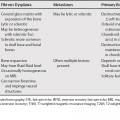
59 Radiologic manifestations are usually confined to the lung tissue within the radiation port and are dependent on the interval after completion of treatment. The radiological changes are expected 8 weeks after 4000 rad, and 1 week earlier for each 1000 rad increments above 4000. In the acute phase (2 to 6 weeks), radiation injury typically manifests as ground-glass opacity or as consolidation; in the late phase, it typically manifests as traction bronchiectasis, volume loss, and scarring. However, the use of oblique beam angles and newer irradiation techniques such as three-dimensional conformal radiation therapy or hypofractionated stereotactic radiotherapy can result in an unusual distribution of these findings. Awareness of the typical and atypical manifestations of radiation-induced lung disease can be useful in differentiating from infection, recurrent malignancy, lymphangitic carcinomatosis, and radiation-induced tumors. Findings such as the late appearance or enlargement of a pleural effusion, development of consolidation, opacification of a previously demonstrated air bronchogram, a mass, or cavitation suggest recurrence of malignancy and/or infection. Because radiation pneumonitis can have increased fluorodeoxyglucose (FDG) uptake that mimics recurrent disease, fluorodeoxyglucose positron emission tomography (FDG PET) is best performed at least 3 months after completion of radiation therapy or before lung radiation-induced lung injury. FDG PET has, however, high negative predictive value, and focal opacities with low FDG uptake can be followed radiographically. Approximately 10% of patients receiving lung radiation will develop clinical disease usually 2 to 6 months after the initiation of therapy. Radiographic changes following radiation therapy can be seen in up to 42% of patients. Drug toxicity can be synergistic and may occur even if the drugs and radiotherapy are separated in time, as many as 10% of patients receiving chemotherapeutic agents will develop an adverse drug reaction in their lungs. The most common drugs resulting in lung toxicity are bleomycin, methotrexate, carmustine, busulfan, and cyclophosphamide. The high-resolution computed tomography (CT) findings of drug-induced lung disease reflect the histologic findings (Table 59.1).
Radiation and Drug-Induced Lung Disease
Radiation-Induced Lung Disease
Drug-Induced Lung Disease