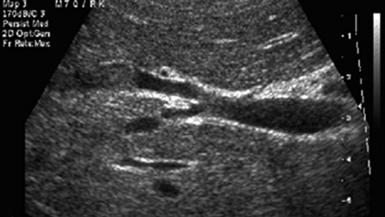
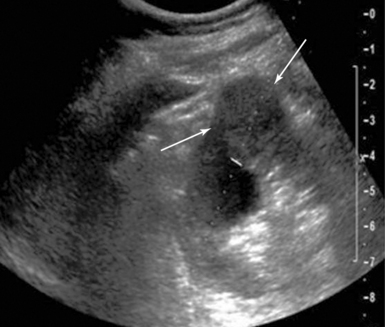
44 Primary hepatocellular carcinoma usually occurs in the setting of dense cirrhosis, which makes visualization and palpation difficult. Furthermore, many hepatomas are smaller than 5 cm and are not fully evident by exploration and palpation alone. IOUS aids with anatomic localization, definition of satellite lesions, and imaging of segmental/subsegmental vascular invasion of the portal or hepatic veins (Figure 44-1). Figure 44-1 Intraoperative ultrasound (IOUS) image of hepatocellular carcinoma invading the right hepatic vein. An isoechoic mass protrudes into the lumen of the vein in a cirrhotic liver. The same principles apply to hepatic metastases of all tissue types. IOUS has higher (>90%) sensitivity and specificity than preoperative computed tomography (CT), US, or surgical inspection in screening for these lesions, largely because IOUS detects tumors less than 1 cm.1 When performed as a routine screening procedure during colorectal resections, occult metastases are identified nearly 10% of the time. Likewise, in determining resectability of other intra-abdominal malignancies (pancreas, gallbladder, stomach), identification of occult metastases in the liver dramatically changes the surgical approach from curative to palliative intent. The results of many studies show that IOUS changes the clinical management in up to 50% of patients undergoing hepatic resection for malignancy. Even when intraoperative US does not change surgical management, it results in corrected staging and, consequently, alters postoperative treatment in 11% of patients.2,3 Bloed et al4 showed that despite preoperative triphasic CT, intraoperative US still provided additional useful information in 50% of their patients, which resulted in a change in the surgical procedure in 15%. In a study done at Royal Prince Alfred Hospital, 20 of 30 hepatic resections (67%) were changed or guided by IOUS. IOUS detected 26 more metastases (44%) in 10 of 19 patients (1-5 per patient). Two patients had preoperatively suspected metastases refuted by IOUS-guided biopsy. Eight of the 11 patients (73%) undergoing resection of primary carcinoma of the liver had the planned procedure changed or guided by IOUS.5 IOUS has equivalent efficacy while providing cost and time savings when compared with cholangiography in biliary disease and has great utility in identifying common bile duct (CBD) pathology during open operations, especially because these procedures typically occur amidst inflammation, malignancy, or prior surgery. In cases of unresectable disease, biopsy can be guided by IOUS, and during reconstructive procedures, transhepatic biliary stent placement can be facilitated. In a recent study, IOUS identified significant biliary abnormalities in 20 patients (40%) undergoing cholecystectomy, including a foreshortened cystic duct (<1 cm) in 7 patients (14%), CBD stones in 4 patients (8%), abnormal cystic duct anatomy in 4 patients (8%), and abnormal vascular anatomy in 8 patients (16%).6 The relationship of renal tumor to structures deeper within the sinus may be more readily appreciated using IOUS. In a series of patients with hereditary renal carcinoma, IOUS identified tumors that were undetectable by the surgeon in 25% of cases, some as large as 4 cm, of which 50% were pathologically proven renal cell carcinoma (Figure 44 E-1). Figure 44 E-1 A renal cell carcinoma is identified as a rounded mass extending off the posterior kidney (arrows). Note the dark area next to the mass, which represents a renal cyst.
Procedural ultrasound for surgeons
(CONSULTANT-LEVEL EXAMINATION)
Liver
Gall bladder
Kidney
Radiology Key
Fastest Radiology Insight Engine