G-R hearing class
Criteria
Class I (good)
PTA 0–30dB and/or SDS 70–100 %
Class II (serviceable/useful)
PTA 31–50dB and/or SDS 50–69 %
Class III (non-serviceable)
PTA 51–90dB and/or SDS 5–49 %
Class IV (poor)
PTA 91dB-max and/or SDS 1–4 %
Class V (none/deaf)
Untestable for PTA and/or SDS
Facial weakness occurs less commonly from tumor growth or from iatrogenic (surgical or radiation) injury than hearing loss in acoustic schwannoma patients even though the nerves run side by side through the internal auditory canal. The House-Brackmann classification for facial weakness [5] (Table 23.2) was devised to grade postoperative facial weakness following acoustic schwannoma surgery. Fortunately the 15–20 % rates of developing any facial neuropathy (temporary plus permanent) reported in early radiosurgery series with higher doses of 16–18 Gy and less conformal treatment plans have dropped to significantly less than 1 % in modern series with lower doses of 12–13 Gy and better treatment planning. Transient facial spasms or twitching without persistent weakness may sometimes occur in acoustic schwannoma patients from facial nerve irritation. Chang et al. [6] reported a series of six patients with hemifacial spasm from cerebellopontine angle tumors (four meningiomas and two acoustic schwannomas) managed by radiosurgery. Four of 6 obtained complete relief and one patient partial relief of hemifacial spasm with accompanying tumor shrinkage. The sixth patient with no relief had no tumor shrinkage.
Grade 1 | Normal facial function in all regions |
Grade 2 | Mild dysfunction: light weakness not obvious at rest |
Grade 3 | Moderate weakness that is obvious at rest but not disfiguring and with complete eyelid closure |
Grade 4 | Moderate to severe weakness: obvious disfiguring weakness with incomplete eyelid closure |
Grade 5 | Severe weakness: barely perceptible muscle movement with incomplete eyelid closure |
Grade 6 | Complete paralysis, no movement, loss of tone |
New onset transient facial twitching has been observed in rare cases following acoustic schwannoma radiosurgery but seems to be a temporary response without any facial weakness developing.
As acoustic schwannomas continue to grow, they may compress the trigeminal nerve causing facial numbness, pain, and/or paresthesias. Tumor growth may also lead to brain stem compression and possibly obstructive hydrocephalus. The Koos classification (Table 23.3) is used to categorize acoustic schwannoma tumors according to size.
Table 23.3
Koos acoustic schwannoma tumor size grading criteria
Koos Grade I | Purely intracanalicular tumor limited to the internal auditory canal only |
Koos Grade II | < 2 cm extracanalicular/CPA extension without brainstem compression |
Koos Grade III | Extracanalicular/CPA extension >2 cm, with no brainstem compression |
Koos Grade IV | Extracanalicular/CPA extension with any degree of brainstem compression |
Management Options
Management options for acoustic schwannoma include observation, complete or partial resection, single fraction or multiple fraction radiosurgery (with 2–5 fractions) and fractionated radiotherapy (>5–30 fractions) with photons (X-rays or Co-60 gamma rays) or with protons. Surgical intervention is usually the preferred option for large acoustic tumors (particularly >4 cm) with no residual hearing in that ear and problems such as obstructive hydrocephalus.
Kondziolka’s literature review of acoustic schwannoma observation reported growth rates of 0–4 mm per year in different series with average volume doubling times of 1.65–4.4 years [7].
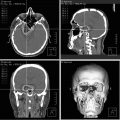
When observation is chosen as the management strategy, patients must stick to regular follow up audiometry and CT or MR scans at the same imaging center with comparisons of the newest to the oldest scans. As with any slow-growing tumor, slow but steady growth may sometimes be reported as no interval growth for several successive scans when only the two latest scans are compared by the radiologists, when comparison of the first to last scan identifies unmistakable growth. High resolution imaging with fine cuts (1–2 mm cuts) and software that allows volume calculation can be extremely useful for early identification of limited tumor growth. One technique for identifying tumor growth that can be useful at the time of radiosurgery in NF2 patients with multiple tumors (usually meningiomas and acoustic schwannomas) is image co-registration (fusion) of old and new scans with subtraction of the old images from the new images to highlight changes as shown in Fig. 23.1.


Fig. 23.1
Subtraction co-registration (fusion) T1-contrast enhanced MR images of a patient with bilateral acoustic tumors from NF-2 with 2009 images subtracted from 2011 images to highlight 2-year growth within the right sided tumor
Higher growth rates have been reported for younger patients and those with extracanalicular and cystic tumors. Observation of small acoustic schwannomas in NF2 patients with good hearing that appears to be stable may allow patients to enjoy more time with good hearing and give patients with tumors in their only hearing ear time to learn sign language before their hearing is lost. Initial observation may also be the best option for elderly patients with significant comorbidities and small tumors. Initial observation also is a good strategy for managing patients who want to delay treatment because of anxiety about any potential side effects from radiosurgery. A strategy of choosing to delay radiation treatment of an acoustic schwannoma until significant growth and/or hearing deterioration is documented exposes patients to the risks of hearing loss during the follow-up intervals as well as potentially higher hearing loss risk from irradiation of a larger tumor while initial radiation treatment has only the risk of hearing loss from treating the tumor at the time it is diagnosed. Kondziolka’s review of the medical literature on observation versus radiation treatment provides a detailed argument for early radiosurgical intervention [7].
Radiobiology of Tumor Control and Complications
Prior to the advent of radiosurgery, vestibular schwannomas were managed almost exclusively by observation or surgical resection because of a belief that they were radio-resistant, with the first article indicating effectiveness of radiotherapy in controlling acoustic schwannomas (following incomplete resection) published in 1987, following early reports of successful control with gamma knife radiosurgery [8].
Since then, multiple radiosurgery and radiotherapy series with long-term follow up demonstrated that vestibular schwannomas have control rates equal or better than other benign CNS tumors like WHO Grade-1 meningiomas and nonfunctional pituitary adenomas using similar or lower doses (in the range of 45–54 Gy at 1.8 Gy per fraction, 18–21 Gy in three fractions or 10–13 Gy in a single fraction).
Vernimmen and Slabbert calculated alpha-beta ratios of 2.4 and 1.8 Gy for control of acoustic schwannomas from published literature using the Fraction Equivalent plot (FE) and the Tucker methods, respectively [9]. Since the accepted alpha-beta values for late reacting CNS injury (cranial nerves, parenchymal brain injury or spinal cord) fall in the range of 1–2.5 Gy, these findings would support limited, if any, therapeutic gain from fractionation compared to single fraction treatment. In contrast to this radiobiological analysis, some centers report of better hearing preservation with fractionated radiotherapy as opposed to single fraction radiosurgery but all of these comparisons have difficulties. All CNS tissue does not seem to be equally likely to manifest clinically symptomatic radiation injury. Changes in function of somatic sensory nerves (optic and auditory) are detected a lower doses than somatic sensory nerves (trigeminal), while motor nerves (Cranial nerve 7, as well as 3, 4, 6, etc.) appear less likely to show radiation injury. Following radiation treatment of acoustic schwannomas (by radiotherapy or radiosurgery), hearing loss is the most frequent sequelae (30–60 % in most series) explained by the anatomy of the tumor and/or the sensitivity of the special sensory nerve, while the rates of trigeminal neuropathy (usually 1–4 %) exceed those of facial neuropathy (usually <1 %). The greater risks of trigeminal versus facial nerve injuries are observed even though a shorter segment of the trigeminal nerve is irradiated with generally lower doses than the facial nerve. Analysis of the initial experience of acoustic schwannoma radiosurgery at the University of Pittsburgh (including doses of 12–20 Gy) correlated rates of trigeminal and facial injury with dose and length of nerve irradiated [10].
Brainstem Tolerance
The parenchymal tissue in the brainstem tissue does not seem to be inherently more sensitive to radiation injury than other locations when assessed by the development of post-radiosurgery T2 signal changes, yet those changes are much more likely to result in neurological dysfunction than in other sites [11].
Nakaya et al. reported the University of Pittsburgh radiosurgery experience with 202 vestibular schwannomas and 44 meningiomas with brainstem compression after a median marginal dose of 13 Gy [12]. Median tumor volumes were 3.9 cm3 (range, 0.8–39.0 mL) and 6.6 mL (range, 1.6–25.1 mL) for acoustic schwannomas and meningiomas, respectively. No clear brainstem injury (with brainstem edema and/or enhancement) was identified with median follow-ups 65 and 60 months for the vestibular schwannomas and meningiomas, respectively. Although 13 Gy to the edge of the brainstem seems reasonably safe from this report, some contribution by radiation exposure to the nerve roots within the brainstem could not be ruled out to development of the 3.5 % and 9.9 % rates of facial and trigeminal neuropathies reported, respectively.
Adams et al. reported brainstem and cranial nerve injury developing after LINAC radiosurgery to a dose of 12 Gy prescribed to an 80 % isodose for treatment of an acoustic schwannoma measuring 27 × 19 × 18 mm [13]. Four months later she developed subjective right facial weakness and reduced taste on the right side of the tongue (seventh cranial nerve—CNVII) and by 8 months post-SRS, new right sided facial numbness and tingling (fifth cranial nerve—CNV). An MRI at 8 months showed reduction in tumor size to 20 × 16 × 14 mm with an adjacent area of enhancement (consistent with parenchymal radiation injury) of the right lateral pons/cerebellar peduncle which subsequently resolved. They performed a γ-H2AX focus formation assay which revealed impaired DNA damage kinetics in ex vivo-irradiated primary tissues which suggest that the radiosurgery patient had an inherent deficiency in double-stranded DNA breakage repair mechanisms.
Hearing Preservation and Cochlear Tolerance
Hearing preservation rates after acoustic schwannoma radiosurgery vary with prescription dose, length of follow up, tumor size, pretreatment hearing, and cochlear dose. Kano analyzed factors affecting hearing preservation in 77 acoustic schwannoma patients with Gardner-Robertson (GR) Grade 1–2 hearing who underwent gamma knife radiosurgery at the University of Pittsburgh with doses of 12–13 Gy between 2004 and 2007 [14]. He correlated hearing loss with Grade 1 hearing (versus Grade 2), age <60 years, and mean cochlear dose <4.2 Gy. 12/12 patients <60 years old with cochlear doses <4.2 Gy retained serviceable (Grade 1–2) hearing for 2 years or more. Although a single fraction cochlear dose of 4.2 Gy seems rather low to expect a correlation with hearing loss. Zuur et al. were able to identify modest decreases in hearing within 101 head and neck cancer patients undergoing 6–7 week courses of IMRT with median cochlear doses of only 11.4 Gy [15]. Yomo correlated hearing loss with a cochlear dose of 4 Gy or more in their series of 154 acoustic schwannoma patients undergoing gamma knife radiosurgery at Marseille [16]. Hasegawa et al. also correlated hearing loss with cochlear dose [17]. Although Kim et al., were unable to find a significant correlation between hearing loss and cochlear dose in their series of 66 unilateral acoustic schwannoma patients undergoing radiosurgery to a mean dose of 12 Gy, but did correlate hearing loss with transient post-radiosurgery volume expansion of ≥20 % from baseline [18].
While most cases of radiation injury to cranial nerves 5 and 7 usually show up within 2 or 3 years after radiosurgery, hearing decline following radiosurgery requires longer follow up.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree