11
Radiologic Gastrostomy and Gastrojejunostomy
Provision of adequate nutritional support is a challenging problem in managing patients who are unable to take food orally. For these patients, nutrition may be provided either enterally or by means of total parenteral nutrition. Total parenteral nutritional support is a labor-intensive, expensive technique that is fraught with problems such as recurrent sepsis and maintenance of adequate central venous access. Provision of adequate trace elements and essential amino acids is more difficult with total parenteral nutrition, as a result of its nonphysiological nature, than with enteral nutrition.
For patients who have a functioning gastrointestinal tract, enteral nutrition is the method of choice. Feeding in these patients can be accomplished by placement of a nasogastric tube, which is usually adequate for short-term nutritional support; however, for long-term feeding, the method of choice is placement of a gastrostomy or gastrojejunostomy tube.
Placement of a gastrostomy tube can be done by surgical, endoscopic, or percutaneous radiological methods. Surgical gastrostomy was first performed by Vernueil in France in 1876, and it remained the sole method for gastrostomy tube placement until 1979. The complication rate of surgical gastrostomy is acceptably low but increases sharply in patients who are in poor physical condition, as many patients requiring gastrostomy tube placement tend to be. In a study of 147 patients who underwent surgical placement of a gastrostomy tube, 15.7% had complications, of which half were major complications such as hemorrhage, wound breakdown, or stoma leak.1 Overall 30-day mortality was 6.1%, most of which was related to respiratory complications. In a recent metanalysis of the literature on gastrostomy placement, the 30-day mortality rate as well as both the major and minor complication rates for surgical placement of a gastrostomy tube were statistically significantly higher than for either endoscopic or radiologic methods of placement.2 Gastrostomy placement was associated with a much higher cost than the endoscopic or percutaneous radiologic methods. For these reasons, there is now an increasing emphasis on nonsurgical placement of gastrostomy tubes.
Endoscopic gastrostomy was introduced by Gauderer and Ponsky in 1980as an alternative to the surgical gastrostomy procedure.3 Essentially, the original technique and the subsequent modifications involve introduction of an endoscope into the stomach and transillumination of the anterior abdominal wall. The abdominal wall then is pierced from the exterior over the region of transillumination, and a guidewire is passed out through the incision. The percutaneous endoscopic gastrostomy (PEG) tube is then passed over the wire into the stomach. A variety of fixation techniques have been developed. Endoscopic placement affords the potential advantages of detection of coexisting lesions in the esophagus or stomach.Wollman’s study reported that additional abnormal findings were detected in 26% of patients who underwent endoscopic gastrostomy placement.2 The endoscopic method is unsuitable for patients requiring gastric decompression for chronic bowel obstruction, in which case the fluoroscopic method offers a more facile placement of primary gastrostomy catheter.
In 1983, several radiology groups, working independently, described a percutaneous method for primary gastrostomy tube placement using a Seldinger technique.4,5 Since the original technique was described, several technical advances and modifications have been made, and considerable clinical experience has been gained. Presently, fluoroscopic placement of gastrostomy tubes is a well-recognized, clinically important technique. In many institutions, it has become the method of choice for placement of gastrostomy feeding tubes as a result of its low complication rate and low cost compared with other available methods.
 Indications for Gastrostomy Tube Placement
Indications for Gastrostomy Tube Placement
The most common indication for gastrostomy tube placement is to provide nutritional support for patients with dysphagia. For most patients, the dysphagia is a result of a debilitating neurological disorder, such as cerebrovascular accident, trauma, dysmyelinating and demyelinating disease, or postsurgical sequelae, such as a neurological deficit following resection of an intracranial neoplasm. A second important group of patients are those with swallowing disorders secondary to oropharyngeal or esophageal tumors. An infrequent but important indication is small bowel disease, such as Crohn’s disease, short bowel syndrome, or radiation enteropathy. Because patients with small bowel disease cannot tolerate a normal diet, nutrition must be presented in a form that can be absorbed, which is achieved by providing an elemental diet through a gastrostomy or gastrojejunostomy tube.
Other less common indications for gastrostomy tube placement include decompression of the upper gastrointestinal tract in a patient with advanced malignant obstruction, chronic adynamic gastroparesis, or ileus, and anorexia with underlying psychiatric or malignant illness. Percutaneous gastrostomy also has been used for the removal of intragastric foreign bodies, such as displaced esophageal stents, and for transgastric drainage of pancreatic pseudocyst fluid collections.
 Contraindications to Percutaneous Gastrostomy
Contraindications to Percutaneous Gastrostomy
Relative contraindications for radiologic gastrostomy tube placement include portal hypertension with gastric varices, severe gastritis, and massive ascites, which can increase the tendency for leakage of gastric contents from the stomach after tube placement. Many radiologists consider large ascites to be an absolute contraindication; however, this is not the case in our practice. We perform decompression gastrostomy in patients with chronic bowel obstruction and ascites, most commonly secondary to intraperitoneal metastatic spread of ovarian carcinoma. For these patients, we perform preprocedural paracentesis, and we routinely use the radiologic T-fastener gastropexy to reduce the incidence of intraperitoneal leakage of gastric contents. We also perform serial paracentesis after gastrostomy tube placement to prevent massive ascites buildup, which can cause necrosis of the gastropexy.
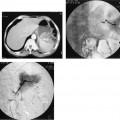
Percutaneous placement of a gastrostomy tube requires a safe percutaneous access to the stomach. Occasionally, a patient’s stomach is overlaid by transverse colon or the left lobe of the liver. The stomach may have a high subcostal position in some patients as an anatomic variant or in patients who have had a previous partial gastrectomy. These problems are usually surmountable by performing the initial gastric puncture under computed tomography (CT) guidance, after which the patient is transferred to the interventional fluoroscopy suite for track dilation and tube placement.
Encasement of the stomach by tumor is also a relative contraindication for several reasons. One reason is that healing does not occur normally, and a fistulous track therefore does not readily form between the stomach and the skin. A second reason is that tumor tissue is abnormally vascularized by neovessels that have an increased propensity to bleed if they are transgressed. Lack of distensibility of a tumor-encased stomach also may make tube placement extremely difficult. The symptoms of anorexia and nausea that patients with tumor encasement of the stomach experience often remain unrelieved by gastrostomy tube placement because the symptoms are due largely to effects of the tumor on the autonomic nervous system.
Gastrostomy tube placement is relatively contraindicated in patients who are taking long-term corticosteriod treatment because they may have a higher complication rate of gastric perforation as a result of stomach wall atrophy and poor healing, leading to increased risk for gastric perforation and leakage of gastric contents. Patients with active or chronic duodenal ulcers should have a gastrostomy tube placed rather than undergo a transgastric jejunostomy or gastrojejunostomy tube because the mechanical irritation from a tube passing through the duodenal bulb may cause serious bleeding.
In some patients, the presence of a tube through the pylorus can cause a partial or complete gastric outlet obstruction syndrome, which may be overcome by placement of either a single gastrojejunostomy tube, which incorporates both a draining gastrostomy port and a feeding jejunal port, or by a two-tube technique, in which both a gastrostomy and a transgastric jejunostomy are placed through separate tracks. Our experience leads us to favor the two-tube approach because better gastric drainage may be achieved by using this approach. To achieve optimum gastric drainage, the drainage tube should be situated at the most dependent portion of the stomach, which in most patients requiring gastrostomy is the fundus because of the patient’s supine position. The two-tube approach allows a tube to be placed directly in the fundus, whereas the use of a single gastrojejunostomy catheter allows only for the gastrostomy drainage port to be placed in the antrum, resulting in suboptimal drainage. The two-tube approach also allows a large 14 Fr catheter to be used for drainage and a separate 14 Fr tube to be used for jejunal feeding. We routinely use gastrostomy tubes that are 30 cm working length and transgastric jejunostomy tubes that are 53 cm working length.
 Preprocedural Assessment and Preparation
Preprocedural Assessment and Preparation
Informed written consent is necessary before the procedure is performed. Because many patients who require a gastrostomy tube cannot give consent themselves, consent should be obtained in advance from the next of kin. Preprocedural blood workup, such as prothrombin time, partial thromboplastin time, and platelet count, although not routinely performed on every patient, should be requested for patients in whom a coagulopathy may preexist, such as patients who have been treated with anticoagulants or who are malnourished. The patient’s medical records are reviewed with particular attention to previous gastric surgery or medical conditions that preclude the use of hypotonic agents, sedation, or narcotics. Patients with a coagulopathy should receive treatment to correct clotting parameters before the procedure is done.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree