Failed agent
Salvage agent
Salvage regimen
Outcome
Reference
Sildenafil
MUSE
Sildenafil 100 mg 1 h prior to intercourse; 500 mcg MUSE immediately before intercourse
83 % patients reported improvements in EF (mean IIEF-5: 18.6 in salvage vs. 13.2 in sildenafil) and penile rigidity
[72]
VED
Sildenafil
Sildenafil 100 mg 1–2 h prior to VED use for intercourse
77 % patients reported improvements in penile rigidity and sexual satisfaction
[73]
Sildenafil or Vardenafil
ICI (alprostadil)
Alprostadil 15 or 20 mcg; timing of treatments not specified
68 % patients reported improvements in EF (mean SHIM: 23.4 salvage vs. 14.3 sildenafil alone; 24.1 vs. 14.9 vardenafil alone)
[74]
Penile Prostheses
Penile prostheses are typically employed as a definitive treatment for ED, including post-prostatectomy ED, should other treatments prove ineffective or unacceptable. In fact, since the introduction of PDE5 inhibitors, it has been demonstrated that the etiology of ED for men undergoing penile prosthesis implantation has changed, with vascular disease being the predominant etiology before sildenafil, and radical pelvic surgery (including radical prostatectomy) predominating since [75]. Although multiple types of penile prostheses are available, including semirigid (non-inflatable) and two-piece inflatable prostheses, the gold standard prostheses are the three-piece inflatable models, currently the most commonly used penile prostheses [76, 77].
When counseling men and their partners about penile prostheses, reasonable expectations must be outlined. These are mechanisms by which to achieve rigid erections for intercourse; sensation, orgasm and actual penile length should not be affected, for better or worse. They must understand that once a penile prosthesis is in place, they cannot simply revert to another ED therapy should they not like it. Opportunities for independent review of information on the prostheses and for discussion with patients who have already undergone the procedure to ascertain their personal experiences should be provided.
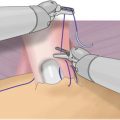
The benefits of the prostheses are the assurance that a rigid erection will be achieved for penetrative intercourse, as well as the relative spontaneity with which an erection can be generated. The drawbacks include their irreversible nature and the need for surgery with all of the attendant risks. Specific risks for penile prostheses include device infection, erosion and malfunction requiring surgical revision or replacement. Especially for the inflatable penile prostheses, with recent advances in the devices including reinforced cylinders, kink-proof tubing, pre-connected pumps and antibiotic coating, these risks are lower than ever, and the devices consistently demonstrate good longevity [78–80].
For men who started a regimen of ED therapy post-prostatectomy, the overall treatment discontinuation rate at 18 months post-surgery was 73 % [81]. Reasons for discontinuation included treatment effect below expectation (with or without dose titration) and loss of interest in sex (either patient or partner). Other possible reasons, although not cited in this study, include cost and treatment side effects. It is also established that the use of penile prostheses can significantly improve quality of life [82]. They may, however, be underused: in one SEER-Medicare analysis, approximately 1 % of men post-prostatectomy ultimately underwent penile prosthesis insertion [83]. In another analysis, while it was found that 50 % of men post-prostatectomy elected to try ED therapy, only 1.9 % underwent implantation of penile prosthesis, the least commonly used therapy [84]. It was, however, reported to be the most helpful ED treatment.
Overall, satisfaction rates for penile prostheses are quite high (69–98 %) [85]. Uncommonly, patients may be dissatisfied as a result of the glans not being rigid to the same extent as the penile shaft, also known as “floppy glans syndrome.” In this case, concomitant use of PDE5 inhibitors, IUA [86] or VED [87] may be attempted for supplemental glanular engorgement.
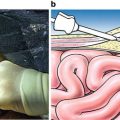
Given the upsurge of robotic-assisted approaches for prostate extirpation, there is scrutiny as to placement of abdomino-pelvic reservoirs for three-piece inflatable devices. For patients status post open radical prostatectomy, typically, reservoirs are easily placed through or adjacent to (traversing through the transversalis fascia) the external inguinal ring into the retropubic space of Retzius. With the robotic approach, this space may be obliterated, and assumed extraperitoneal reservoir placement may in fact be intraperitoneal [88]. This fact has led to the novel approach of ectopic reservoir placement in the abdominal wall [89]. Alternatively, a counter-incision may be employed for safe reservoir placement [90].
Other surgical considerations include the fact that radical prostatectomies are safely performed in men with preexisting inflatable penile prostheses (and their abdomino-pelvic reservoirs) [91–93]. Finally, Ramsawh and colleagues [94] examined the benefits of simultaneous placement of penile prosthesis at the time of radical prostatectomy. The patients who opted for this procedure reported greater overall quality of life, erectile function and more frequent sexual contact than those who underwent RP alone. This may be a reasonable option for patients in whom nerve-sparing is not possible, or who have severe ED refractory to medical options prior to surgery.
Penile Rehabilitation
Penile rehabilitation is defined as medical treatment at the time of or after prostatectomy to improve the restoration of natural penile mechanics which results in spontaneous erectile function [32]. This is different (perhaps subtly) than ED treatment post-prostatectomy, which is characterized by the administration of medication to achieve a more rigid erection which permits penetrative intercourse. In the former, the goal is to bring about recovery of the erectile mechanism so that, at least ideally, the patient is not dependent on any erectile aid, and can generate erections as he did prior to his surgery. The goal of the latter, however, is the attainment of a rigid erection. The importance of this distinction cannot be understated, and many patients and clinicians may not fully appreciate the difference.
The rationale for penile rehabilitation is that the ultimate erectile capacity of the penis is compromised as a result of the chronic absence of erections that the patient experiences postoperatively. Due to this inability to achieve erections, the normal cycling of arterial blood flow to the penis is disrupted and theoretically penile hypoxia results, which leads to intracorporal fibrosis [95]. In preclinical models of post-prostatectomy ED, improved oxygenation of cavernosal tissue, either via hyperbaric oxygen administration or PDE-5 inhibitors, yields improved erectile hemodynamics and prevention of smooth muscle loss and fibrosis [96–100].
Based on this knowledge, it is recommended that some form of treatment or penile rehabilitation be employed following radical prostatectomy, as this “…is undoubtedly better than leaving the erectile tissue to its unassisted, unfavorable fate” [101]. Furthermore, initiating therapy/rehabilitation early postoperatively may confer advantage to commencing in a more delayed fashion, although there is currently insufficient evidence to support specific time recommendations. Indeed, surveys of clinicians reveal that over 80 % recommend some sort of rehabilitation to their patients [102, 103]. Although all treatment options were employed, the most common initial therapy was PDE-5 inhibitors, and treatment was most commonly initiated at catheter removal, and lasted for 12–18 months. There were similar findings for members of the International Society of Sexual Medicine (ISSM) [102], wherein more members had formal sexual medicine training, although treatment duration tended to be for 12 months or less. Interestingly, 97 % of responders did not expect full rigidity with rehabilitation. As well, those clinicians who perform radical prostatectomy or who assessed more than 50 such patients annually were more likely to utilize penile rehabilitation. Finally, for those who do not employ rehabilitation, 50 % cited cost, 25 % the absence of evidence-based therapy, and 25 % the lack of familiarity with penile rehabilitation as their reasons.
The majority of data available for the utility of penile rehabilitation address the use of PDE-5 inhibitors. For many practitioners, they are considered first-line therapy for rehabilitative purposes as well, relating to their ease of use and safety. Bannowsky et al. [104] showed a benefit of nightly low-dose sildenafil (25 mg) in recovery of erectile function in patients following nerve-sparing radical prostatectomy in a small study. Forty-three patients, following catheter removal at 7–14 days following surgery, were studied, with 23 patients randomized to sildenafil 25 mg nightly starting the day following catheter removal, and a control group of 18 patients were followed without sildenafil administration. IIEF scores were then recorded at various timepoints after surgery. Over the course of the first postoperative year, there was a gradual increase in the IIEF scores for patients in both groups. In the nightly sildenafil group, however, there was a significantly higher IIEF score at 36 and 52 weeks post-op, compared to controls (9.6 vs. 6.4, 14.1 vs. 9.3, respectively). At 52 weeks, 47 % of men taking nightly sildenafil were able to achieve and maintain erections sufficient for intercourse, compared to 28 % in the control group (p < 0.001). Furthermore, when on-demand sildenafil 50–100 mg was used for patients in both groups, the overall potency of the nightly sildenafil group increased to 86 % compared to 66 % in the control group. The conclusion of the authors, that “…daily low-dose sildenafil leads to significant improvement in the recovery of erectile function,” is limited by the small patient population and the absence of a true control group (i.e., patients administered a placebo). A higher dose of nightly sildenafil, 50 or 100 mg, and its impact on recovery of erectile function was assessed by Padma-Nathan et al. [105]. In a randomized, double-blind, placebo-controlled study of men having undergone nerve-sparing radical prostatectomy, patients were assigned to placebo, sildenafil 50 mg or sildenafil 100 mg nightly commencing 4 weeks postoperatively for 36 weeks. At 48 weeks, 4 % of the placebo group were deemed to have responded, whereas 26 % of those in the sildenafil 50 mg nightly group were responders, and 29 % of those in the sildenafil 100 mg group were responders (both p < 0.05). Based on these results, the authors concluded that nightly use of sildenafil markedly increased the return of normal spontaneous erections. These conclusions, however, are tempered by the substantial limitations of the study: the small number of patients enrolled, the dropout rate, the significantly lower placebo response rate than that published in the literature, and the non-validated primary outcome of the study (responders were defined based on individual questions from the IIEF-EF, not the overall score).
Vardenafil had been studied for efficacy in improving recovery of erectile function [106]. Of particular importance in this study was that patients underwent unilateral nerve-sparing surgery, and that there was no significant difference between 5 and 10 mg vardenafil dosing in erectile recovery according to the IIEF-5 (equivalent to the SHIM questionnaire). The utility of nightly versus on-demand therapy with vardenafil on erectile function recovery following bilateral nerve-sparing radical prostatectomy was assessed [107]. The design consisted of a 9-month double-blind treatment period, a 2-month single-blind washout period and an optional 2-month open-label period, to start within 2 weeks of surgery. The primary outcome measure was the percentage of subjects with an IIEF-EF score of >22 after the washout period. The intention-to-treat population consisted of 628 men randomized to treatment. Whereas at the end of the treatment period there was noted to be a significantly higher proportion of patients with IIEF-EF > 22 in the on-demand group, there were no significant differences between on-demand and nightly dosing at the end of the washout period. The authors concluded that these results support a paradigm shift toward on-demand dosing in a rehabilitative context in men post-prostatectomy. While certainly interesting, the trial is limited by the potential inexact definition of potency according to the IIEF-EF, as well as the failure to report the number of tablets consumed in the on-demand group. As such, it is unclear (though unlikely) whether patients in the on-demand group used similar doses to those in the nightly dosing group.
There are no clinical studies specifically addressing the role of tadalafil for penile rehabilitation for recovery of erectile function post-prostatectomy.
Montorsi [108] was the first to conceive of a penile rehabilitative concept, utilizing ICI with alprostadil. In that study, after bilateral nerve-sparing radical retropubic prostatectomy, 30 men were randomized into two groups: 15 men underwent alprostadil injection three times per week for 12 weeks, and 15 men observation with no erectogenic treatment. After 6 months, in the control group, only 3/15 (20 %) patients had normal erectile function, compared to the experimental group (8/12–67 %, p < 0.01). Despite there being several notable limitations to this study, including small sample size, preoperative parameters of erectile function and patient comorbidities not discussed and despite the claim of “spontaneous recovery of erections” erectogenic aids still being required, this served as the basis for further studies assessing penile rehabilitation, employing different ED treatments and protocols. Another study of penile rehabilitation involving ICI assessed the combination of intracavernous alprostadil or triple therapy with sildenafil started at the time of hospital discharge following bilateral nerve-sparing radical prostatectomy [109]. Injections were started within 3 weeks of catheter removal. This early combination therapy was shown to facilitate early sexual intercourse, improve patient satisfaction and possibly promote earlier return of spontaneous erections in 22 men. Sildenafil was taken daily and the ICI was done 2–3 times per week until natural erections occurred. The combination also allowed for a lower dose of ICI, which minimized penile discomfort. This study is limited by the small patient number as well as the absence of a control group.
The data supporting the use of the VED in the context of penile rehabilitation exceeds that available for primary ED treatment. In a pilot study of early (starting 1 month postoperatively, daily 10-min device application) VED use, Kohler et al. [110] demonstrated not only better erectile function at 3 and 6 months postoperatively according to the IIEF in the early VED use (compared to a control group), but also maintained stretch penile length, which was significantly shorter in the control group. In another prospective study [111], daily VED use (no constriction ring unless attempting intercourse) was compared to no erectogenic treatment in 109 men starting 1 month following surgery for a total of 9 months. A modest benefit was noted in the VED group for vaginal penetration without erectile aid. While these studies suggest a role for VED in penile rehabilitation, opponents would argue that by virtue of the fact that no more than 60 % of blood drawn to the penis using a VED is arterial [112], the potential benefit of VED in this context is limited compared to treatments which target and are meant to enhance penile arterial blood flow, such as PDE5 inhibitors, ICI or IUA.
IUA has been demonstrated to be of benefit in the rehabilitative setting. In a prospective study of 91 men after bilateral nerve-sparing radical prostatectomy with a median follow-up of 6 months, 56 men treated with 125 or 250 μg of intraurethral prostaglandin E1 three times per week starting 12–15 days after catheter removal reported higher SHIM scores, and had a higher proportion of men recovering spontaneous erections compared to the control group who had no rehabilitative treatment [113]. Notable is the 32 % dropout rate for patients in the IUA group. Drawbacks of this study include lack of intent-to-treat analysis and randomization, and self-selection of intervention, as well as the absence of statistical analysis between groups. In another study [114], a prospective randomized trial comparing nightly intraurethral alprostadil (IUA) versus sildenafil for post-prostatectomy penile rehabilitation was conducted. Two hundred and twelve patients were randomized to receive nightly intraurethral alprostadil IUA (initially 125 μg, with titration up to 250 μg at 1 month post-op) or sildenafil, and were followed up regularly over the first 12 postoperative months. By the end of the study period, there were no differences noted in the IIEF-EF scores or intercourse success rates between the 2 groups. The dropout rate for patients in the IUA group was higher than in the sildenafil group (30 % vs. 19 %), and the drug compliance rate (measured by the dispensed-to-returned medication ratio) was lower (79 % vs. 98 %). The rationale for the use of a subtherapeutic dose (125 μg) of IUA initially was that higher doses may have led to an unacceptably high dropout rate due to local adverse effects. Practically speaking, given the absence of a clear benefit with IUA versus sildenafil, it seems unlikely that clinicians and patients would elect to pursue nightly IUA for rehabilitation when a seemingly more convenient oral therapy yields similar outcomes. Nevertheless, for patients interested in some form of penile rehabilitation, should PDE5 inhibitors be contraindicated due to risk, adverse effect or cost, IUA may be considered (Table 11.2).
Table 11.2
Summary of penile rehabilitative strategies
Treatment | Dose | Regimen | Duration | Success | Level of evidence | Reference |
|---|---|---|---|---|---|---|
Sildenafil | 25 mg | Nightly, starting the day of catheter removal | 52 weeks | Improvement in IIEF-5 | 2b | [104] |
Sildenafil | 50–100 mg | Nightly, starting 4 weeks after surgery | 36 weeks | Improvement in spontaneous EF and satisfaction | 2b | [105] |
Vardenafil | 10 mg nightly; 5/20 mg on demand | Nightly versus on-demand | 9 months | No difference in IIEF-EF between nightly versus on-demand | 1b | [107] |
Alprostadil ICI | Optimized per patient (2.5–14 mcg, mean 8 mcg) | Three times weekly, starting 1 month after surgery | 12 weeks | Recovery of spontaneous erections | 2b | [108] |
Alprostadil/trimix ICI + sildenafil | Alprostadil 1–4 mcg; trimix 20 U; sildenafil 50 mg at the time of hospital discharge | Injections 2–3 times weekly; sildenafil daily | 6 months | 50 % patients recovered partial spontaneous erections | 4 | [109] |
VED | Not specified | Daily starting 2 weeks after surgery | 9 months | Improvement in IIEF-5 in the early daily VED use | 2b | [111] |
MUSE | 125 mcg, with possible titration to 250 mcg | Three times weekly starting 3 weeks after surgery | 9 months | Improvement in SHIM | 4 | [113] |
MUSE (vs. Sildenafil) | 125 mcg (vs. 50 mg sildenafil) | Nightly starting within 1 month of surgery | 9 months | No difference in recovery between MUSE and sildenafil groups | 4 | [114] |
The success of a penile rehabilitative program is not solely defined by the ability for the participants to generate their own erections. Compliance is an important issue to consider: no matter what the potential is for achieving success, should the regimen be too intensive, costly or with too many adverse effects, patients will not adhere to the protocol, may not recover erections, and frustration and mistrust may develop. This unfortunate prospect has been proven: Polito et al. [115] showed that 36.5 % of 430 consecutive radical prostatectomy patients ultimately declined participation in a rehabilitation protocol involving ICI with alprostadil, and of those that participated, 18.6 % eventually withdrew from the program, for a total of 55.1 % of their overall patient cohort not participating in their program. Reasons for declining participation in the program included patient’s lack of sexual interest (51.6 %), lack of interest by the partner (30.2 %), and presence of urinary incontinence (26.7 %), and reasons for withdrawal after initiation of the program included disappointment with treatment efficacy (64.7 %), injection pain (45 %), and difficulties with or fear of performing the injection by themselves or by the partner (35.2 %). Cost of the drug was not cited to be a cause for dropout. Men who declined or withdrew participation were significantly older, had inferior preoperative erectile function and sustained more adjuvant therapy (androgen deprivation and/or radiation therapy) than those who carried out the program. Although the exact rehabilitative regimen with regard to the frequency of injections was not specified, and that these results may not be generalizable to other rehabilitative regimens (especially with other ED treatment modalities), the important takeaway point of this study is that compliance with penile rehabilitation is an important issue to consider.
Another issue to resolve is which patients should be considered for rehabilitation, that is, who is most likely to benefit from a rehabilitative protocol. Briganti et al. [116] attempted to help define this concept, by retrospectively analyzing 435 patients who had undergone bilateral nerve-sparing radical prostatectomy, who were stratified into three groups according to their risk of post-prostatectomy ED. Low-risk patients were those who were below 65 years of age, had a preoperative IIEF-EF score ≥26 and a Charlson Comorbidity Index (CCI) of ≤1; intermediate-risk patients were 66–69 years of age, preoperative IIEF-EF score 11–25 and CCI ≤ 1; high-risk patients were ≥70 years of age, IIEF-EF ≤ 10 and CCI ≥ 2. In the low- and high-risk groups, there was comparable efficacy of a rehabilitative protocol consisting of daily PDE-5 inhibitor use, whereas in the intermediate patient group, daily PDE-5 inhibitor use was associated with significantly greater erectile recovery at 3 years. A similar study by Müller et al. [117] found that on multivariate analysis, factors which predicted lack of success for a rehabilitation protocol (in this study consisting of thrice weekly sildenafil to achieve a penetration-rigidity erection for at least 18 months post-prostatectomy, with ICI to be used if oral therapy failed) included age >60 years, non-bilateral nerve-sparing surgery, presence of two or more vascular comorbidities (hypertension, dyslipidemia, coronary artery disease, diabetes mellitus), initiating the rehabilitation program >6 months after surgery, lack of response to sildenafil by 12 months post-surgery and the need for ICI trimix dosing of >50 units. Based on these two studies, it appears as though several factors, including patient demographic factors (age), preoperative erectile functional status, comorbid status, type of surgery (nerve-sparing), timing of rehabilitation initiation, and response to ED therapy should assist in determining the capacity to respond to a rehabilitation protocol.
Another issue that must be considered is whether penile rehabilitation is cost-effective. Although the cost of the use of these therapies has not been studied specifically in the context of rehabilitation, their cost in treating ED has been examined, with undecided results, with up to tenfold differences noted depending on the analysis [118, 119]. The reasons why an exact cost estimate cannot be ascribed to ED therapy are multiple, and include older studies with dated cost estimates, the upsurge in ED treatment use over time, the inability to capture the opportunity cost of how ED affects other aspects of life (such as other health problems [i.e., depression, relationship discord] and time missed from work) and the limitations of the various methods of answering the question (retrospective claims analyses, decision analytic models). Furthermore, most patients must cover most, or at times, all of the costs associated with ED treatment out of pocket: for example, in the USA, approximately 60 % of sildenafil prescriptions are paid out of pocket [120]. As such, many of the expenses associated with ED therapies are not even accounted for in these studies. Therefore, while an exact monetary figure cannot be estimated for the different therapies either for primary ED treatment or penile rehabilitation, the socioeconomic impact on the patient, as well as society, is not negligible, and should at least be considered, when prescribing these therapies.
Overall, when counseling patients and their partner about the prospect of penile rehabilitation post-radical prostatectomy, many factors should be considered: patient-related (preexisting comorbidities, motivation, recovery from surgery), partner-related (presence or absence of a regular sexual partner, motivation, partner comorbidities which may preclude regular sexual attempts, motivation), and disease-related (pathological stage and need for adjuvant therapy). As in other aspects of managing post-prostatectomy ED, managing patient and partner expectations is critical, and provision of reliable and honest data is important for patients to make their best informed decision about participation in a penile rehabilitation protocol.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree