Posterior Tibialis Tendinitis and Other Abnormalities of the Posterior Tibialis Tendon
Anatomic Considerations
The posterior tibialis muscle plantarflexes the foot at the ankle and inverts the foot at the subtalar and transverse tarsal joints. The muscle finds its origin from the posterior tibia and fibula (Fig. 7.1). The tendon of the muscle passes behind the medial malleolus, running beneath the flexor retinaculum, and into the sole of the foot where it inserts on the navicular bone (Fig. 7.2). The posterior tibialis tendon is susceptible to the development of tendinitis as it curves around the medial malleolus (Fig. 7.3).
Clinical Correlates
Posterior tibialis tendinitis is a clinical syndrome characterized by sharp, constant, and severe inner ankle pain. This painful condition is often seen as a result of acute eversion injuries to the ankle although it is also seen with overuse or misuse of the ankle in foot, as seen in long distance running with improper shoes. Recently, there have been a number of reports of posterior tibialis tendinitis in Irish dancers as a result of the “leap over move” that is a common part of their dance routine.
Patients suffering from posterior tibialis tendinitis often splint the inflamed posterior tibialis tendon by adopting an antalgic gait to avoid using the affected tendon. This dysfunctional gait may cause a secondary bursitis and tendinitis around the foot and ankle, which may both confuse the clinical picture and further increase the patient’s pain and disability. Pain on palpation of the posterior tibialis tendon as it passes behind the medial malleolus is a consistent finding in patients with posterior tibialis tendinitis as is exacerbation of pain with active resisted inversion and passive eversion of the ankle (Fig. 7.4). The inner aspect of the ankle may feel hot and appear swollen, which may be misdiagnosed as superficial thrombophlebitis or cellulitis. Patients suffering from posterior tibialis tendinitis will also often complain that it feels like their shoes are rubbing the inside of their ankles raw, although on examination the skin appears normal. A creaking or grating sensation may be palpated when passively inverting and everting the ankle. Untreated, posterior tibialis tendinitis will result in increasing pain and functional disability calcium deposition around the tendon occurring, making subsequent treatment more difficult. Continued trauma to the inflamed tendon ultimately may result in tendon rupture (Fig. 7.5). Rupture of the posterior tibialis tendon will result if disruption of the normal architecture of the foot resulting in the loss of the arch of the foot and development of the pes planus deformity (Fig. 7.6).
Plain radiographs are indicated in all patients who present with medial ankle pain. Based on the patient’s clinical presentation, additional testing may be indicated, including complete blood cell count, sedimentation rate, and antinuclear antibody testing. MRI or ultrasound imaging of the ankle is indicated if posterior tibialis tendinitis, rupture, or joint instability is suggested (Figs. 7.7 to 7.11). Radionuclide bone scanning is useful to identify stress fractures of the tibia not seen on plain radiographs.
Ultrasound Technique
Ultrasound-guided evaluation of the posterior tibialis tendinitis is carried out by placing the patient in the supine position with the arms resting comfortably along the patient’s chest and the affected lower extremity externally rotated. A total of 4 mL of local anesthetic and 80 mg of depot steroid are drawn up in a 12-mL sterile syringe. The medial malleolus is then identified by palpation. A linear high-frequency ultrasound transducer is placed in a longitudinal plane, with the middle of the ultrasound transducer lying over the posterior border of the medial malleolus (Fig. 7.12). This will put the ultrasound transducer parallel to the posterior tibialis tendon as it passes behind the medial malleolus. An ultrasound survey scan is taken. The posterior tibialis tendon can be seen lying just behind the medial malleolus as a fibular linear structure (Figs. 7.13 and 7.14). When the posterior tibialis tendon is identified on ultrasound imaging, the tendon is evaluated for fluid, extrinsic compression, tendinosis, tendinitis, tears, and rupture (Figs. 7.15 to 7.31). Ultrasound imaging is also useful in assessing the effect of implantable hardware on surrounding structures.
Clinical Pearls
Bursitis and arthritis of the ankle and foot may coexist with posterior tibialis tendinitis and may contribute to the patient’s pain symptoms. It is important to timely diagnose posterior tibialis tendonitis and to identify the activity and/or pathology responsible for its evolution and then initiate prompt treatment to avoid tendon rupture.
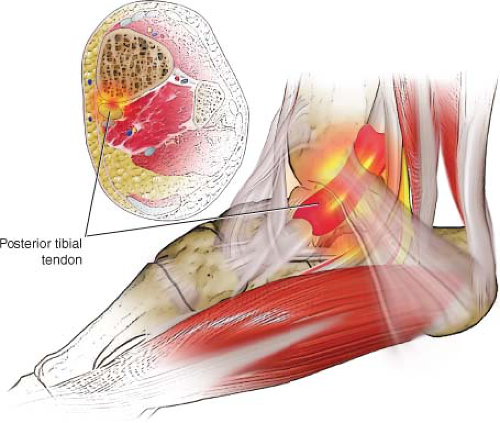 FIGURE 7.3 The posterior tibialis tendon is susceptible to the development of tendinitis as it passes behind the medial malleolus. |
 FIGURE 7.4 Pain on palpation of the posterior tibialis tendon as it passes behind the medial malleolus is a consistent finding in patients with posterior tibialis tendinitis. |
 FIGURE 7.5 Failure to aggressively treat posterior tibialis tendinitis may result in rupture of the tendon. |
 FIGURE 7.6 Rupture of the posterior tibialis tendon will result if disruption of the normal architecture of the foot resulting in the loss of the arch of the foot and development of the pes planus deformity.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|