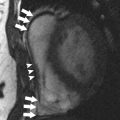
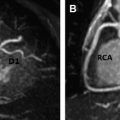
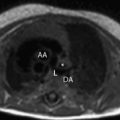
The role of cardiac magnetic resonance (MR) imaging as a prognostic tool in patients with ischemic heart disease is well established. However, an increasing body of data now demonstrates that cardiac MR imaging can provide prognostic information in a variety of nonischemic and diffuse myocardial diseases including myocarditis, dilated and hypertrophic cardiomyopathies, sarcoidosis, amyloidosis, and arrhythmogenic right ventricular cardiomyopathy. Cardiac MR imaging can also supply incremental information above established prognostic indicators, providing an additional tool for use in the prediction of disease progression, response to treatment, and risk stratification. An increasing body of data demonstrates that cardiac magnetic resonance (MR) imaging can provide prognostic information in a variety of nonischemic and diffuse myocardial diseases, including myocarditis, dilated and hypertrophic cardiomyopathies, sarcoidosis, amyloidosis, and arrhythmogenic right ventricular cardiomyopathy. Cardiac MR imaging can also supply incremental information above established clinical prognostic indicators, providing an additional tool for use in the prediction of disease progression, response to treatment, and risk stratification. The role of cardiac magnetic resonance (MR) imaging as a prognostic tool in patients with ischemic heart disease is well established, and MR imaging has been widely trusted in making clinical decisions regarding suitability for coronary revascularization. Recent efforts from the scientific imaging community have focused on the potential prognostic role of MR imaging biomarkers in patients with nonischemic myocardial diseases. In particular, delayed-enhancement cardiac MR imaging has been interrogated as a tool for risk stratification and treatment guidance in patients diagnosed with nonischemic cardiomyopathies and myocarditis. This article discusses current evidence on the role of MR imaging as a prognostic tool in these patients, with special focus on incremental value of cardiac MR imaging over well-established prognostic indicators. The clinical research community has recently focused on trials to establish the use of MR imaging beyond a precise diagnostic tool, focusing on guidance of treatment strategies and identification of high-risk patients. Cardiac MR imaging can generate imaging biomarkers that have the potential to predict disease progression and patient response to specific treatment strategies, and to identify patients at risk for disease-specific mortality who may require more aggressive management. More importantly, MR imaging techniques for quantification of regional myocardial function and tissue characterization are able to identify cardiac abnormalities at a subclinical stage, allowing for early interventions to prevent the development of symptomatic disease. In patients with viral myocarditis, the classic mortality predictors in clinical practice are related to severity of clinical symptoms, decreased systolic function, and left ventricular enlargement. These parameters are quantified using the New York Heart Association (NYHA) class, left ventricular ejection fraction (LVEF), and left ventricular end-diastolic volume index (LVEDVi), respectively. In addition to providing accurate and reproducible quantification of LVEF and LVEDVi, MR imaging can demonstrate areas of abnormal signal on delayed-enhancement images, which have been associated with worse outcome in patients with myocarditis ( Fig. 1 ). A recent study including 222 patients with biopsy-proven myocarditis and a follow-up of 4.7 years has shown that the presence of delayed enhancement has a hazard ratio of 12.8 for all-cause mortality and 8.4 for cardiac mortality. In addition, this study showed that delayed-enhancement MR imaging had a hazard ratio significantly higher than that for LVEF, LVEDVi, and NYHA class. The presence of delayed enhancement has been described as a common feature in patients with chronic heart failure from myocarditis, supporting the hypothesis that the presence of scar on MR imaging is associated with worse clinical disease. Quantification of left ventricular systolic function, measured by LVEF, is a well-established indicator of prognosis in patients with nonischemic dilated cardiomyopathy, and can be precisely determined with volumetric cardiac MR imaging analysis. It has been recently demonstrated that the presence of delayed enhancement on cardiac MR imaging also indicates a worse prognosis in patients with dilated cardiomyopathy ( Fig. 2 ). Gulati and colleagues have shown that patients with myocardial fibrosis on delayed-enhancement imaging have significantly higher mortality rate in comparison with patients without abnormalities on delayed-enhancement imaging, with a hazard ratio of 2.96 (95% confidence interval [CI] 1.87–4.69) and an absolute risk difference of 16.2% (95% CI 8.2%–24.2%). In addition, abnormal delayed-enhancement imaging had an incremental role in prognostication of patients with dilated cardiomyopathy when compared with LVEF alone, with a significant improvement in risk reclassification for all-cause mortality and a sudden cardiac death composite. Assomull and colleagues have previously shown that the presence of mid-wall fibrosis in patients with dilated cardiomyopathy was associated with a higher rate of a predefined primary combined end point of all-cause mortality and hospitalization for a cardiovascular event (hazard ratio 3.4, P = .01), independently of ventricular remodeling.
Key points
Introduction
MR imaging as a prognostic tool
Disease-specific considerations
Myocarditis

Dilated Cardiomyopathy