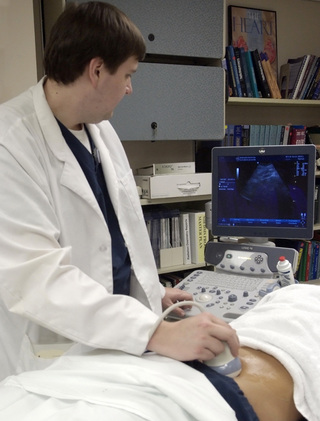
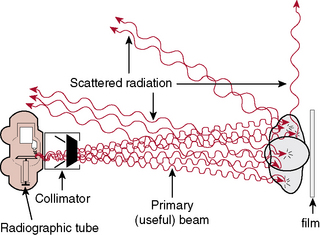
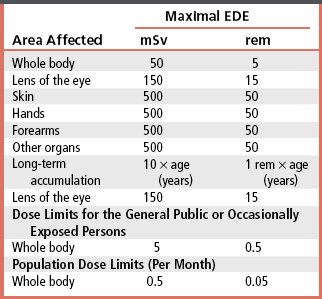
CHAPTER 18 On completion of this chapter, you should be able to: • Explain the need for radiation protection efforts by operators of radiation-producing equipment. • List sources of radiation and explain their significance in dose accumulation. • Define radiation units of measurement such as roentgen, rad, rem, and curie. • Describe the role of the National Council on Radiation Protection and Measurements. • Explain what is meant by as low as reasonably achievable (ALARA) for radiation workers and nonradiation workers. • List and explain the three types of radiation/matter interactions that are significant in radiology. • List and explain the four possible results that may occur when photons of radiation strike cells. • List and explain the significance of radiation effects on the total body. • List and describe the practical radiation protection methods expected of all radiologic technologists on each radiographic test. • List and describe instruments for monitoring personnel exposure to radiation. Units of measurement are known as the roentgen (written as R in calculations), the rad, the roentgen-equivalent-man (rem), and the curie (Ci); the quantities associated with these units are exposure, absorbed dose, dose equivalent, and activity, respectively. The roentgen is a unit of exposure for x-rays and gamma rays. The rad is a unit of absorbed dose of any type of radiation. The rem is a unit that measures the biologic effect of x, alpha, beta, and gamma radiation on humans. The International System of Units (SI) uses coulomb*/kilogram (C/kg) in place of roentgen, gray (Gy) instead of rad, and sievert (Sv) rather than rem. For radiation protection from x and gamma radiation, 1 roentgen (C/kg) approximately equals 1 rad (Gy) or 1 rem (Sv). The Ci measures the amount of activity (known as radioactive disintegrations) that a radionuclide gives off. The unit of activity in the SI system is Becquerel (Bq); this measure is used in nuclear medicine studies with radionuclides, which are sometimes erroneously called radioactive isotopes (Table 18-1). TABLE 18-1 rad, Radiation absorbed dose; rem, roentgen-equivalent-man; Si, International System of Units. Students who are younger than 18 years and who are exposed to radiation during educational activities should receive no more than a 0.1-rem whole-body dose in 1 year. This EDE limit is based on the laws regarding minors. Thus this limit is the same for students younger than 18 years as it is for the general public. Minors employed in radiation areas are also included in these guidelines. After the age of 18, the student or employee is classified as an occupational worker (Table 18-2). TABLE 18-2 Maximal EDE for Occupational Exposure (Annual)* EDE, Effective dose equivalent. *The 1987 edition of NCRP Report No 91 recommends the discontinuance of the MPD formula; it suggests as guidance for protection that the cumulative exposure should not exceed the age of the individual in years × 10 mSv (years × 1 rem). The total permissible dose to a pregnant woman should be no more than 0.5 rem because of the susceptibility of the developing embryo or fetus to the harmful effects of radiation. Authorities further suggest that the rate of exposure be controlled by specifying that the dose equivalent should not exceed 0.5 mSv (0.05 rem) in any given month. In fact, postponing any radiation exposure is advisable during the entire gestation period or to use another imaging modality, such as ultrasonography, to gather information for diagnosis (Fig. 18-1). An atom is the smallest part of an element and is made up of a nucleus surrounded by electrons. X-rays are packets of energy called photons, which have the ability to knock electrons out of their orbit; this action creates electrically charged ions. When x-rays pass through matter, this process of ionization results in a transfer of energy. The x-ray photons can be absorbed or scattered by the medium with which the photons interact or pass directly through the medium without any interaction taking place (Fig. 18-2).
Radiation Safety and Protective Measures
Need for radiation protection
Radiation Measurements
Quantity
Traditional Unit
SI Unit
Name
Symbol
Name
Symbol
Exposure
roentgen
R
coulomb per kilogram
C/kg
Absorbed dose
rad
rad
gray
Gy
Dose equivalent
rem
rem
sievert
Sv
Activity
curie
C
Becquerel
Bq
A
B
C
R
2.58 × 10-4
C/kg
rad
0.01
Gy
rem
0.01
Sv
Ci
3.7 × 1010
Bq
National Council on Radiation Protection and Measurements
Effective Absorbed Dose Equivalent Limits
Interaction of x-rays with matter
Radiation Safety and Protective Measures