This article discusses the typical findings seen on conventional radiography in 3 common shoulder pathologies, namely glenohumeral instability, rotator cuff pathology, and acromioclavicular joint dislocation. Correlative MR images are used to explain and illustrate the significance of radiographic findings that suggest the presence of underlying shoulder pathology.
Key points
- •
Conventional radiograph is the first modality of imaging used in the evaluation of shoulder pain, allowing diagnosis of acute traumatic injuries and suggesting soft tissue pathology, especially in the setting of advanced disease.
- •
MR imaging plays an important role in the assessment of the shoulder, with high accuracy for both the osseous and soft tissue structures but can only be obtained in selected cases related to availability and cost considerations.
- •
Correlation with MR imaging allows the radiologist to improve his/her understanding of findings on conventional radiography and recognize signs indicating significant pathology, helping to guide further imaging and management.
Introduction
Shoulder pain is a common cause of pain and disability and can be due to a range of pathologies, most commonly related to trauma or degeneration. The initial evaluation of the symptomatic shoulder consists of clinical examination, followed by conventional radiography. Conventional radiography, although limited in its visualization of the soft tissues about the shoulder, affords excellent spatial resolution and accurate assessment of osseous abnormalities. Advanced imaging, including ultrasound, computed tomography (CT), and MR imaging, is used for more accurate delineation of anatomy and pathology in selected cases. Increasing use of these modalities has resulted in less emphasis on teaching and understanding how lesions appear on conventional radiographs. In this article, the authors use MR imaging to illustrate the basis of the typical appearances on radiography of common lesions associated with glenohumeral instability, rotator cuff pathology, and acromioclavicular (AC) joint injury.
Glenohumeral instability
The glenohumeral joint (GHJ) is the most mobile joint in the human body, and the relatively small contact area between its glenoid and humeral articular surfaces and mismatch in their arcs of curvature results in inherent instability. At the midrange of shoulder motion, the concave articular surface of the glenoid and the labrum function as static stabilizers maintaining articular congruity. As movement progresses, the capsulolabral structures become the primary restraints, with the rotator cuff musculature contributing as a dynamic stabilizer of shoulder stability. Instability of the GHJ occurs as a result from failure of these coordinated stabilizers, leading to displacement and abnormal contact between its articular surfaces.
Anterior Instability
The most common direction of GHJ dislocation is anterior, in which the humerus displaces anteroinferiorly to lie below the coracoid process or glenoid rim. Anterior dislocation is frequently associated with an impaction fracture at the posterosuperior humeral head (Hill-Sachs lesion) and/or a shearing fracture of the anteroinferior glenoid (Bankart lesion). Radiography is the initial modality used to detect, localize, and quantify displacement and these characteristic fractures. The standard anteroposterior (AP) view obtained in external rotation readily detects humeral displacement but is not tangential to the posterior humerus or GHJ, leading to suboptimal evaluation of fractures.
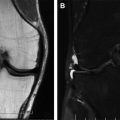
The Hill-Sachs lesion seems as a region of articular surface flattening at the posterior superior humeral head. An AP view in internal rotation is necessary to profile this region ( Fig. 1 ). The defect varies in size, location, and orientation depending on the position of the arm and force applied during dislocation. Variations in its appearance range from deep angular defects to a paradoxic “osteophyte-like” protuberance when the radiograph is tangent to the raised edge of the lesion relative to the affected segment. The Hill-Sachs lesion should be distinguished from normal physiologic flattening at the posterior head-neck junction of the humerus. The Hill-Sachs lesion is located at the uppermost portion of the humeral head, whereas the physiologic depression lies further distally, typically 20 mm or more below the top of the humeral head. In the axial plane, the Hill-Sachs lesion is generally located farther laterally than the anatomic indentation. Pseudocysts at the bare area of the humeral head, marginal erosions in inflammatory arthropathies, and irregularity secondary to enthesopathy can also simulate a Hill-Sachs lesion.

The Bankart lesion is less common and can be challenging to visualize on radiography, particularly when small. It appears as a disruption of the inferior half of the anterior glenoid rim, with an elongated bone fragment typically displaced medially and inferiorly. The Grashey view (AP view obtained obliquely along the plane of glenoid anteversion) is more sensitive ( Fig. 2 ). The standard axillary projection is not sensitive, as the fracture is typically limited to the inferior glenoid below the profiled articular surface. The apical oblique projection (AP with 45° caudal angulation in internal rotation) is sensitive, although it and other specialized projections such as the West Point, Velpeau, and Bernageau views are less commonly used with the advent of cross-sectional imaging. Soft tissue injuries associated with anterior dislocation such as tearing of the glenoid labrum and disruption of the glenohumeral capsule and supporting ligaments are best assessed with MR imaging ( Fig. 3 ).


Posterior Instability
The primary restraints to posterior instability are the posterior capsule, posterior band of the inferior glenohumeral ligament, posterior labrum, and subscapularis. Posterior glenohumeral instability is less common than the anterior form, accounting for only 2% to 4% of all shoulder dislocations; it may be bilateral when related to seizure or electric shock. The humeral head is displaced posteriorly in internal rotation, producing impaction fractures at the contact zones at the anterior humeral head (reverse Hill-Sachs lesion) and posterior glenoid rim (reverse Bankart fracture). Avulsion fracture of the lesser humeral tuberosity and other fractures at the shoulder girdle may also be present.
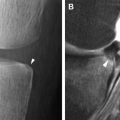
Posterior shoulder dislocation can be challenging to identify on AP radiographs, with greater than 50% missed at initial examination. Findings on AP radiographs include the “lightbulb sign” (fixed internal rotation of the humerus), “rim sign” (widening of the GHJ), absence of normal overlap of the humeral head and glenoid, and the “trough sign” (double contour of the medial humeral head, representing the normal cortex and the long axis of a reverse Hill-Sachs fracture). When a posterior dislocation is suspected, a lateral scapula (“Y view”) or axillary view should be obtained. The injury is most evident on the axillary projection, which also profiles the trough and reverse Bankart fractures better ( Fig. 4 ).

Frank posterior dislocation is less common than recurrent posterior subluxation. Chronic posterior instability may be related to repetitive trauma in competitive athletes or related to atraumatic factors such as soft tissue laxity and glenoid retroversion, hypoplasia, and dysplasia. In repetitive trauma, as seen in overhead throwing sports, a Bennett lesion (“thrower’s exostosis”) may be seen as an extraarticular curvilinear bony spur along the posteroinferior glenoid rim related to traction at the posterior band of the glenohumeral ligament. The Bennett lesion itself is asymptomatic but is commonly associated with posterior labral and posterior undersurface rotator cuff tear.
Advanced Imaging
Advanced imaging techniques play a critical role in the assessment of shoulder instability. CT is most useful for identifying and characterizing bone injuries, whereas MR imaging excels at identifying labral and soft tissue injury. Evaluation of the orientation of the fractures and the extent of humeral, glenoid, and combined (bipolar) bone loss is important for planning surgical repair to avoid recurrent shoulder instability ( Fig. 5 ). Hill-Sachs fractures parallel to the anterior glenoid rim in abduction allow the humerus to engage the glenoid lip and redislocate. Larger Hill-Sachs and Bankart defects require soft tissue augmentation or bone grafting to reestablish stability. The on-track off-track method uses 3-dimensional CT scanning to assess fracture size and orientation. It applies the glenoid track definition, defined as the contact area between the humeral head and glenoid during shoulder abduction and external rotation. It postulates that the risk of instability and engagement between the humeral defect and glenoid rim and redislocation is increased when the Hill-Sachs lesion approaches the medial margin of the residual glenoid. Inadequate reconstruction in such cases leads to persistent instability and a high incidence of redislocation.

Rotator cuff
Rotator cuff pathology, a common cause of shoulder pain and dysfunction, may present acutely, typically caused by trauma or crystal-induced inflammation, or more commonly, resulting in chronic symptoms related to degeneration of the rotator cuff tissues causing loss of rotator cuff structure and function. Several radiographic findings can be used to diagnose rotator cuff pathology, supported by advanced imaging to confirm the diagnosis, delineate cuff morphology, identify associated abnormalities, and plan appropriate treatment.
Acute Pathology
Trauma resulting in an acute tear of the rotator cuff is uncommon, representing a small minority of tears encountered in routine clinical practice. Standard shoulder radiographs are typically normal in such patients unless there is an associated fracture. In the setting on an acute massive tear of the supraspinatus tendon, the active abduction view of the shoulder obtained with the shoulder at 90° from the horizontal plane may demonstrate decreased acromiohumeral distance (≤ 2 mm), but only if there is significant medial retraction of the torn tendon. Unfortunately, most of the acute tears do not immediately retract, so initial radiographs are insensitive.
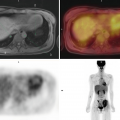
Acute rotator cuff symptomatology is more commonly related to hydroxyapatite deposition disease (HADD), with symptoms related to crystal extrusion from the tendon into the peritendinous tissues, subacromial bursa, or less frequently, into the bone or muscle, producing acute inflammation. The shoulder is well recognized as the most common site of symptomatic HADD. The imaging appearance depends on the phase of the disease, which varies from a dense ovoid homogeneous sharply marginated intratendinous calcification in the inactive phase to an irregular ill-defined amorphous calcification extending beyond the tendon footprint when active. AP radiographs with the shoulder in internal and external rotation allow identification and localization of calcific deposits. Supraspinatus tendon calcifications are seen adjacent to the greater tuberosity in external rotation, whereas infraspinatus and teres minor calcifications are seen adjacent to the lateral edge of the greater tuberosity in internal rotation. On MR imaging, calcific deposits appear as rounded areas of low signal intensity on all imaging sequences. Findings in the inflammatory phase include surrounding inflammation, bursal fluid and bone edema, mimicking infection, trauma, or neoplasm ( Fig. 6 ).

Degenerative Pathology
Degenerative rotator cuff disease is more common and its incidence increases with age, resulting in tendinosis and ultimately tearing. The cause of cuff degeneration is multifactorial, caused by factors that include aging, repetitive microtrauma, hypovascularity, laxity, and impingement. Clinical examination shows high sensitivity (90%) and specificity (54%) for full-thickness tears but has low accuracy for partial tears. Similarly, radiographs show higher accuracy in large chronic complete tears than in early degeneration, when changes dominate at the entheseal attachment of the tendons at the tuberosities. Entheseal changes at the tendon insertion include osteopenia, bony sclerosis, surface irregularity, and cyst formation.
The significance of cystic changes at the tuberosities depends on their precise position. These form as the tendon tearing at the footprint disrupts the normal barrier to synovial fluid intrusion, followed by further ingrowth of synovial and granulation tissue. In partial-thickness tears, such cysts are more common with those that are articular-sided rather than bursal-sided. Cysts occur in 2 distinct locations that differ in their pathogenesis and clinical significance. Cysts located anteriorly at the supraspinatus and subscapularis insertions are closely related to rotator cuff disorders, with a 94% positive predictive value ( Fig. 7 ). Conversely, posterior humeral cysts at the infraspinatus insertion and in the bare area of the anatomic neck have little correlation with cuff disease and are typically related to vascular intrusions and asymptomatic. Cystic changes in the greater and lesser tuberosity appear as focal round lucencies with sharply defined margins, usually isolated on each location; these are typically 3 to 4 mm in diameter and uncommonly exceed 1 cm. Supraspinatus cysts are located at the upper anterior greater tuberosity and best seen in external rotation, whereas the less significant infraspinatus cysts are situated lower at the posterior tuberosity and anatomic neck and are profiled in internal rotation. CT and MR imaging are more accurate in identifying and localizing these and other entheseal changes at the tendon attachment sites.