CHAPTER 100 Pulmonary Edema
Pulmonary edema is frequently classified as hydrostatic edema (e.g., cardiogenic pulmonary edema) or edema caused by increased capillary permeability (e.g., noncardiogenic pulmonary edema or capillary leak). Often, chest radiographs of patients with pulmonary edema are not as easily classified in such a dichotomous fashion. The following pulmonary edema classification has been proposed to better accommodate the histopathologic, physiologic, and radiographic findings of these patients1:
HYDROSTATIC PULMONARY EDEMA
Imaging Techniques and Findings
Radiography
The chest radiographic findings of hydrostatic pulmonary edema are detailed in Box 100-1. These findings are all more reliably distinguishable on posteroanterior (PA) and lateral chest radiographs than on portable radiographs, but commonly patients with the greatest likelihood of hydrostatic pulmonary edema will be imaged using an anteroposterior technique (AP). AP techniques can make the diagnosis of hydrostatic pulmonary edema difficult because heart magnification, resulting from the considerably shorter focus-film distance as well as projectional magnification, can render determination of cardiac size unreliable, particularly in patients with low lung volumes. Additionally, pulmonary vascular congestion is difficult to determine accurately in nonerect patients because upper lobe vessels frequently normally appear larger than lower lobe vessels for patients imaged in a supine or semierect position. Furthermore, azygos vein dilation, often considered an indicator of elevated right atrial pressure, is a common and potentially normal finding on supine radiographs. Finally, pleural effusions often appear only as hazy attenuation projecting over lungs in patients imaged in a supine or semierect position. However, this appearance is not specific for pleural effusion and can be seen with extensive posterior atelectasis because anterior aerated lung superimposes on the increased opacity of the posteriorly located atelectatic lung. This pattern is often seen in severely ill patients and patients in the intensive care unit, which is the same patient population at risk for hydrostatic pulmonary edema.
The first chest radiographic signs of pulmonary venous hypertension include pulmonary vascular redistribution, appearing as equalization of the size of the upper and lower lobe vessels, which progresses to the upper lobe vessels becoming larger than those in the lower lobes (a reversal of the normal situation). In the acute setting, this phenomenon is seen with left atrial (wedge) pressures in the range of 12 to 19 mm Hg.2 In chronically compensated patients, such as those with mitral stenosis, upper and lower lobe vascular equalization and reversal will occur with left atrial pressures between 15 to 25 mm Hg.2 As the physiologic derangements worsen, pulmonary venous hypertension progresses to frank interstitial pulmonary edema, with the development of interlobular septal thickening, often referred to as Kerley A and B lines (Fig. 100-1A), perihilar indistinctness and vascular haze (see Fig. 100-1B), peribronchial cuffing (see Fig. 100-1C), and subpleural edema (see later).2 Findings of interstitial edema usually are apparent on the chest radiograph, with left atrial pressures of 20 to 25 mm Hg in the acutely ill patient and 25 to 30 mm Hg in chronically compensated patients.2 At higher left atrial pressures, frank alveolar edema occurs, with spillage of fluid into the air spaces. In these patients, the chest radiograph will show an air space consolidation pattern (see Fig. 100-1D) and acinar nodules,2 often superimposed on findings of interstitial edema. The relationship between left atrial (pulmonary capillary wedge) pressure and radiographic findings is not precise, and the radiographic findings often lag behind the physiological changes. Furthermore, stepwise progression through these phases is not always seen, and some imaging findings of hydrostatic edema may be present in the absence of others.
CT
On thoracic CT, findings of hydrostatic pulmonary edema include those seen on chest radiographs, such as cardiomegaly, vascular engorgement, and pleural effusions. Findings of interstitial edema (see later), are also apparent and are more readily appreciable with thoracic CT, particularly high-resolution CT (HRCT), than with chest radiography. Bronchial wall thickening, smooth interlobular septal thickening (Fig. 100-2), and ground-glass opacity (often with hazy, poorly defined centrilobular nodules) are highly suggestive of hydrostatic pulmonary edema.
Classic Signs
Interstitial Edema
The findings of interstitial edema on chest radiography (see Box 100-1) are usually readily visible with CT scanning and, in addition to the findings noted, ground-glass opacity and centrilobular nodules are frequently present in patients with hydrostatic pulmonary edema.
Interlobular Septal Thickening (Kerley A and B lines)
Both Kerley A and B lines represent thickened interlobular septae. Kerley B lines are horizontal linear opacities, 1 to 2 cm in length, in contact with the pleural surface. Kerley B lines are most readily visible in the inferior and lateral aspects of the thorax, near the lateral costophrenic sulcus (see Fig. 100-1A). The regular appearance of Kerley B lines in the lung bases is the result of the regular organization of pulmonary lobules at the lung bases.
The interlobular septal thickening resulting from hydrostatic pulmonary edema is readily visualized on thoracic CT, especially HRCT. Interlobular septal thickening in patients with hydrostatic pulmonary edema is smooth and often most readily visualized in the lung bases and in the pulmonary apices (Fig. 100-2). Poorly defined, ground-glass attenuation centrilobular nodules or lobular ground-glass opacity often coexists.
Vascular Indistinctness and Perihilar Haze
Perihilar haze is a term occasionally used to refer to poor definition of and slightly increased opacity surrounding the perihilar vessels; it manifests as perihilar vascular indistinctness with a hazy or ground-glass appearance (see Fig. 100-1B). Although not always easily recognizable, perihilar haze can be a useful finding that suggests hydrostatic pulmonary edema in patients with lower lobe atelectasis.
Peribronchial Cuffing
Peribronchial cuffing represents bronchial wall thickening, possibly accompanied by a variable amount of peribronchial interstitial fluid. Peribronchial cuffing is most readily recognizable in the central and perihilar regions of lung, when bronchi are seen in cross section (see Fig. 100-1C). Peribronchial cuffing may also be seen as a tram-track appearance when bronchi are visualized in longitudinal section. Peribronchial cuffing may also appear as nonspecific thickening of the interstitium radiating outward from the hilum. On thoracic CT, peribronchial thickening or cuffing usually appears as bronchial wall thickening. Peribronchial cuffing may represent a finding of interstitial edema in the proper clinical setting, but is not specific for that diagnosis; peribronchial inflammation or tumor may also produce this finding.
Air Space (Alveolar) Edema
As factors producing interstitial edema progress, eventually interstitial fluid will begin to accumulate within the air spaces, producing air space edema. Because the edema fluid replaces air within the alveoli, air space edema represents a form of air space consolidation and appears as a confluent opacity (see Fig. 100-1D), which may be accompanied by air space or acinar nodules.
Distribution of Hydrostatic Edema
Hydrostatic edema may assume a number of different distributions, although a symmetric perihilar and basilar predominant distribution is most common. A distinct perihilar distribution of hydrostatic edema is often referred to as a bat wing or butterfly distribution, and is often seen when edema fluid accumulates rapidly. Uncommonly, hydrostatic edema will accumulate in a reverse bat wing distribution reminiscent of other causes of peripheral lung opacity. Other variations in the distribution of hydrostatic edema are frequently recognized (Box 100-2).2




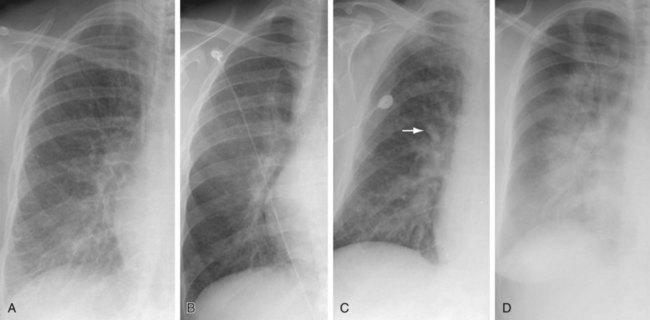
 FIGURE 100-1
FIGURE 100-1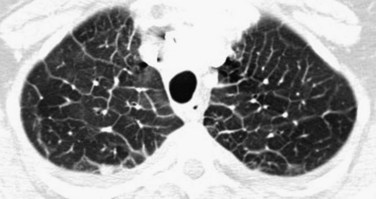
 FIGURE 100-2
FIGURE 100-2







