SONOGRAM ABBREVIATIONS
AFMS Anterior fibromuscular zone
Bl Bladder
CZ Central zone
ED Ejaculatory duct
Ip Iliopsoas muscle
NVB Neurovascular bundle
Ob Obturator muscle
Pr Prostate gland
PZ Peripheral zone
SP Symphysis pubis
SV Seminal vesicle
TZ Transitional zone
UR Urethra
KEY WORDS
Anterior Fibromuscular Stroma. Smooth muscle that forms the anterior surface of the prostate.
Apex. Inferior region of the prostate.
Base. Superior region of the prostate.
Benign Prostatic Hypertrophy (BPH). Nonmalignant enlargement of the glandular component of the prostate. The true prostate forms a shell around the enlarged gland. Common in older men.
Central Zone. Portion of the prostate that surrounds the urethra and encases the ejaculatory ducts. It is located at the prostatic base. It is typically the site of BPH but is rarely affected by prostate cancer. Accounts for 20% to 25% of the prostate glandular tissue.
Corpora Amylacea. Calcification within the prostate.
Ejaculatory Ducts. Paired ducts that connect the seminal vesicle and the vas deferens to the urethra at the verumontanum.
Neurovascular Bundle. Grouping of nerves, veins, and arteries located on the posterolateral aspect of the prostate at the junction of the seminal vesicles. Sonographically they appear hyperechoic.
Peripheral Zone. Comprises the posterior, lateral, and apical aspects of the prostate. The peripheral zone is the most common site for prostate cancer. It accounts for 70% of the prostate.
Prostate-Specific Antigen (PSA). A protein produced by the prostate gland. PSA levels may become elevated in the blood secondary to prostate cancer, BPH, or prostatitis.
Prostatitis. Inflammation of the prostate.
Seminal Vesicles. Paired glands that lie posterior and lateral to the base of the prostate. Responsible for producing fluid in which sperm move and are nourished.
TNM Classification. Staging technique for prostate cancer. “T” refers to tumor size, “N” refers to lymph node involvement, and “M” refers to the presence of metastasis.
Transitional Zone. Two small glandular areas located on either side of the proximal urethra. Comprises approximately 5% of the gland. It cannot be distinguished from the central zone by ultrasound.
Transurethral Resection of the Prostate (TURP). Surgical procedure most often used to treat men with BPH. A portion of the prostate is removed by a cystoscope to relieve pressure on the urethra.
Urethra. Canal through which urine is drained from the bladder. The urethra passes through the center of the prostate.
Vas Deferens. The ducts that convey sperm from the epididymis to the urethra.
Verumontanum. Junction of the ejaculatory ducts with the urethra.
RELEVANT LABORATORY VALUES:
PSA (Prostate-Specific Antigen)
Less than 4 ng/mL is normal.
More than 10 ng/mL increases the risk of prostate cancer by 67%.
The Clinical Problem
The most common diseases to affect the prostate are benign prostatic hypertrophy (BPH), prostatic cancer, and prostatitis.
BENIGN PROSTATIC HYPERTROPHY
BPH is common in older men. As the name implies, it is a benign hypertrophy of the prostate. Although the exact cause is not completely understood, diminished androgen secretion is thought to be involved. Histologically, the transitional and central zones of the prostate undergo hypertrophy, resulting in an increase in fibromuscular stroma. The enlarged prostate obstructs the outflow of urine by compressing the prostatic urethra. Symptoms include a poor urinary stream and frequent urination. Hydronephrosis may occur secondary to urethral obstruction. Ultrasound can be used to determine:
1. the size of the prostate, which determines the type of treatment.
2. the amount of postvoid residual urine in the bladder.
3. the presence of hydronephrosis.
PROSTATE CANCER
Prostate cancer is the second most common cancer in American men. More than 70% of prostate cancers are diagnosed in men over 65 years of age. The disease is much more common in African-American men then in white men. It is less common in Asian and American Indian men. A man’s risk of developing prostate cancer is elevated if he has an affected father or brother. Prostate-specific antigen (PSA) is a blood test that is usually elevated in the presence of prostate cancer, but may also be elevated by BPH or prostatitis. PSA levels also increase with age. Many unsuspected cancers are found when a PSA is performed on a screening basis. If symptoms are present, they usually include difficult or painful urination. In the setting of an increased PSA or an enlarged prostate by digital rectal examination, ultrasound can be used to identify the presence of a prostatic mass. However, not identifying a focal mass does not decrease the risk of prostate cancer being present. Ultrasound is also used to:
1. aid in the biopsy of patients with increased PSA.
2. attempt to stage periprostatic spread.
3. guide radiotherapy treatment.
PROSTATITIS
Prostatitis is defined as inflammation or infection of the prostate gland. Prostatitis is usually classified as acute, chronic, or noninfectious. Acute and chronic infectious prostatitis are caused by bacteria and treated with antibiotics. Noninfectious prostatitis is a chronic condition not caused by bacteria. Causes are not fully understood but may include mechanical or chemical trauma, or an autoimmune process. The role of sonography in acute prostatitis may be limited. In many cases, the patient may not be able to tolerate the transrectal ultrasound secondary to pain.
Anatomy
SEMINAL VESICLES AND VAS DEFERENS
The two paired seminal vesicles lie posterior to the bladder and superior to the prostate (Figs. 26-1 and 26-2). Typically, they are symmetric in size, homogeneous, and hypoechoic. The internal fluid is usually simple, but complex fluid may also be visualized. The size of the seminal vesicles is variable.
The vas deferens inserts on the medial aspect of the seminal vesicle to form the bilateral, paired ejaculatory ducts (Fig. 26-1).
PROSTATE
The prostate is a pear-shaped organ with the urethra running through the center. The base is the superior end closest to the bladder. The inferior margin is the apex. At the apex of the prostate lies a thin muscular structure, the urogenital diaphragm, separating the prostate from the penile structures. Sonographically, the normal prostate gland is homogeneous, with the fibromuscular stroma appearing slightly more hypoechoic.
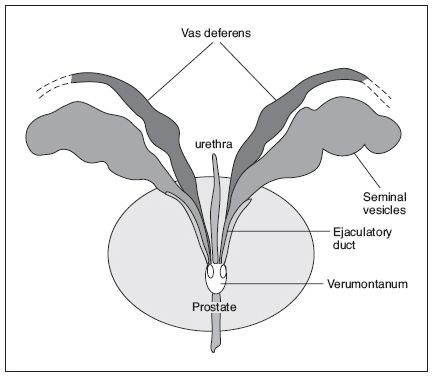
Figure 26-1. ![]() Diagram showing the relation of the seminal vesicles to the vas deferens. Both structures empty into the ejaculatory duct that ends at the verumontanum.
Diagram showing the relation of the seminal vesicles to the vas deferens. Both structures empty into the ejaculatory duct that ends at the verumontanum.
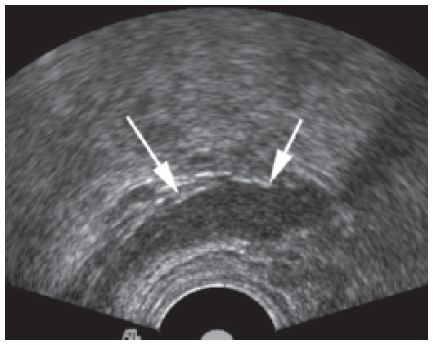
Figure 26-2. ![]() Normal view of a seminal vesicle (arrows) by transrectal ultrasound imaging.
Normal view of a seminal vesicle (arrows) by transrectal ultrasound imaging.
The central and transitional zones surround the urethra. Cupping the central and transitional zones posteriorly is the peripheral zone. The peripheral zone is relatively larger at the apex. The peripheral zone is typically isoechoic to the central and transitional zones.
EJACULATORY DUCTS
The ejaculatory ducts run alongside the peripheral zones within the prostate, from the seminal vesicles to the verumontanum. They are normally quite small but are visible by ultrasound (Figs. 26-1 and 26-3).
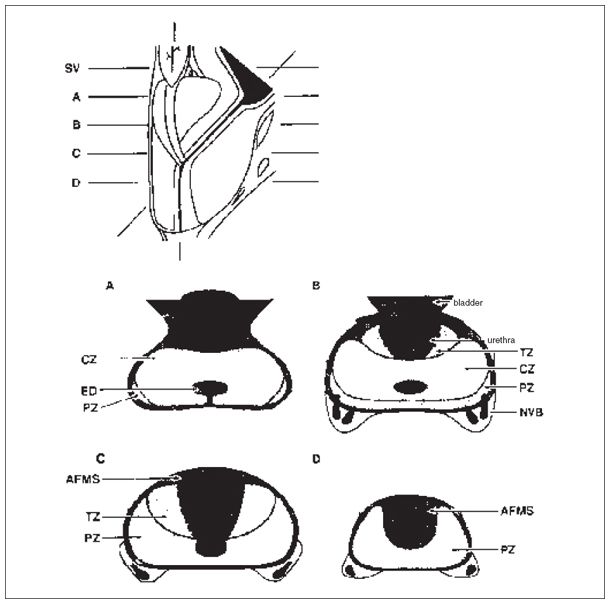
Figure 26-3. ![]() Diagram of the longitudinal and transverse anatomy of the prostate, showing the location of the central (CZ), transitional (TZ), peripheral (PZ), and fibromuscular zones (AFMS). The neurovascular bundles are seen at the posterolateral aspect (NVB). (Adapted from Villers A, Terris MK, McNeal JE, et al. Ultrasound anatomy of the prostate. J Urol 1990;143:732–738, with permission.)
Diagram of the longitudinal and transverse anatomy of the prostate, showing the location of the central (CZ), transitional (TZ), peripheral (PZ), and fibromuscular zones (AFMS). The neurovascular bundles are seen at the posterolateral aspect (NVB). (Adapted from Villers A, Terris MK, McNeal JE, et al. Ultrasound anatomy of the prostate. J Urol 1990;143:732–738, with permission.)
The normal prostate volume is less than 20 mL in younger men. In older men, prostate volumes greater than 40 mL are considered enlarged. Volume is calculated using the formula for a prolate ellipse:
Length × Width × Height × 0.523
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


