Key Points
- ▪
To appreciate the abnormal patterns of pulmonary vasculature, it is important to be proficient with the details and nuances of normal pulmonary vasculature patterns.
- ▪
The classic patterns of abnormal pulmonary vasculature include cephalization, centralization, collateralization, lateralization, localization, generalized decreased flow, and overcirculation vascularity.
- ▪
There are radiographic signs of large and small pulmonary embolism as well as complications of pulmonary embolism, although final diagnosis resides with, usually, contrast-enhanced computed tomography scanning.
- ▪
Recognition of other right-sided heart disease associated patterns such as those of large and small pulmonary arteries, dilation of the azygous vein, and enlargement of the superior vena cava is clinically useful.
Patterns of Pulmonary Vasculature
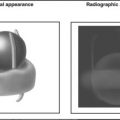
The influence of a cardiac lesion on the pulmonary vasculature is indicative of its hemodynamic consequence. Because the pulmonary vasculature is surrounded by air-filled lung, the pulmonary vessels are well defined. The distal one third of the intrapulmonary vessels are normally not apparent because of their small size. The arteries are normally slightly larger than their accompanying bronchi at any distance into the lung ( Graphic 5-1 ).
Normal Pulmonary Vasculature
The left hilum is normally a couple of centimeters more carinal than the right because the left pulmonary artery is slightly raised by the left mainstem bronchus. Pulmonary arteries to the upper lobes run medial and parallel to the veins. Normally, these veins are fairly well defined. Pulmonary veins from the lower lobes run more horizontally than the pulmonary arteries and enter the hila more inferiorly than the arteries leave the hila. The dependent portions of the lung receive greater flow; hence, in the erect chest radiograph, the lower lobe vessels are greater in size than the upper lobe vessels. In fact, the apical arteries are usually only faintly visualized because in the normal individual, there is little blood flow to the lung apices. The chest radiograph of a normal individual lying flat shows equal vessel size in the lower and upper lobes, because gravitational forces increase the flow and vessel size of the posterior lower and upper lobes. Bronchial vessels are normally not visible.
Abnormal Pulmonary Vasculature Patterns
The following categories are useful, because these radiographic descriptive patterns correspond to different pathophysiologic processes. Increased vessel size is noticeable only when vessels are at least twice normal size.
Cephalization: With pulmonary venous hypertension, pulmonary veins become dilated and more visible throughout the lung fields. However, dilated upper lobe pulmonary arteries are the most apparent feature of pulmonary venous hypertension, because lower lobe vessels are constricted (i.e., narrower than the apical vessels) as a result of local vascular reflexes initiated by raised intravascular pressure (>10–15 mm Hg). To maintain pulmonary perfusion in the face of constricted lower lobe vessels, upper lobe vessels become recruited. Such a pattern strongly suggests elevated pulmonary venous pressure. It is not often seen in left-to-right intracardiac and extracardiac shunts. It is a reliable sign only for erect (nonsupine) radiographs, because, for the reasons mentioned previously, equal vessel sizes to the upper and lower lobes are to be expected in supine radiographs.
Centralization: Increased size of the main pulmonary artery and proximal pulmonary arteries with some reduction of peripheral pulmonary vessels is referred to as centralization. It is found in states of precapillary pulmonary hypertension ( Figs. 5-1 to 5-8 ).

Figure 5-1
There is a borderline increase of the cardiothoracic ratio on the posteroanterior (PA) radiograph and more obvious enlargement of the heart on the lateral chest radiograph. There is some prominence of the right atrial curvature on the PA radiograph and increased apposition of the right ventricle to the sternum consistent with right ventricular enlargement on the lateral chest radiograph. The appearance of the aorta is unremarkable. The main pulmonary artery appears to be enlarged, and the interlobar pulmonary artery is clearly enlarged. In addition, there is reduced peripheral vascularity. No pleural effusions are present. Severe pulmonary hypertension was present due to recurrent thromboembolic disease.
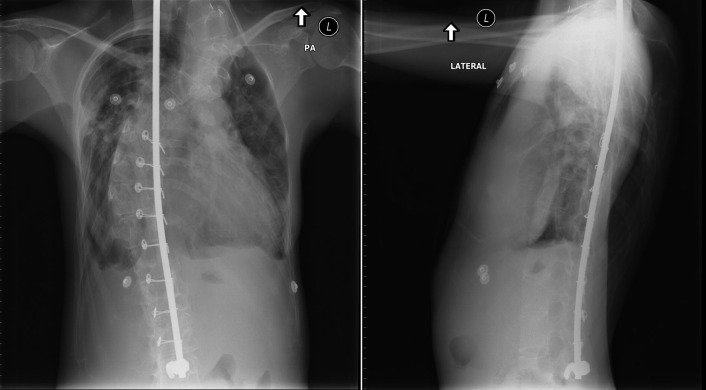
Figure 5-2
Posteroanterior (PA) and lateral chest radiographs. Spinal rods and extreme scoliosis are present. On the PA chest radiograph, cardiomegaly with ambiguous contours are apparent. The lateral chest radiograph shows that anterior postural dimension of the heart of the chest is narrow. The aorta is left-sided, and the main pulmonary artery appears to be enlarged. The remainder of the pulmonary vasculature is difficult to evaluate. There were systemic levels of pulmonary hypertension from restrictive chest disease due to childhood treatment of a neuroblastoma. There is marked enlargement of the right heart confirmed by echocardiography.
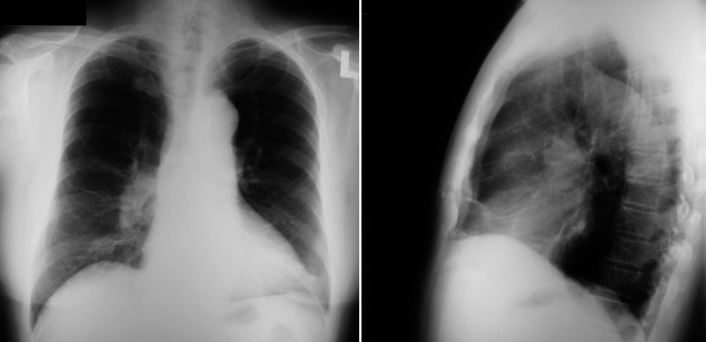
Figure 5-3
Posteroanterior (PA) and lateral chest radiographs. On the PA chest radiograph, there is no definite cardiomegaly or abnormal contours to the heart. The aorta is left-sided, and its appearance is normal. The main pulmonary artery is difficult to scrutinize, but the interlobar pulmonary artery is clearly enlarged and there is reduced peripheral pulmonary vasculature. On the lateral chest radiograph, the relation of the right ventricle to the sternum is ambiguous. There are systemic levels of pulmonary hypertension due to primary pulmonary hypertension in this adult male. There was considerable enlargement of the right heart on echocardiography, although this is not apparent on the chest radiograph.
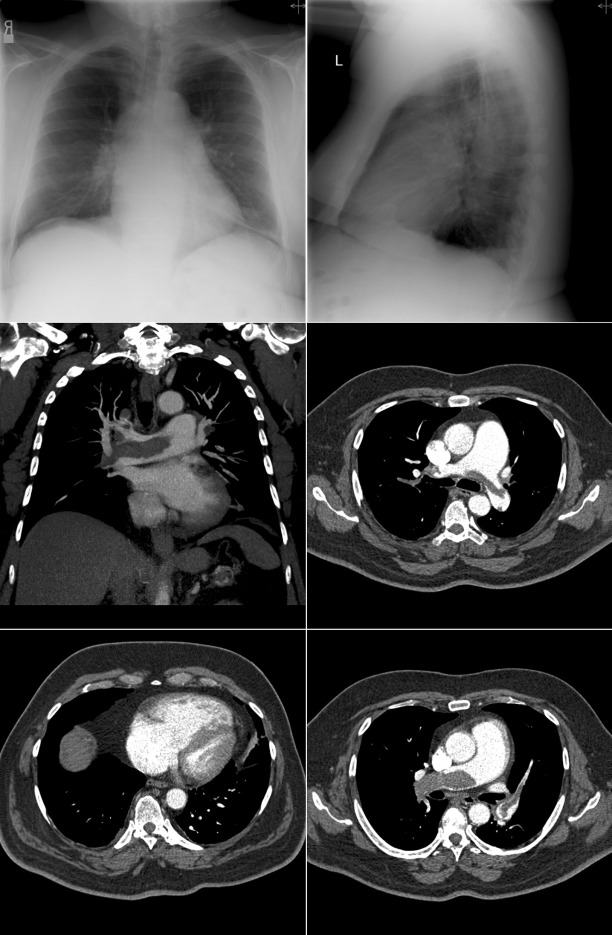
Figure 5-4
Chest radiographs and contrast-enhanced computed tomography (CT) scans of a patient with recurrent thromboembolism and terminal right-sided heart failure. Note the size of the main and central pulmonary arteries and of the right heart chambers on both the chest radiographs and the CT scans.
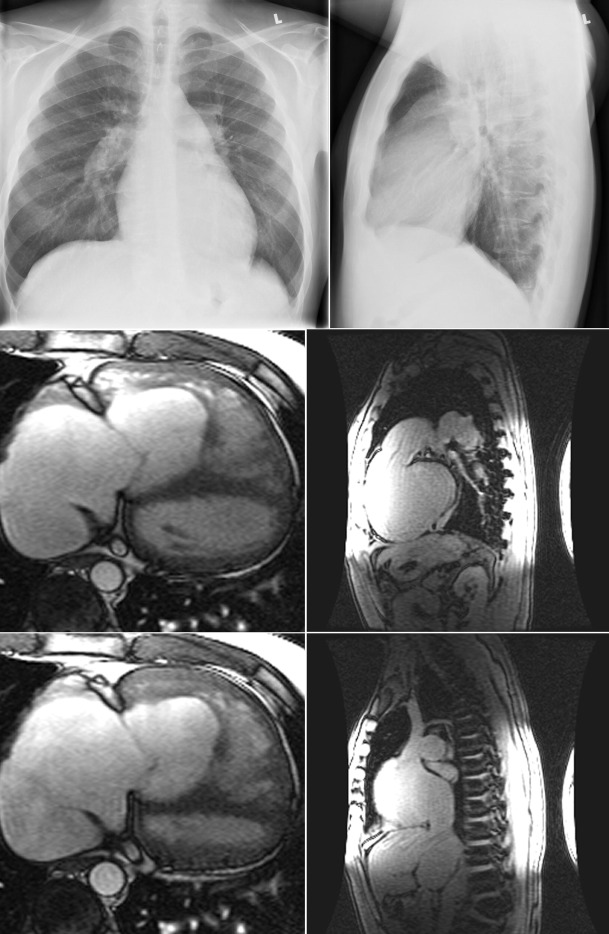
Figure 5-5
Chest radiographs and cardiac magnetic resonance (CMR) images of a patient with advanced primary pulmonary hypertension. On the radiographs, the main and central pulmonary arteries are dilated, the right ventricle is prominent, and the azygous vein may be dilated. There is rapid tapering of the pulmonary arteries (“centralization”) and paucity of peripheral vessels, including veins. The CMR steady-state free precession images demonstrate the extent of right-sided chamber, main pulmonary artery, and caval and azygous vein enlargement.
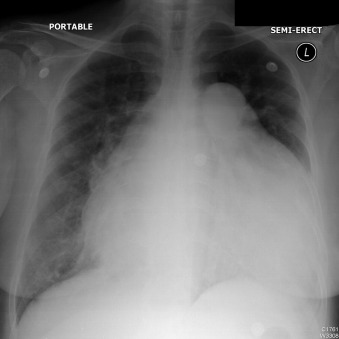
Figure 5-6
The cardiothoracic ratio is markedly increased, as is the dimension of the main pulmonary artery. There is terminal right-sided heart failure from primary pulmonary hypertension.
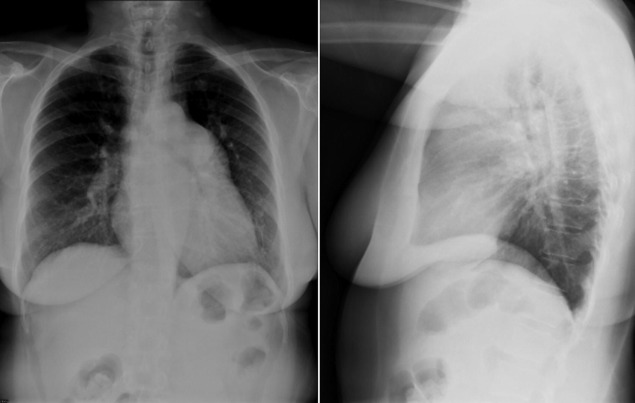
Figure 5-7
Severe pulmonary hypertension. Note the markedly enlarged main, left, and central pulmonary arteries, which are “pruned.” As is seen on the lateral radiograph, the right ventricle is enlarged.
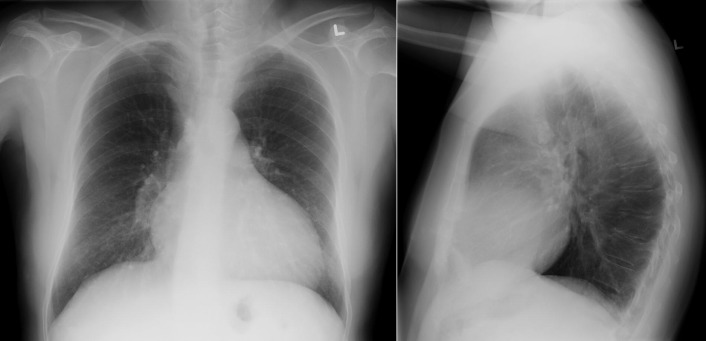
Figure 5-8
Posteroanterior (PA) and lateral radiographs in an adult male with systemic levels of pulmonary hypertension due to primary pulmonary hypertension. There is an increase of the cardiothoracic ratio, with some prominence of the right atrial curvature on the PA radiograph. There is increased apposition of the right ventricle to the sternum on the lateral chest radiograph. Some kyphosis is present. The main pulmonary artery is slightly enlarged, and the interlobar pulmonary artery is clearly enlarged.
Collateralization: This is suggested by oligemia of the lung fields, with evidence of
- □
Bronchial collateralization (vessels seen in the upper and medial lung zones near their origin from the descending aorta)
- □
Intercostal collateralization (indicated by rib notching) (see Chapter 6 )
Lateralization of flow : This is suggested by segmental oligemia and segmental preserved flow. This may be seen in the clinical setting of a pulmonary embolus (Westermark sign), or pulmonary artery anomalies ( Fig. 5-9 ).

Figure 5-9
Congenital absence of the right pulmonary artery.
Localization of pulmonary vasculature : This usually indicates a pulmonary arteriovenous malformation ( Figs. 5-10 to 5-12 ).
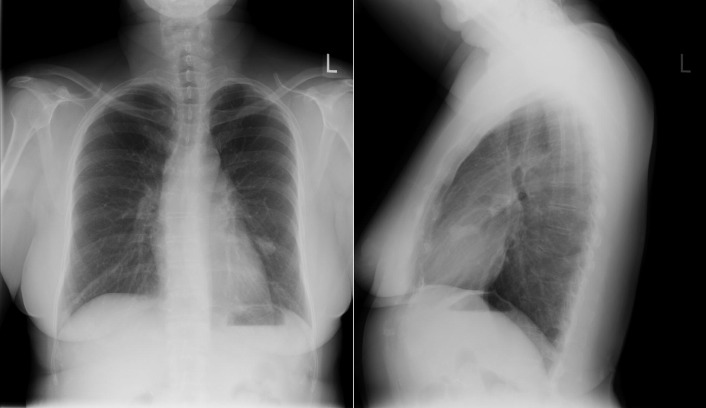
Figure 5-10
Posteroanterior (PA) and lateral chest radiographs of a patient with bilateral pulmonary arteriovenous malformations (AVMs). The appearance of AVM on the left side is rounded and nodular and projects just over the left heart border on the PA film. The appearance of AVM on the right side is more classic, with a prominent feeder pulmonary artery and draining pulmonary vein extending to and away from it.
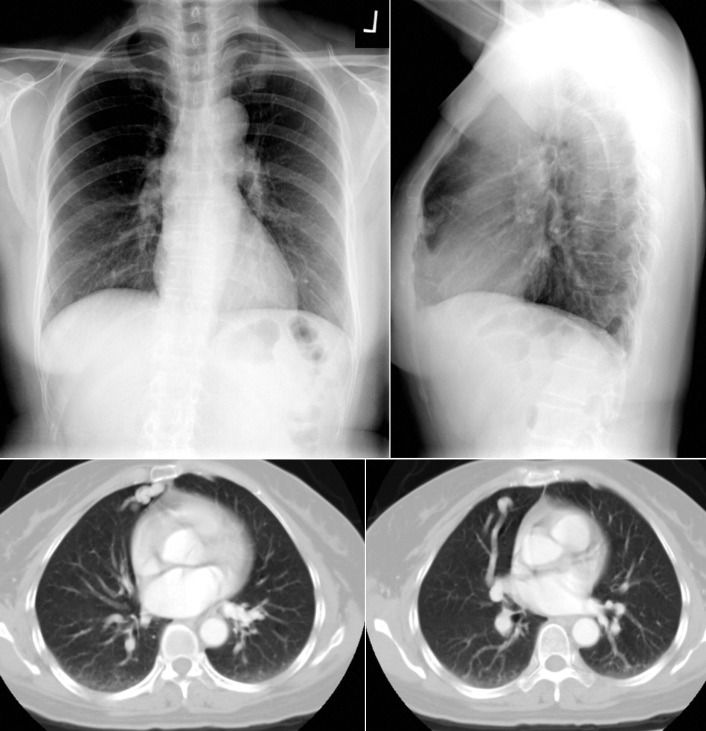
Figure 5-11
On the frontal radiograph, a pair of worm-sized feeder and drainage vessels to an arteriovenous malformation in the lingua is seen. Contrast-enhanced axial computed tomography images depict it well.
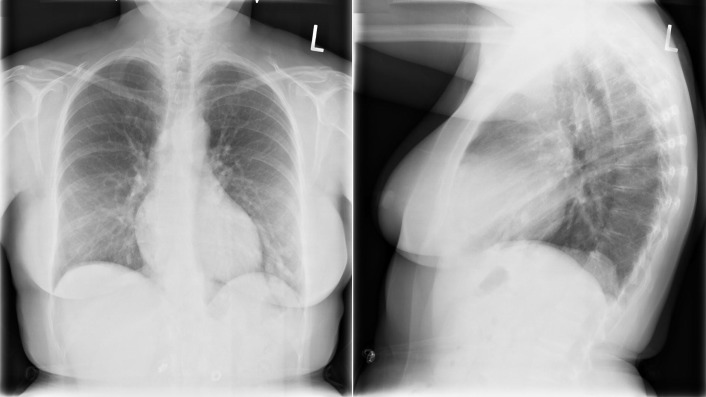
Figure 5-12
Bilateral pulmonary arteriovenous malformations (AVMs) of the lower lobes. The AVM in the left lower lobe is obvious, as are the feeder and drainage vessels.
Generalized decreased flow: This occurs with severe congenital right-sided obstructive lesions or advanced pulmonary vascular disease. Reduced blood flow is suggested by abnormal lung lucency and small vessel size.
Overcirculation vascularity: This refers to uniform increase in prominence of central and intrapulmonary vessels. The pattern may be symmetric or asymmetric (asymmetry may be because of a congenital cause or a surgical corrective procedure). Causes of overcirculation vascularity include
- □
Left-to-right shunting
- •
Intracardiac (e.g., atrial septal defect, ventral septal defect)
- •
Extracardiac (e.g., patent ductus arteriosus, truncus, transposition, anomalous pulmonary venous return, surgical shunts, other)
- •
- □
High flow states (e.g., hyperthyroidism, pregnancy, anemia)
Obviously, plethoric pulmonary vasculature is always due to a shunt of greater than 2:1 pulmonary-to-systemic flow ratio (Qp:Qs). A less obvious appearance may be from any hyperdynamic state.
Pulmonary Artery Sizing
The most frequent visible branch of the pulmonary arteries is the right descending pulmonary artery. This component of the pulmonary arterial system is the most visible because it is surrounded by air-filled lung and lies free of other radiopaque structures in the heart. It is usually well visualized near the right hilum, lateral and parallel to the lower lobe bronchus and is measured there.
Interlobar Pulmonary Artery
An increase in the pulmonary artery size is seen in states of increased pressure, increased flow, or turbulent flow (i.e., poststenotic dilatation, pulmonary hypertension, atrial septal defect). Normally, the diameters of the bronchi and pulmonary arteries are roughly comparable at any distance into the lung. The interlobar (right) pulmonary artery is typically silhouetted on its medial and lateral aspects on the frontal radiography and can be measured:
- □
Normal: 9–14 mm
- □
Abnormal: ≥17 mm (male or female) (<14 mm is unlikely to have significantly increased flow)
- □
Upper limit normal (males): 15 mm
- □
Upper limit normal (females): 16 mm
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree