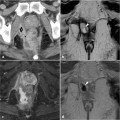
Fig. 22.1
A 56-year-old male patient with Crohn’s disease. After surgical fistulectomy in the previous site of a simple transsphincteric fistula, the anal canal shows subtle right-sided hypointense irregularity (arrowhead) on the axial T2-weighted image (a) without hyperintense signal on the axial STIR image (b) nor abnormal enhancement on the corresponding post-contrast axial fat-suppressed (c) and coronal (d) T1-weighted images
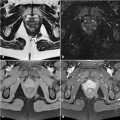
At MRI, setons appear as thin tubular structures with low signal intensity on all sequences; they are best identified within a fluid-containing T2-hyperintense fistulous tract or abscess collection (Fig. 22.2). An alternative surgical option is the positioning of a draining large-caliber Foley catheter [3].
Owing to its precise reproducibility, with high contrast and spatial resolution (Figs. 22.3, 22.4), MRI is the imaging modality of choice to document postoperative appearances, even after more complex surgical procedures, including extensive resection, omentoplasty, and fasciocutaneous flaps, and to investigate suspected complications such as leakages and abscess collections [1,2].


Fig. 22.2
A 32-year-old male patient with Crohn’s disease. Initial MRI including axial T2-weighted (a) and contrast-enhanced coronal T1-weighted (b) images shows a large abscess collection occupying the left levator ani muscle. After treatment via a surgical approach, follow-up MRI consisting of axial (c) and coronal (d) T2-weighted images shows abscess reduction with the seton (arrowheads) in place
22.2 MRI Follow-Up During and After Infliximab Therapy
Treatment with the anti-tumor necrosis factor (anti-TNF) antibody infliximab has been shown to effectively achieve rapid closure of anal fistulas, although its mechanism of action is still poorly understood. Fistula healing is undoubtedly a refractory and slow process although its rate, extent, and duration are under investigation. After induction therapy, the clinical response is often short and maintenance therapy at scheduled intervals is usually required [4–8].
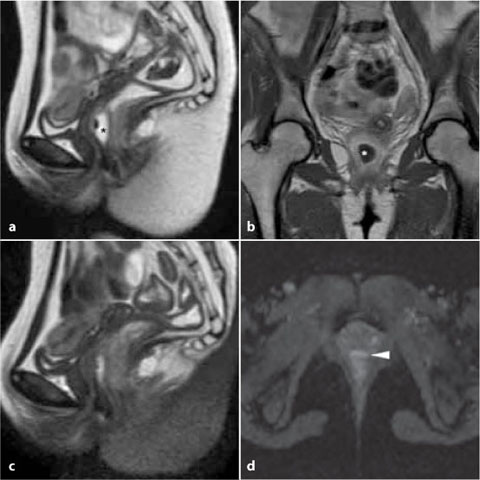
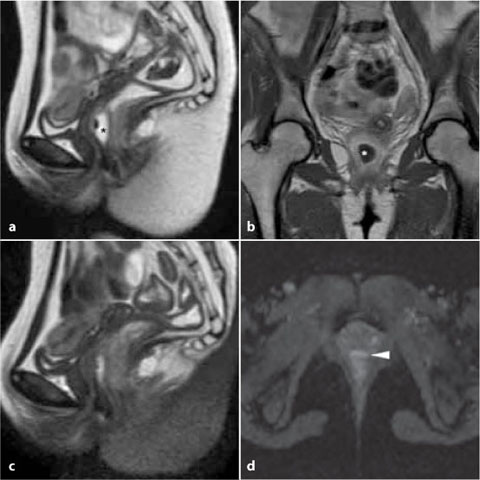
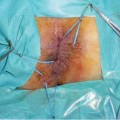
Fig. 22.3
A 27-year-old female patient with Crohn’s disease. Initial MRI including sagittal T2- weighted (a) and post-contrast coronal T1-weighted (b) images detects a large abscess occupying the anovaginal septum (*). After surgical drainage, repeated MRI (c, d) shows significant reduction, evidenced by the collapsed abscess walls (arrowheads)
Preliminary studies have suggested that the cessation of drainage from external orifices does not accurately reflect the true condition of the fistulous tract, since fistulas may persist despite healing of the external openings, leading to abscess formation that may become clinically evident after treatment [3,6,9,10]. The ability of MRI to detect residual active inflammation even with closed orifices makes it particularly suited for the non-invasive assessment of the results of infliximab therapy [10].
The recent ECCO (European Crohn’s and Colitis Organization) guidelines recognized the need for pre-treatment imaging and thus recommended MRI or endoanal ultrasound for all fistulas under consideration for medical and/or surgical treatment [11].
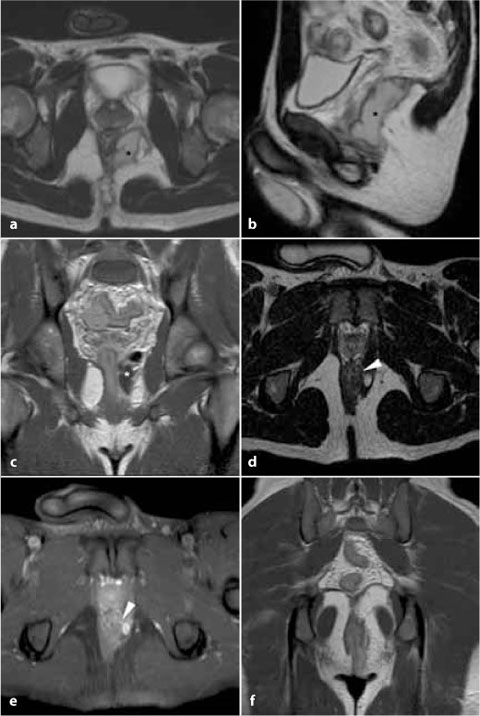
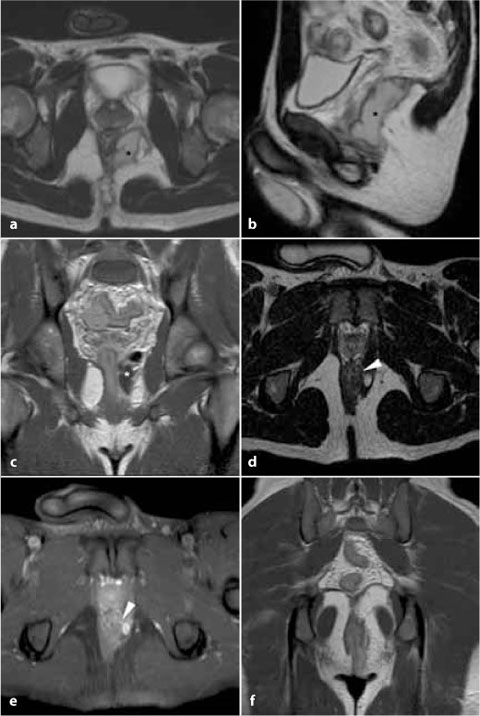
Fig. 22.4
A 25-year-old male patient with Crohn’s disease. Initial MRI (a-c) showed a large abscess with mixed air and fluid content, extensively involving the left ischioanal fossa and leva- tor ani muscle (*). Complementary transperineal ultrasound revealed the presence of a posterior extrasphinteric fistula. Following seton placement and medical therapy with azathioprine plus infliximab, MRI at one-year follow-up (d-f) evidenced a significant reduction of the abscess and a normalization of the levator ani muscle (f). The left-sided transsphinteric fistula became visible (arrowheads in d and e) in association with a very small residual ischioanal abscess
In 2003, Van Assche et al. published a MRI-based severity score for perianal Crohn’s disease that takes into account the anatomical extension of the fistulous tracts along with their T2-hyperintensity in areas of inflammation, the presence of abscess collections, and rectal wall involvement (Table 22.1). Although this scoring system has been validated in the pretherapeutic setting, is easily reproducible, and useful in clinical trials, it notably lacks key information obtainable from MRI, since it does not consider inflammatory activity that is well detected by contrast enhancement [10].
Baseline MRI examinations evaluated prior to infliximab therapy should be carefully analyzed for evidence of clinically occult purulent collections, since their presence may predispose the patient to abscess development during biologic therapy. Anti-TNF drugs are contraindicated in the presence of an abscess [12]; instead, these patients should be referred for drainage or other surgical treatment before infliximab is started [6,10].
Complex inflammatory disease at baseline is reportedly associated with a worse outcome after medical therapy. Conversely, other investigators have not identified the initial MRI features that reliably predict fistula healing and clinical remission after infliximab treatment [13,14].
Parameter | Score |
|---|---|
Number of fistula tracts | |
None | 0 |
Single, unbranched | 1 |