, Joon Woo Lee1 and Jong Won Kwon2
(1)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Kyonggi-do, Republic of Korea
(2)
Department of Radiology, Samsung Medical Center, Seoul, Republic of Korea
Abstract
Commonly encountered postoperative issues include differentiating (1) normal immediate post-diskectomy changes from residual disk herniation, (2) normal postsurgical changes from infection in the early postoperative period, (3) epidural scar from recurrent disk herniation at any period, and (4) determining fusion or pseudoarthrosis in the late postoperative period. In this chapter, we will describe imaging findings useful in the evaluation of the postoperative spine, focusing on the abovementioned issues.
Commonly encountered postoperative issues include differentiating (1) normal immediate post-diskectomy changes from residual disk herniation, (2) normal postsurgical changes from infection in the early postoperative period, (3) epidural scar from recurrent disk herniation at any period, and (4) determining fusion or pseudoarthrosis in the late postoperative period. In this chapter, we will describe imaging findings useful in the evaluation of the postoperative spine, focusing on the abovementioned issues.
7.1 Normal Post-diskectomy Changes Versus Residual Disk Herniation
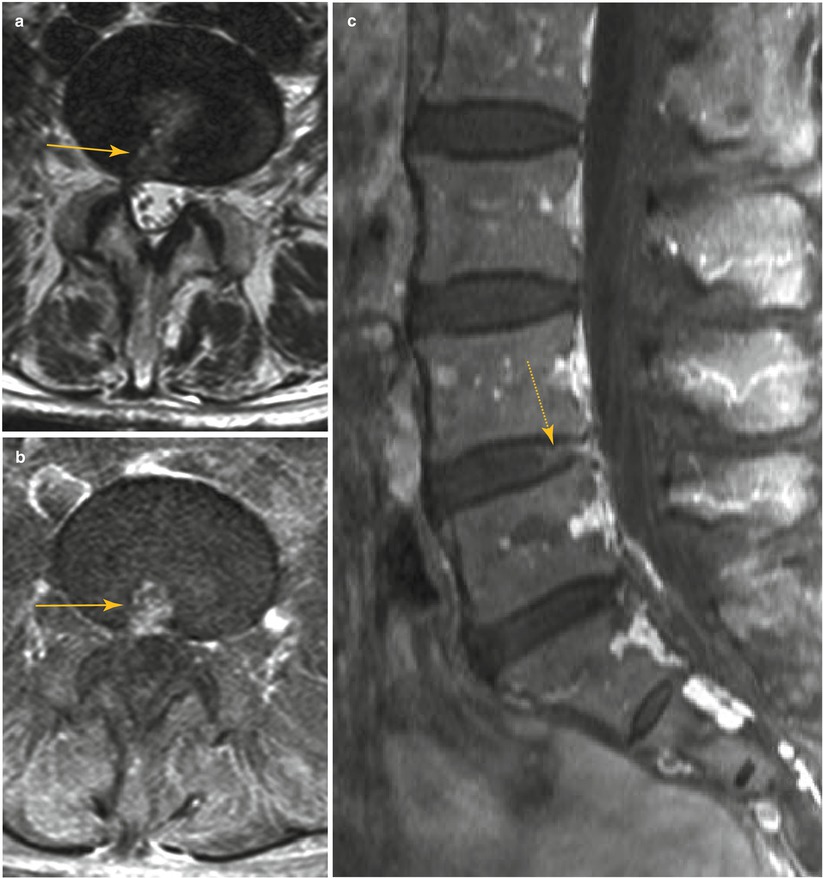
Immediate post-diskectomy changes can mimic residual disk herniation due to residual mass effect upon the epidural space and may be similar in extent to the preoperative state. This is attributed to edema and granulation tissue at the diskectomy site. However, unlike residual disk herniation, the post-diskectomy area usually shows high signal intensity on T2-weighted images as well as homogeneous postcontrast enhancement due to the granulation tissue (Salgado et al. 2006). Thus imaging characteristics suggestive of normal post-diskectomy changes over residual disk herniation include T2 signal change following operation (from low to high signal) and homogeneous enhancement. Mere bulging of the posterior margin of the disk similar in appearance to the preoperative appearance is not in itself a conclusive indicator of residual disk herniation.
7.2 Normal Postoperative Change Versus Early Postoperative Infection
Enhancement of the lumbosacral vertebral endplates and posterior annulus fibrosis has been reported in normal asymptomatic patients in the early postoperative period (Jinkins et al. 1993). This is due to an aseptic reaction, although this can mimic early postoperative infection. Thus in the postoperative period, bone marrow edema and intervertebral disk enhancement are not reliable findings in differentiating between infection from normal postoperative changes. In our experience, the presence of enhancement or increased T2-weighted signal in the psoas muscles remote from the surgical approach (such as performed during a posterior interbody fusion) could be an indication of early postoperative infection. As such, careful review of the paravertebral structures including the psoas muscles on T2-weighted axial images and contrast-enhanced T1-weighted axial images is required to detect any abnormal signal change which may suggest early infection.
It can be difficult to distinguish postoperative fluid collections from abscesses in the surgical site on the basis of imaging findings alone. Image-guided aspiration is often required in cases of clinical uncertainty.
7.3 Postoperative Scarring Versus Recurrent Disk Herniation
While it can sometimes be difficult to differentiate postoperative scar formation from recurrent disk herniation following diskectomy, there are some imaging features that may be helpful in this regard. Postoperative scarring causes retraction of adjacent structures such as the thecal sac and nerve roots, while recurrent disk herniation displaces or compresses upon the adjacent structures. Postoperative scarring also shows homogeneous enhancement, while recurrent disk herniation reveals peripheral enhancement or no enhancement (Bundschuh et al. 1988). The margins of postoperative scarring are ill defined; however the margins of recurrent disk herniation are usually well defined. Postoperative scarring shows discontinuity from the parent disk, while recurrent disk herniation maintains continuity with the parent disk. Postoperative epidural scarring frequently demonstrates intermediate signal intensity on both T1-weighted and T2-weighted images for up to 2 years following operation, beyond which the scar often shows low signal intensity on T1-weighted and T2-weighted images (Sotiropoulos et al. 1989).
Table 7.1
Postoperative scar versus recurrent disk herniation
Postoperative scar | Recurrent disk herniation |
|---|---|
Retraction of adjacent structures | Displaces or compresses adjacent structures |
Homogeneous enhancement | Peripheral or no enhancement |
Ill-defined margins | Well-defined margins |
Discontinuity from the parent disk | Continuity with the parent disk |
7.4 Postoperative Pseudomeningocele Versus Postoperative Fluid Collection
Postoperative pseudomeningoceles occur when cerebrospinal fluid leaks into the operative site resulting in the formation of large cystic masses. These are not true meningoceles as these are lined by reactive fibrous tissues without a true arachnoid layer. Pseudomeningoceles typically develop after inadvertent surgical laceration of the dural sac or following intradural surgery. These should be differentiated from postoperative fluid collections in the surgical site. A postoperative pseudomeningocele manifests as a large cystic lesion communicating from the epidural space to the back muscles and sometimes to the subcutaneous tissues, whereas a postoperative fluid collection is usually smaller, with single or multiple small fluid locules along the operative site most often in the fascial or subcutaneous layers, without identifiable communication between the locules.
7.5 Fusion Versus Pseudoarthrosis
In the late postoperative period, the main concern of the surgeon is the assessment of the degree of fusion and the identification of fusion failure (pseudoarthrosis). One of the signs of interbody fusion is the absence of segmental motion on flexion and extension lateral radiographs. Six criteria indicative of solid fusion based on plain radiographic findings have been defined by Ray and are as follows (Ray 1997): (1) no motion or less than 3° of intersegment position change on lateral flexion and extension views; (2) lack of a lucent area around the implant; (3) minimal loss of disk height; (4) no fracture of the device, graft, or vertebra; (5) no sclerotic changes in the graft or adjacent vertebra; and (6) visible bone formation in the cage or about the cage. CT images with coronal and sagittal reconstructions are an ideal way to determine fusion of the intervertebral disk space. Fusion can be confirmed if there is solid bone bridging the adjacent vertebral bodies. Lucency seen around cages, screws, or any other implants on late postoperative CT imaging (more than 1 year) is suggestive of loosening, this representing osteolysis secondary to device or screw motion. Cystic changes seen on axial images adjacent to the implants are also useful markers of failed fusion. Linear defects in the intradiskal new bone are also indicators of fusion failure. Changes in fusion device position and device subsidence are signs of failed fusion as well, with subsidence being defined as sinkage of the fusion device into the adjacent vertebral bodies (Williams et al. 2005).
Table 7.2
CT features of failed fusion (pseudoarthrosis)
Lucency at the fusion device or pedicle screw margin |
Cystic change within the endplates adjacent to the implant |
Linear defect through intradiskal new bone |
Change in fusion device position |
Device subsidence |
MRI can be used to evaluate for secondary changes due to segmental motion after operation, which can result in Modic type I changes in the adjacent vertebral bodies. Conversely, solid fusion sometimes leads to conversion of preexisting Modic type I changes into fatty Modic type II changes. Persistent or new Modic type I changes occurring 6 months after surgery can be a sign of pseudoarthrosis (Salgado et al. 2006).
7.6 Adjacent Segment Degeneration
New or accelerated disk degeneration adjacent to a fused level (known as “adjacent segment degeneration”) is a problem that occurs in the late period after interbody fusion. One possible mechanism involves load shifting to adjacent levels following elimination of motion after the fusion. Adjacent segment degeneration manifests as loss of disk height, alignment disorders such as anterolisthesis or retrolisthesis, as well as disk bulging, ultimately resulting in central canal stenosis at the level adjacent to the interbody fusion. Artificial disk replacements have been introduced to reduce the incidence of adjacent segment degeneration; however, postoperative results of artificial disk replacements remain controversial.
Table 7.3
Postoperative issues
Early issues | Residual disk herniation versus normal diskectomy changes |
Infection versus normal postoperative findings | |
Pseudomeningocele versus postoperative fluid collection | |
Presence/absence of nerve root injury | |
Presence/absence of hematoma | |
Late issues | Recurrent disk herniation versus scar |
Fusion versus pseudoarthrosis | |
Adjacent segment degeneration |
Forget Me Nots!
Normal post-diskectomy changes show T2 hyperintensity and homogeneous enhancement.
Enhancement of endplates and posterior annulus fibrosis can be seen in normal asymptomatic patients following operation.
CT features of failed fusion include lucency at the fusion device or pedicle screw margin, cystic change within the endplates adjacent to the implant, linear defect (fracture) through intradiskal new bone within or adjacent to the fusion device, change in fusion device position, and device subsidence.
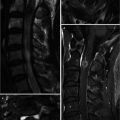
7.7 Illustrations: Post-operative Imaging
7.7.1 Normal Postoperative Changes