Primary Ciliary Dyskinesia
Melissa L. Rosado-de-Christenson, MD, FACR
Key Facts
Terminology
Primary ciliary dyskinesia: Genetic disorder of ciliary structure resulting in impaired mucociliary clearance
Kartagener syndrome: Situs inversus, sinusitis, bronchiectasis
Imaging Findings
CT & HRCT
Bronchiectasis, bronchial wall thickening
Centrilobular nodules, tree-in-bud opacities
Mucus plugs, bronchial air-fluid levels
Peribronchial airspace disease
Radiography
Hyperinflation
Bronchial wall thickening, bronchiectasis
Atelectasis, consolidation
Situs inversus or dextrocardia (50%)
Top Differential Diagnoses
Cystic Fibrosis
Allergic Bronchopulmonary Aspergillosis (ABPA)
Postinfectious Bronchiectasis
Immune Deficiency Disorders
Young Syndrome
Pathology
Abnormal ciliary ultrastructure &/or function
Clinical Issues
M:F = 1:1
Typical presentation in early childhood, but many patients are symptomatic since birth
Recurrent rhinosinusitis, otitis, and pulmonary infection; male infertility
Good prognosis with aggressive prophylaxis and treatment
TERMINOLOGY
Abbreviations and Synonyms
Primary ciliary dyskinesia syndrome (PCD)
Includes all genetic disorders that cause ciliary defects and impaired mucociliary clearance
Synonyms
Dyskinetic cilia syndrome, immotile cilia syndrome
Note ciliary motion is usually present but abnormal
Definitions
Primary ciliary dyskinesia syndrome
Abnormal ciliary ultrastructure with resultant mucociliary dysfunction and sinopulmonary disease
Abnormalities of situs in 50% of cases (including situs inversus and situs ambiguous)
Kartagener syndrome: 50% of PCD
Triad of situs inversus, sinusitis or nasal polyposis, and bronchiectasis
Is subset of PCD
Kartagener-Afzelius syndrome: Kartagener described sinusitis, bronchiectasis, and situs inversus; Afzelius described associated infertility
IMAGING FINDINGS
General Features
Best diagnostic clue: Triad of abnormal situs, bronchiectasis, and sinusitis
Patient position/location: Bronchiectasis with predilection for middle and lower lobes
Size: Bronchial dilatation ranges from mild to severe
Morphology: Bronchial dilatation, bronchial wall thickening, and surrounding airspace disease
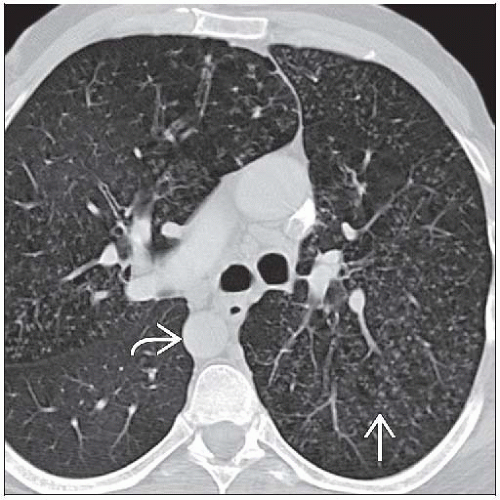
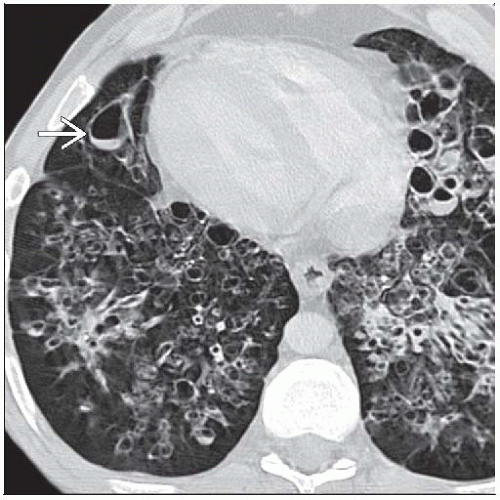
CT Findings
Bronchial wall thickening
Bronchiectasis with predilection for lingula, middle and lower lobes
Variable severity: Cylindrical, varicose, and cystic
Signet-ring sign; bronchial diameter > adjacent pulmonary artery
CT section perpendicular to bronchial long axis
“Ring” is dilated bronchus
“Stone” is adjacent pulmonary artery
Mucus plugs within dilated airways
Centrilobular nodules and tree-in-bud opacities
Peribronchial airspace disease
Ground-glass opacity
Consolidation
Mosaic attenuation, air-trapping on expiratory CT
Atelectasis, often segmental
Findings of prior pulmonary resection
Associated conditions
Abnormalities of situs
Situs inversus
Situs ambiguous
Congenital heart disease
Sinusitis
Radiographic Findings
Hyperinflation
Bronchial wall thickening
Bronchiectasis of variable severity
Atelectasis
Consolidation, may be recurrent
Dextrocardia and abnormalities of situs
Findings of prior pulmonary resection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree