicoceles are palpable, but if a man has unexplained infertility, a sonogram to exclude a varicocele that cannot be felt is worthwhile.
UNDESCENDED TESTICLE
Most testicles descend from the abdomen into the scrotum by 28 weeks of fetal life. If descent is arrested in the abdomen or the groin, there is an increased chance of tumor development. Surgeons move the undescended testicle into the scrotum in the first few years of life. Ultrasound can be of help in locating a testicle that cannot be felt within the groin, although those that lie deep in the abdomen cannot be detected with ultrasound; magnetic resonance imaging or computed tomography may be necessary in those cases.
Anatomy
TESTICLE
The testicle is an ovoid, homogeneous, mildly echogenic structure (Fig. 25-1). The adult testicles are normally symmetric and approximately 3 to 5 cm in length, 2 to 4 cm in width, and 3 cm in anteroposterior dimension. A central line within each testicle is termed the “mediastinum testis.”
A series of tubules radiate from the mediastinum testes into the testicle. Sometimes a vague hypoechoic region is seen. On other occasions, visible tubules or even cysts can form in this area as a benign normal variant, known as “rete testis” or tubular ectasia.
EPIDIDYMIS
The tubular, slightly sonolucent structure lying posterosuperior to the testicle at the proximal end is termed the “head of the epididymis.” The body of the epididymis varies in its position and generally lies posterolateral to the testicle. The testicular artery and the veins of the pampiniform plexus run along the lateral and posterior aspect of the testicle in the region of the epididymis and are not normally visible. The epididymis is an echopenic structure.
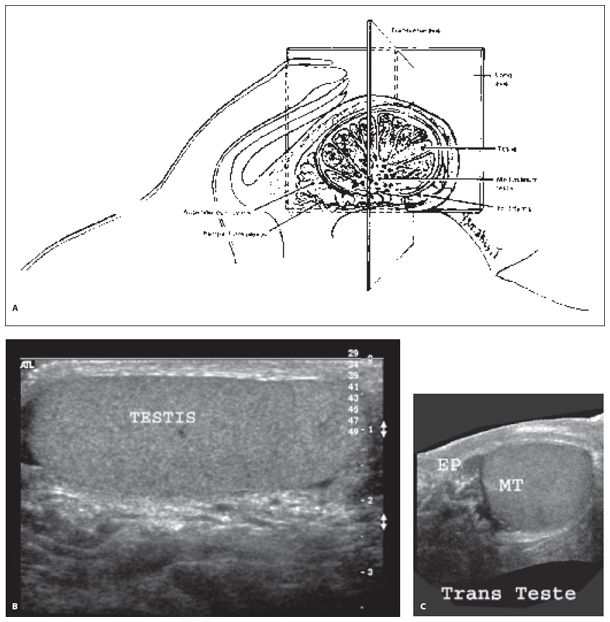
Figure 25-1. ![]() Diagram showing the normal structures visible within the scrotum. The mediastinum testis is only occasionally seen as an echogenic line. A. Diagram of imaging planes. B. Longitudinal axis view. C. Transverse axis view.
Diagram showing the normal structures visible within the scrotum. The mediastinum testis is only occasionally seen as an echogenic line. A. Diagram of imaging planes. B. Longitudinal axis view. C. Transverse axis view.
The scrotal wall is an echopenic structure that surrounds the testicle and epididymis. The wall thickens with edema and infection. The two layers of the tunica vaginalis form a double layer around the testicle. Fluid can accumulate between these two layers forming a hydrocele. A small amount of serous fluid here is a common normal variant of no significance, but pus accumulating here (“pyocele”) is a serious problem.
Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


