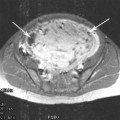
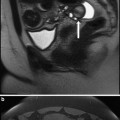
Fig. 1
The position of fibroids in the uterus
It is usually assumed that fibroids only impact on HMB if they are sub-mucous. However, this is an over simplification in that HMB has been reported in those with sub-serosal fibroids, although it is not known if this is causation or association (Sulaiman et al. 2004). Intra-cavity fibroids can also be associated with irregular bleeding since the surface blood vessels may be large and prone to bleed. These are more likely to cause intra-menstrual and irregular bleeding rather than HMB although the evidence for this is circumstantial.
Much of the data comes from ‘before and after’ studies of myomectomy that are difficult to interpret as the site and size may not be clearly defined. Recently, studies looking at the impact of some of the newer treatments such as MR guided high-intensity focused ultrasound that necessitate detailed imaging, suggest that submucosal fibroids do impact on menstrual blood loss. These techniques require absolute definition of the fibroids and allow the relationship with the uterine cavity to be very clearly visualised. HMB has even been reported in the presence of subserosal fibroids, although it would appear that this is less common. The reasons why fibroids at different sites may cause HMB is unclear. It is quite possible that a fibroid within the myometrium might produce cytokines and vaso-active factors that will impact both on the blood supply to the uterus and also endometrial function.
2.2 Importance of Size
It appears that the size of fibroids does not impact on symptoms of HMB or sub fertility to any great extent. It is more the site and the relationship with the endometrium that is of importance. This may not be the case of an intra-cavity fibroid where the surface blood vessels may be large and might be prone to bleed. These are more likely to cause intra-menstrual and irregular bleeding rather than HMB.
2.3 Theoretical Explanation of HMB in Women with Fibroids
There is research data to support an association between heavy periods and uterine fibroids (Fraser et al. 1986). The mechanism by which uterine fibroids increase the blood loss during menstruation is still not fully understood and there are several possible explanations.
1.
Disturbance in the ovarian hormones, it was thought that the number of anovulatory cycles increased leading to an excess of oestrogen. However, no difference in circulating concentrations of steroid hormone has been found between women with fibroids and women with out fibroids.
2.
Increased size of uterine cavity leading to an increased surface area. Studies in dysfunctional uterine bleeding where fibroids are absent have failed to demonstrate any conclusive association.
3.
High vascularity of the uterus associated with fibroids. The fibroids themselves are relatively avascular and only have immature blood vessels running through them. However, there are often very large vessels supplying the fibroid and these are found in the ‘cavity’ between the fibroid and the myometrium.
4.
Venous pooling due to pressure from the fibroids. Compression of fibroids on the venous plexus of the adjacent tissues causes congestion to the myometrium and endometrium lead to abnormal uterine bleeding.
5.
Abnormal uterine contractility in the presence of fibroids may lead to dysmenorrhoea (period pain).
6.
The presence of a uterine factor.
It is well documented that there is a role for factors produced by the endometrium in HMB. The best studied of these are the prostaglandins but others such as endothelin and inflammatory mediators may also be involved (Downie et al. 1974; Maybin et al. 2011). Their role is much less clear than where heavy bleeding occurs in the absence of fibroids and it is also noted that medical treatment does not appear to be so effective in those with fibroids or other pathology.
Endometriosis and adenomyosis are often associated with fibroids especially those that are sub-mucous. Women with fibroids who have HMB should always be investigated to exclude other pathology.
Recent reports suggest that there is a relationship between development of fibroids and the dysregulation of several growth factors or their receptors, leading to vascular dysfunction and angiogenesis which contribute to abnormal vascular function or structure in the uterus, and subsequently to HMB (Munro 2011).
3 Role of Fibroids in Fertility
The place of fibroids in contributing in sub-fertility has been controversial for many years (Farquhar 2009; Latharby and Vollenhoven 2007). Many clinicians assume that if fibroids are present, they must be the cause of the problem but this is not necessarily the case as will be demonstrated in the next section. It is well-known that fibroids are extremely common in women of reproductive age, and therefore it is not surprising that many of those presenting with sub-fertility are found to have them within their uterus. On the other hand, many of those who achieve a pregnancy also have fibroids and do not experience any difficulty in becoming pregnant. It is difficult to be sure of the exact incidence of fibroids as the studies depend on the population involved and also the enthusiasm with which fibroids have been identified. The widespread use of ultrasonography has resulted in an increase in the diagnosis of uterine fibroids in those who are asymptomatic and have unexplained infertility
There is very little evidence that fibroids impair fertilisation itself. This might occur in the presence of an anatomical distortion of the tubal ostia or if fibroids produced factors that impaired the process although there is no evidence of this. Fibroids that impinge on the cavity could lead to abnormalities of endometrial function which would inhibit implantation or may alter uterine contractility, although the role in fertility is unknown.
Much of the evidence has been obtained by looking at the results of myomectomy. These are largely uncontrolled, and therefore make the drawing of conclusions very difficult. Some clarity has been introduced to the discussion by studying the role of fibroids on the results of assisted conception which gives a greater insight into their role in implantation and will be discussed in greater detail below.
4 Non-medical Treatment of Fibroids and Impact on Fertility
4.1 Myomectomy
It would appear that overall, the myometrium heals well after a myomectomy, although there is a fear that hysteroscopic myomectomy can lead to extensive damage and scarring in the uterine cavity. Removal of intramural or subserosal fibroids will often lead to some bleeding. If this is very heavy then hysterectomy may be required as a life saving procedure. However, even the smallest amount of bleeding can lead to adhesion formation, which could impair fertility in the future.
There are few data on the outcome of myomectomy beyond these already alluded to, so that the place is very uncertain and further research is undoubtedly required.
4.2 Uterine Artery Embolisation
The impact of uterine artery embolisation on fertility is extremely controversial, and thus there are many who believe that it should not be used in women wishing to conceive. However, as the above discussion has outlined, this is often because studies do not compare like with like since they have not been randomised. There have been successful pregnancies in women following uterine artery embolisation, but it would appear there might be an increased incidence of problems in pregnancy, although it is difficult to know whether the increase is due to the technique itself or the fact that the women has uterine fibroids. The role of embolisation increasing fertility is discussed elsewhere in this book and will not be further developed here.
5 Outcomes in the Studies of Infertility
When studying fertility, there are multiple outcomes reported in most papers. These start with what are called ‘chemical pregnancy rates’, which act as a surrogate for implantation since there is a rise in human chorionic gonadotrophin (the hormone used to diagnose pregnancy). This level may drop before the time of a missed period but can be used to confirm that ‘pregnancy’ did occur. The next parameter tends to be ‘on going’ pregnancy rate in relation to the gestation of the pregnancy which usually relates to miscarriage rates that are defined as first trimester (up to 12 completed weeks) and second trimester (from 13 completed to 28 weeks of pregnancy). Preterm labour occurs before 37 completed weeks and then term from 37 to 42. Live or ‘take home’ baby rate at term are obviously the most important outcomes for the women in question.
There have been three systematic reviews of the role of fibroids and reproductive outcomes (Klatsky et al. 2008; Pritts et al. 2009; Somigliana et al. 2007). In addition, a consensus statement was produced from a group in Australia that included that all these reviews and also additional studies, but did not generally alter any of the conclusions (Kroon et al. 2011




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree