Pulmonary Infections
Ramesh S. Iyer, MD
LEARNING OBJECTIVES
1. Describe typical radiographic features of viral bronchiolitis.
2. Recognize lobar pneumonia, bronchopneumonia, and atypical patterns of bacterial infections.
3. Identify round pneumonia, and recommend appropriate management.
4. Identify cavitary necrosis on radiography and CT.
5. Discuss the imaging appearances of simple and complicated parapneumonic pleural effusions, and empyema.
6. Describe the imaging manifestations of primary tuberculosis.
7. Describe the imaging findings in fungal pneumonia.
INTRODUCTION
Pulmonary infections are a leading cause of morbidity and mortality in children, and are among the most common reasons for pediatric imaging.1, 2 and 3 Viruses, bacteria, fungi, and other microorganisms may cause pneumonia. Viruses account for the majority of pulmonary infections in children younger than 5 years. In children older than 5 years, Mycoplasma pneumoniae (a bacteria-like organism) is the most common agent. Streptococcus pneumoniae is the most common cause of bacterial pneumonia.1,3 Immunocompromised patients are susceptible to a host of opportunistic infections including fungi.4 Neonatal pneumonia is discussed in Chapter 3.
Frontal and lateral chest radiography is routinely performed for suspected infection. Distinguishing between viral and bacterial infection, the latter requiring antibiotics, is the main reason for imaging.2,5 CT is reserved for detecting pulmonary nodules in immunocompromised patients and for characterizing advanced pathology such as cavitation, pulmonary abscess, and empyema.
VIRAL BRONCHIOLITIS
Viral bronchiolitis is also referred to as viral pneumonia, viral lung infection, and viral airways disease. Viral pneumonias constitute the majority of pulmonary infections in infants and young children (less than 5 years). Common viral agents include influenza, respiratory syncytial virus (RSV), parainfluenza, rhinovirus, and adenovirus.1,3 Infection begins in the upper respiratory tract with aerosol inhalation, eventually migrating to the small bronchioles and alveoli. There is resultant small airway obstruction from peribronchial edema and sloughed mucosa and debris.1,2,5 Presenting signs and symptoms include cough, wheezing, tachypnea, and fever.
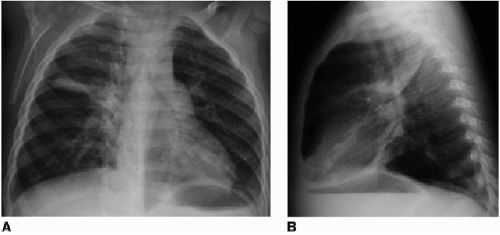
On chest radiographs, viral bronchiolitis presents with bilateral peribronchial or interstitial thickening, perihilar streaky opacities, and pulmonary hyperinflation (Fig. 5.1).1,2,4, 5, 6 and 7 Hyperinflation is often best identified on the lateral projection, with flattening of the diaphragm, anteroposterior expansion of the thorax, and an increased radiolucent retrosternal space. Scattered regions of atelectasis or air trapping are common. Pleural effusions are rare.1
Diagnosing viral bronchiolitis on chest radiographs can be problematic for several reasons. First, peribronchial thickening is among the most subjective interpretations in pediatric radiology. Radiologists will undoubtedly have varying thresholds by which to make this finding. The lateral projection is often helpful for identifying abnormal perihilar opacities. Viral airways disease produces dense or “busy” hila on both projections rather than just the frontal view.5,6 Second, patchy atelectasis in viral lung disease may be misinterpreted as airspace consolidation from bacterial pneumonia.2,7,8 Finally, viral pneumonia is frequently indistinguishable radiographically from reactive airways disease (RAD) or asthma. Asthma often presents similarly with wheezing or cough, but is managed with bronchodilators and corticosteroids.9 Given this overlap both in imaging and symptomatology, peribronchial thickening on pediatric chest radiographs is often interpreted as “viral or reactive airways disease.”
Treatment for viral lung infections is supportive only.6,7 The most common complication of viral pneumonia is a secondary bacterial infection.1 Postinfectious bronchiolitis obliterans (BO) is a rare complication of severe viral pneumonia in young children, most often from adenovirus infections. Peribronchial thickening and hyperlucency are observed on chest radiographs (Fig. 5.2A). High-resolution CT shows a mosaic perfusion pattern, peribronchial thickening, atelectasis, and air trapping (Fig. 5.2B).1,10
BACTERIAL PNEUMONIA
Bacterial infections are usually acquired through inhalation, though hematogenous spread and direct extension from the chest wall are also possible.2,7 Common bacterial agents include S. pneumoniae, Staphylococcus aureus, and Haemophilus influenzae. M. pneumoniae, a bacteria-like organism, accounts for up to 30% of pneumonia in children aged 5 to 15 years.3,7 Historically, Chlamydia was believed to be an important cause for pneumonia in infants, but recently, its role as a causative agent is less clear given its frequency in asymptomatic children.3,11 Presenting symptoms of bacterial infections include fever, productive cough, chest pain, nausea, and emesis. In infants, lethargy, poor feeding, and grunting are observed.
The imaging hallmark of bacterial pneumonia is focal airspace consolidation. Alveoli become filled with exudate, inflammatory cells, and fibrin.1,2 The pattern of airspace opacities is dependent on the causative organism. S. pneumoniae infections are generally confined to one lobe, but rarely involve the entire lobe (Fig. 5.3). Bronchopneumonia is a pattern of patchy multilobar consolidation resulting from peribronchiolar inflammation rather than the alveoli (Fig. 5.4). Staphylococcus typically causes bronchopneumonia, in contrast to the lobar pneumonia observed with S. pneumoniae. Atypical pneumonia is caused by less common infectious organisms, such as Mycoplasma, exhibiting reticular or reticulonodular opacities that resemble viral infections (Fig. 5.5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree