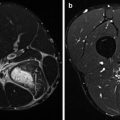
Fig. 2.1
MRI of avascular necrosis of the lunate. Child, 13 years old, with centrally located chronic pain at the dorsal aspect of the wrist. High-level tennis player. No obvious acute trauma. (a) Coronal SE T1-WI prior to intravenous gadolinium injection, (b) coronal TSE intermediate TE WI, (c) Coronal digital subtraction image of T1-WI after and before intravenous gadolinium administration. Normal fat signal on T1-WI (a), homogeneous suppression of signal on water-sensitive intermediate TE series, and absence of bone marrow edema at all the carpal bones (b). Normal shape of the carpal bones and absence of gadolinium enhancement at the entire lunate (c). This case demonstrates the importance of IV gadolinium administration in diagnosis of AVN to prove the lack of vascular perfusion in the absence of other signs of AVN as there are crescent line, demarcation line, and collapse
2.2.2 Ultrasound
Major advantages of US are its high spatial resolution for superficial structures, low cost, availability at short notice, ease of examination, short examination times, and lack of radiation exposure. Since approximately 30 % of sports injuries deal with muscle and tendon injuries, ultrasound (US) plays a major role in sports traumatology, helping the clinician to decide whether the athlete should or should not return to training and competition (Peterson and Renstrom 1986). Due to the excellence of spatial resolution and definition of muscle structure, US keeps its leading edge when dealing with muscle strain and contusion, both in the initial phase for recognition of a lesion, but also for follow-up of lesions and search for healing problems such as fibrosis, muscle cysts, hernias, or myositis ossificans. High-frequency (13 MHz or higher) linear-array probes are used to perform musculoskeletal US examinations; only the deeper-located muscles and tendons are documented at a lower resolution leading to less sensitivity, e.g., hamstrings muscles and the deep flexor compartment of the lower leg in well-trained sports people with increased muscle mass. The highest accuracy of ultrasound is calculated 24–72 h after the muscle injury; this is related to the easy ultrasound detection of fully developed serosanguinous fluid collections (Fig. 2.2). Because of this drawback, ultrasound evaluation on the sports field is not indicated. Transverse and longitudinal evaluation is mandatory. Lesion detection is most accurate by transverse screening of the involved muscle compartments from origin to insertion. US palpation is a very valuable tool, trying to find the point of maximal tenderness during the examination by a gentle but firm compression of the probe on the skin (Peetrons 2002). Active and passive dynamic US study may be very helpful to the correct diagnosis, e.g., to search for muscle hernia (during muscle contraction), to discriminate grade II (partial) and grade III (complete) muscle or tendon tears, or to evaluate the anterior and lateral snapping hip syndrome (during hip flexion and lateral rotation). To avoid artifacts or pitfalls, comparison with the contralateral side may be necessary. The addition of color-power Doppler imaging to US has allowed for the noninvasive study of blood flow and vascularization within anatomic structures and angiogenesis in lesions (Fig. 2.3). The highest accuracy is reached in the evaluation of angiogenesis in superficial and relaxed structures with gentle probe manipulation. In patients with tendinosis, angiogenesis in the tendon may be correlated with clinical symptoms [Weinberg et al. 1998; Zanetti et al. 2003] and discriminates early (reactive) from advanced (dysrepair or degenerative) stages of tendinopathy (Cook and Purdam 2009). Furthermore, US provides image guidance for interventional procedures such as drainage of fluid collections and cysts (Peetrons 2002), percutaneous tenotomy, and platelet-rich plasma (PRP) injection in chronic tendinopathy. US-guided sclerosis of neovascularity in painful chronic tendinosis has been described as an effective treatment with significant reduction of pain during activity by Öhberg and Alfredson; their accuracy however is until now not reproduced by other centers; in a large RCT only moderate results were obtained with few of the patients cured; the majority still had reduced function and substantial pain after 24 months of follow-up (Öhberg and Alfrendson 2002; Hoksrud et al. 2012). The trade-off for high-frequency, linear, musculoskeletal transducers is their limited depth of penetration and the small, static scan field. This is a disadvantage if the structure to be visualized is large (e.g., large intramuscular hematoma) or deeply located (e.g., hip joint). Extended-field-of-view sonography (EFOVS) overcomes the disadvantage of a small static field by generating a panoramic image. With this technique, during longitudinal probe translation over the skin of the patient, sequential registration of images along a broad examination region and their subsequent combination into an image of larger dimension and format is obtained (Weng et al. 1997). EFOVS does not add much in diagnosis but is, however, easily interpretable by the novice and improves cross-specialty communication. For better evaluating deeply located structures, such as the hip joint, hamstrings, and deep posterior lower leg compartment in an obese or well-trained patient, other (cross-sectional) imaging modalities are often required. Other disadvantages of ultrasound include operator dependency, selective and often incomprehensible documentation, and the inability to penetrate osseous structures. Despite the latter, ultrasound is sensitive to rule out cortical fractures of superficially located bones and is more accurate to detect rib fractures compared to radiographs (Evans and Harris 2012).
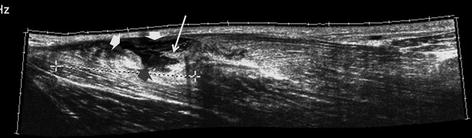
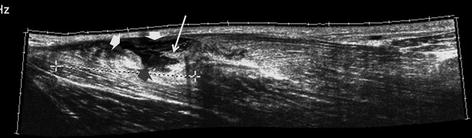
Fig. 2.2
Ultrasound of an adductor longus muscle tear. Longitudinal EFOVS of the proximal half of the right adductor longus in an adult soccer player after sudden snap during ball kicking. Examination performed 2 days after the injury. The EFOVS covers a length of 21 cm including the proximal MTJ and muscle belly of the adductor longus. Disruption of fiber discontinuity with distally retracted tendon (arrow) surrounded by a hyporeflective serosanguinous fluid collection with irregular margins (arrowheads). The hyporeflective fluid collection accentuates the structural anomaly of the muscle improving lesion conspicuity
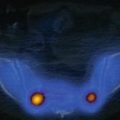
Fig. 2.3
Ultrasound of patellar tendinosis (jumper’s knee), advanced stage with angiogenesis. Sagittal US examination in 17-year-old female volleyball player with chronic pain at right the patellar apex. (a) Image with stretched quadriceps muscle, (b) image with relaxed quadriceps muscle and with gentle probe manipulation. Demonstration of thickening of the patellar tendon at its origin without obvious major structural anomalies and regular lining on the image with stretched quadriceps muscle. (a) Demonstrates no angiogenesis and (b) demonstrates major angiogenesis at the thickened area of the tendon and at the anterior cranial part of Kager’s fat plane
2.2.3 Multidetector Spiral CT Scan
2.2.3.1 Technique
CT imaging, by virtue of its excellent multiplanar capability and submillimeter spatial resolution due to the development of the spiral acquisition mode and current multidetector row technology, is a valuable imaging tool for the evaluation of all kinds of sports injuries (Berland and Smith 1998). Very fast image acquisition time of large volumes with submillimeter section thickness has become the norm. It has proved to be an effective method for documenting injuries particularly in complex bony structures such as the wrist and pelvis and may often show post-traumatic changes not shown by radiography. For most musculoskeletal studies, slice thickness is 0.75 mm, reconstructed to 1 mm images with increment of 0.5 mm. The images should be assessed using both bone and soft tissue window settings. From the three-dimensional data set, images can be reformatted in other planes (2-D technique) and be used for volume rendering (3-D technique). The 2-D reformatting of sagittal and coronal images from axial images can highlight longitudinal fracture lines and can make it easier to evaluate horizontal interfaces, such as the acetabular roof. The 3-D rendering allows different displays of the volume data. Surface rendering by thresholding, which, in contrast to volume rendering, incorporates only a portion of the data into the 3-D image, is the most widely used technique. By adding a virtual light source, a shaded surface display (SSD) can be achieved, which enhances the 3-D understanding of the image. However, it may provide an inadequate display of undisplaced and intra-articular fragments, and, in comparison to axial imaging, surface rendering does not increase the detection rate of fractures and should only be supplementary to plain films and axial CT scan in the evaluation of comminuted fractures. Volume rendering, incorporating all the data into the 3-D image, requires more computer manipulation. All reconstruction methods offer a more effective display of complex anatomic and pathologic structures. It may be helpful for the assessment of comminuted fractures, improving visualization of the fracture’s extent and location, shape and position of the fracture fragments, and the condition of articular surfaces (Bohndorf et al. 2001). New iterative CT reconstruction algorithms and cone beam computerized tomography (CBCT) techniques are developed to reduce radiation dose with similar or even increased image quality (see Sect. 2.3).
2.2.3.2 CT Arthrography
Intra-articular injection of iodinated contrast material mixed with 1 ml of a 0.1 % solution of epinephrine is performed under fluoroscopic or ultrasonographic observation (Newberg et al. 1985; Jacobson et al. 2012; Berkoff et al. 2012). The volume of contrast medium injected depends on which joint is studied: shoulder, 10–15 ml; wrist, 5 ml; hip, 10 ml; knee, 20 ml; and ankle, 6–12 ml. After injection of contrast material, patients are asked to perform full-range mobilization of the joint with weight bearing and walking a few steps if a joint of the lower limb is involved. Anteroposterior, lateral, and oblique views are routinely obtained to image the entire articular cavity. Subsequently, multidetector CT is performed. The major advantage of CT arthrography (CTA) for the assessment of the cartilage is the excellent conspicuity of focal morphologic cartilage lesions continuous with the articular surface of the cartilage that results from the high spatial resolution and the high attenuation difference between the cartilage substance and the joint contrast filling the lesion (Fig. 2.4). Vande Berg et al. (2002) found, in a study with spiral CTA of cadaver knees, a better correlation for grading articular surfaces between macroscopic examination and spiral CTA than with MR imaging. Other potential advantages of spiral CTA with respect to MR imaging are the short examination time, the availability at short notice (short waiting list), and the low sensitivity for and limited degree of imaging artifacts related to the presence of microscopic metallic debris which may hinder MR imaging studies. Limitations of CTA include its invasiveness, possible allergic reaction, use of ionizing radiation, and poor extra-articular soft tissue contrast resolution. Another major limitation of CTA imaging of the cartilage is its complete insensitivity to alterations of the deep layers of the cartilage.
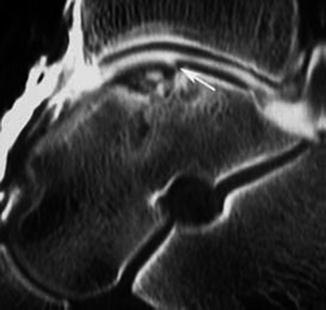
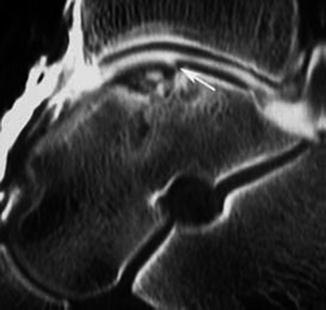
Fig. 2.4
CT arthrography of the ankle. 24-year-old soccer player with chronic ankle pain and history of repetitive ankle distortion. Radiographs demonstrate osteochondral lesion of the talus with in situ fragment (grade 3). CTA is performed to discriminate adherence of the fragment. Sagittal multiplanar reconstruction demonstrates the osteochondral defect with centrally located bone fragment; posterior to the fragment contrainfiltration is documented (arrow) that is not surrounding the fragment
2.2.4 Magnetic Resonance Imaging
Magnetic resonance imaging is the most complete radiological imaging technique with accurate evaluation of musculoskeletal soft tissues, bony structures, and joints. Its major indication in sports injury is internal derangement of joints, occult bone fractures, stress reaction and fracture of the bone, and deeply located muscle and tendon tears. Acute, subacute, and active chronic lesions are demonstrated with high conspicuity due to their increased water content that produces a “light bulb effect” on fat-suppressed sequences with long repetition time (TR); this sequence has become the cornerstone of musculoskeletal imaging. This light bulb is present in similar areas with high tracer uptake in bone scintigraphy and PET imaging. Specific MRI applications in the musculoskeletal system are addressed in the specific chapters.
2.2.4.1 Technique
Equipment and techniques for MRI vary widely, and although it is generally accepted that high-field-strength magnets provide the highest quality images, there has been considerable advancement in the technology of low-field-strength systems over the past few years, greatly improving their image quality. Open-bore gantry design is available in low- and midfield MRI and has specific musculoskeletal advantages related to off-center positioning and patient comfort with less claustrophobic renouncement. Absence of claustrophobia and low cost are the major advantages of low-cost extremity small-bore design (e-MRI); this is available at low field up to 1.5 T and used for investigation of the peripheral joints only (wrist, elbow, foot and ankle, and knee). Although appropriate selection of imaging planes will depend on the location and desired coverage of the anatomical region to be examined and the pathology to be expected, a complete MR examination of musculoskeletal regions requires that images be obtained or reconstructed in the axial, coronal, and sagittal planes. Of utmost importance is to respect the anatomical orthogonal planes since, with excessive rotation of a limb, inappropriate positioning of imaging planes may result in images which are difficult to interpret. Oblique planes may also be useful, e.g., in the hip in FAI (paracoronal and parasagittal images) and wrist in LT ligament disorders (paraxial images). The number of pulse sequences and combinations (“hybrid techniques”) is almost infinitive: in musculoskeletal MR, the most commonly used sequences include conventional spin echo (SE) for T1 weighting, turbo SE (TSE) sequences for intermediate or T2 weighting, and gradient echo (GRE) sequences. SE T1-WI is used for anatomic detail and as an adjunct in the evaluation of the osseous structures. TSE sequence has replaced conventional SE for T2 weighting (due to its relatively long acquisition times). However, because of image blurring, TSE sequences are not recommended for proton density imaging. Blurring can be reduced by increasing TE, decreasing the inter-echo time and echo train length (ETL), and increasing matrix. At higher field strengths (3 T), volume sequences are available with multiplanar reconstruction capacity at high resolution (0.5 mm) in all imaging planes. 3D-SPACE (sampling perfection with application-optimized contrasts using different flip-angle evolution) is recently pushing 2D TSE T2 or intermediate TE to the background (Fig. 2.5). TSE sequences are less susceptible to field inhomogeneity than SE sequences. Therefore, when metallic artifacts are present, such as in postsurgical patients, TSE sequences are preferred over SE and GRE. GRE sequences and TSE sequences with intermediate TE are used for the evaluation of articular cartilage. GRE sequences are used for dynamic contrast-enhanced imaging. They are also used in a limited number of T2 protocols (glenoid labrum, meniscus of the knee). When using short TE in T1-weighted or PD images, one should take the magic angle phenomenon into account, a source of false-positive MR findings. Furthermore, a pulse sequence is always a compromise between acquisition time, contrast, detail, or signal-to-noise ratio (SNR). SNR is highest in TSE and decreases respectively in SE and GRE sequences. Concerning the different fat-suppression (FS) techniques, in our institution, we prefer the spectral FS technique because of its better SNR and spatial resolution compared to inversion recovery fat-suppression techniques (Fleckenstein et al. 1991). Both T2-WI with (spectral) FS and STIR images are most sensitive to bone marrow and soft tissue edema or joint effusion. For good detection of fluid with preservation of anatomical detail and good differentiation between joint fluid and hyaline cartilage, we include an FS TSE intermediate-weighted sequence (TR/TE = 75/30–35 msec) in at least one imaging plane in our standard protocols. Cartilage-specific sequences have been developed (Disler et al. 2000; Ulbrich et al. 2013). The musculoskeletal system, especially in the extremities, is not influenced by motion, and as a consequence, motion artifacts are rare. Infolding artifacts can be avoided by selecting an appropriate imaging matrix, saturating anatomical areas outside the region of interest, and off-center imaging. Artifacts due to distortions of the local magnetic field are attributable to ferromagnetic and, to a lesser degree, nonferromagnetic orthopedic devices. The use of surface multichannel coils will improve the SNR; smaller slice thickness and larger matrices are essential for soft tissue imaging. The choice of small “field of view” (FOV) without changing the matrix size will increase the spatial resolution. Sometimes, imaging of the contralateral side may be useful, requiring a larger FOV and the use of a body coil. Contrast-enhanced MR studies lead to a prolonged examination time and high costs, and therefore, the use of intravenous contrast agents is not indicated when evaluating a sports lesion. It should be reserved for cases in which the results would influence patient care (Kransdorf and Murphey 2000). Application of intravenous gadolinium is indicated when dealing with a tumoral or pseudotumoral mass to detect neovascularization and intralesional necrosis (which is a major parameter for malignancy), in cases of inflammation or as part of indirect arthrography. For detection of subtle areas of contrast enhancement, we use subtraction images (SE T1-WI with FS after minus SE T1-WI with FS before gadolinium) (static MR imaging). After IV administration of gadolinium, STIR-type sequences should not be used, since not only fat but also enhancing tissue will be shown with a reduced signal intensity.