Etiology, Prevalence, and Epidemiology
Pulmonary hamartomas are benign neoplasms, probably derived from bronchial wall mesenchymal cells. Hamartomas are the most common benign pulmonary neoplasm and account for about 8% of primary lung tumors. Although they may be seen in adolescents and young adults, most cases occur in patients older than 40 years; the peak incidence is in the seventh decade of life. Men are affected two to three times more often than women. Endobronchial hamartomas are much less common than parenchymal lesions, accounting for 5% to 20% of pulmonary hamartomas.
Although hamartomas are benign neoplasms, they may rarely coexist with pulmonary carcinoma. Occasionally, they may be multiple. Multiple pulmonary hamartomas may be part of the Carney triad or, rarely, the Cowden syndrome. The Carney triad consists of pulmonary chondroma (often multiple), gastric epithelioid leiomyosarcoma, and functioning extraadrenal paraganglioma. This rare disease usually affects women younger than 35 years. It is recommended that patients with multiple pulmonary hamartomas have further examinations to rule out gastric leiomyosarcoma and extraadrenal paragangliomas.
Pathophysiology
Most hamartomas are solitary, well-circumscribed, slightly lobulated tumors located within the parenchyma, usually in a peripheral location. Most measure 1 to 4 cm in diameter, but tumors 25 cm in diameter have been described. On cut section the tumors consist of lobules of white, cartilaginous-appearing tissue. Histologically, the lobules are often composed of a central area of more or less well-developed cartilage surrounded by loose fibroblastic tissue. Adipose tissue, smooth muscle, and seromucinous bronchial glands also may be seen. Calcification and ossification of the cartilage can be present and are occasionally extensive. Although endobronchial hamartomas can be morphologically identical to the parenchymal variety, more often they appear as fleshy, polypoid tumors attached to the bronchial wall by a narrow stalk. Endobronchial hamartomas typically contain more macroscopic fat than parenchymal hamartomas.
Manifestations of the Disease
Radiography
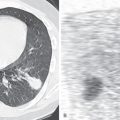
The radiologic manifestations of parenchymal tumors usually consist of a well-circumscribed, smoothly marginated solitary nodule without lobar predilection ( Fig. 20.1 ). Most are smaller than 4 cm in diameter. Although calcification has been identified pathologically in 15% of tumors in some series, it is visible on the chest radiograph in less than 10% of cases. The radiographic pattern of calcification may resemble popcorn; although virtually diagnostic, this appearance is uncommon. Endobronchial hamartomas usually manifest radiographically by the effects of airway obstruction with distal atelectasis and obstructive pneumonitis ( Fig. 20.2 ). The endobronchial lesion is uncommonly visible.


Computed Tomography
The characteristic finding on CT consists of a sharply defined, smoothly marginated nodule. Up to 60% of larger hamartomas have focal areas of fat density (see Fig. 20.1 ). The presence of fat can be ascertained by comparison of the areas of low density with that of subcutaneous fat or by measurement of attenuation values (fat can be considered present when the CT attenuation values are −40 to −120 Hounsfield units (HUs) in at least eight voxels). In review of the CT findings in 47 hamartomas, CT allowed diagnosis in 28 (60%) cases by identifying the presence of fat or fat alternating with areas of calcification ( Fig. 20.3 ). Of the remaining cases, 17 showed no discernible calcium or fat (the diagnosis being made by other means), and 2 revealed diffuse calcification. Hamartomas also may manifest as nodules with soft tissue attenuation and single or multiple foci of calcification. Multiple coarse foci of calcification are referred to as “popcorn calcification” (see Fig. 20.2 ). With the increasing use of CT, smaller hamartomas are being detected but often lack diagnostic CT features. In a recent review of 21 cases of pathologically proven hamartomas (median diameter, 10 mm), none had characteristic internal fat or calcification, but all were well circumscribed with a round or lobular shape ( Fig. 20.4 ). Occasionally, pulmonary hamartoma may have the appearance of a collection of multiple tiny nodules. This appearance results when pulmonary alveoli and bronchioles are entrapped within the hamartoma with tumor buds appearing in a multicentric manner. Serial chest radiographs or CT may show slow growth, with a doubling time usually greater than 450 days ( Fig. 20.5 ).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree