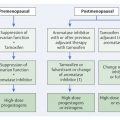
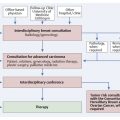
Radiotherapy of Breast Cancer For many decades now, radiotherapy has occupied a firm place in the multimodal treatment of carcinoma of the breast. It is an essential part of breast-conserving therapy, but it is also needed after mastectomy for advanced tumors. The use of radiotherapy leads to a substantial reduction of locoregional risk and to significant improvement in the long-term survival rate. These positive effects of radiotherapy cannot be achieved by the use of systemic therapeutic measures. In addition, modern radiotherapy methods have evolved dynamically such that significant acute reactions and late complications have become much rarer. As a result, the anticipated benefits of radiotherapy have, as a rule, clearly outstripped its potential risks. This is equally true for the primary treatment of very advanced and inoperable tumors 2 and the palliative treatment of symptomatic metastasis, especially in the skeletal system. As an integral component of what is always a multimodal treatment, the use of radiotherapy requires close interdisciplinary cooperation, especially with the gynecologist, the breast surgeon, and the internist/oncologist. Its organization for the benefit of the patients has significantly improved in the more recent years with the establishment of breast cancer centers. The essential aspects of radiotherapy of breast cancer are summarized in the respective current international guidelines for breast cancer 9, 15, including the most important references. Here the most important considerations are described, and additional current results are discussed and their practical uses clarified. Accordingly, the references presented here are limited to those aspects that go beyond the current guidelines. Breast-conserving surgery today is by far the predominant modality in the primary treatment of breast cancer—used in over 80% of the cases in designated breast cancer centers. This is always true for patients with early breast cancer. Even large primary tumors or involvement of an axillary lymph node do not constitute contraindications to breast-conserving surgery. In all these cases, adjuvant radiotherapy is an integral component of multimodal treatment. This also applies to most cases of ductal carcinoma in situ (DCIS). Earlier studies had already shown that, for most affected patients, a total mastectomy usually offers no advantage in comparison to breast-conserving surgery with subsequent radiation therapy. It is also applicable for younger patients with early breast cancer. 13 After its contribution to breast-conserving surgery, the most important effect of adjuvant radiotherapy is that the local recurrence rate is reduced by approximately one-third to one-fourth. Additionally, the tumor-related mortality also declines significantly in absolute terms by 3.3 to 8.5%, depending on risk factors with postoperative radiation therapy. 4 Similar improvements are also seen in the overall survival of affected patients, but manifested only after a period of at least 5 years (in contrast to the reduction of local recurrence rate) (▶ Table 13.1). 21 Thus, adjuvant radiotherapy after breast-conserving surgery has a similarly large long-term effect on tumor-specific and long-term survival as adjuvant systemic therapeutic measures. 20 Take Home Point Radiotherapy after Breast-Conserving Surgery In invasive carcinoma, the affected breast should be irradiated following breast-conserving surgery. The performance of a mastectomy in patients with breast cancer has substantially declined over the last few decades. In large centers today, it is carried out at most on only 20% of all affected patients, predominantly those in locoregionally advanced stages. Even in this situation, adjuvant percutaneous radiotherapy not only significantly improves the locoregional tumor control but improves the long-term survival rate as well (▶ Table 13.1). This also holds if additional effective systemic treatment is given, such as hormonal therapy and chemotherapy. 4, 21 The positive effect of adjuvant radiotherapy has been strengthened even further to the extent that, as part of an effective systemic therapy program, it can prevent systemic metastasis. 15 There have been further positive effects resulting from the continued improvement of radiotherapeutic modalities and techniques. Take Home Points Radiotherapy to the Chest Wall after Mastectomy Postsurgical radiotherapy to the chest wall after mastectomy decreases the risk of locoregional recurrence. In patients with high risk of local recurrence, the overall survival is also improved. Therefore, subsequent radiotherapy to the chest wall after mastectomy is indicated in the following situations: Tumor > 5 cm. Tumor < 5 cm only with the existence of other risk factors. R1/R2 resection with no possibility of a reexcision to clean up the margins. Axillary lymph node involvement. Overall, it may be assumed that, in patients with advanced locoregional tumors, the locoregional risk of relapse decreases to about one-fourth and that the long-term survival rate (after 5–10 years) shows an absolute increase of at least 5%. The more advanced the disease is at the time of diagnosis, the greater are these effects. Today it can be expected that the risk of locoregional recurrence is less than 8% (see ▶ Table 13.1). One indication for adjuvant radiotherapy following mastectomy is in patients with T3 tumors and/or positive axillary lymph nodes—especially if other unfavorable factors, such as invasion of lymph or blood vessels, are present (L1, V1), or if the primary tumor could not be completely surgically excised (R1, R2). In patients with T1/T2 tumors without axillary lymph node involvement in whom a mastectomy is performed instead of breast-conserving surgery, there is no sufficient advantage to be gained from adjuvant radiation therapy. However, all patients who undergo neoadjuvant chemotherapy and in whom a locoregional advanced carcinoma was diagnosed before this treatment, should undergo radiation therapy. In these patients, the indication is correspondingly oriented to the constellation of findings at the time the diagnosis is made. 15 Note If possible, the nodal status of a breast cancer should already be determined by sentinel lymph node biopsy before neoadjuvant chemotherapy is given. The positive effect of adjuvant radiotherapy is recognized in all age groups. However, a younger age, especially an age of less than 40 years, is the most important risk factor for local recurrence. Consequently, in this age group, the absolute benefit of adjuvant radiotherapy is of the greatest importance. Only in older patients with favorable prognostic risk factors and a limited life expectancy for other reasons, can adjuvant radiotherapy possibly be waived, and then only after extensive consultation with the patient. One must be explicitly warned of a therapeutic nihilism in this age group. Such behavior in the past has actually led to unjustifiably unfavorable results. 5 An important risk factor for local recurrence is a positive surgical margin after surgery. In the few cases with positive margins without the opportunity for a follow-up resection, the radiation therapist should consider a local increase in the radiation dose. Moreover, there is no doubt that systemic hormonal therapy, chemotherapy, and immunotherapy likewise contribute to a reduction of local recurrence. However, the positive effect of adjuvant radiotherapy on the local risk of recurrence and on long-term survival is sustained even after systemic therapy. 4, 21 There are other prognostic factors that have a confirmed influence on the tumor-specific mortality to some extent but have no importance in the indication for adjuvant radiation therapy. This is especially true for various molecular-genetic factors or gene-expression analyses, which are considered in making the choice of adjuvant medical treatment. Overall, current data indicate that—possibly with the exception of a subset of older patients with good prognostic factors and limited life expectancy—the withholding of adjuvant radiotherapy is associated with an approximately threefold higher risk of local recurrence in the affected breast and a significantly worsened survival rate. Correspondingly, all national and international guidelines include adjuvant radiotherapy as a standard part of the multimodal treatment scheme after breast-conserving surgery. 15 As a rule, when there is an indication for systemic chemotherapy, it is administered first, with the adjuvant radiotherapy being initiated about 3 to 4 weeks later. If there is merely an indication for adjuvant antiestrogen therapy, on the other hand, the adjuvant radiotherapy should be performed first and not later than 4 to 6 weeks after surgery. Because the use of tamoxifen before the course of radiotherapy could possibly increase the risk of side effects, it should preferably be started only after completion of the radiation therapy 23. On the other hand, treatment with trastuzumab can safely be continued, because this treatment represents an essential building block in the overall treatment of the high-risk patient (with positive HER2/neu status). 15 A reasonable definition of the target volumes, the overall dose, and the respective individual doses to be applied daily are of vital importance for the effectiveness and safety of the course of radiation therapy. Thus the clinical target volume (CTV) designates the regions in which residual tumor cells may be expected. The planning target volume (PTV), on the other hand, includes additional possible sources of spatial variability, such as movements of individual organs (some caused by breathing), and must take into account the technical aspects of optimal radiation therapy. For many years, adjuvant radiotherapy consisted of application to the entire chest wall on the affected side of 50 Gy, preferably homogeneously, with individual doses of 1.8 to 2.0 Gy over 5 to 6 weeks. After breast-conserving therapy, the entire affected mammary gland is included; the tumor bed receives a dose that is about 10 to 16 Gy higher (▶ Fig. 13.1, ▶ Fig. 13.2). As a rule, such a boost can be omitted after breast-conserving surgery in sano for DCIS, or after a mastectomy for locoregional advanced breast cancer. Fig. 13.1 Radiotherapy after breast-conserving surgery. The entire mammary gland is treated with 50 Gy and the tumor bed with 60 to 66 Gy. When positive axillary lymph nodes are found, the possibility of additional irradiation of the supraclavicular (SC), infraclavicular (IC), and lymph nodes of the internal mammary chain (IMC) of up to 45 Gy is discussed with the patient. In planning the radiation therapy, additional markings (arrows) are used that reliably ensure the correct positioning of the patient with the use of lasers. Fig. 13.2 Computer-aided planning (selected cross section) of radiotherapy to the tumor bed (red) and the remaining right mammary gland (green). Various colors signify different individual and cumulative doses for the various risk regions. Take Home Points Radiotherapy after Breast-conserving Surgery The target volume for the percutaneous radiotherapy should include the entire remaining breast and the adjacent chest wall. The dose should total approximately 50 Gy using conventional fractionation (5 × [1.8–2.0] Gy/week). A local radiation boost to the tumor bed decreases the local recurrence rate in the breast but does not confer a survival advantage. The boost radiation is usually indicated. The recommended boost dose amounts to 10 to 16 Gy with conventional fractionation. Whether and in what manner the regional lymphatic drainage should be part of the clinical target volumes has been a matter of debate for many years. Recent results of randomized trials (MA.20 and EORTC 22922/10925) have demonstrated that the addition of regional nodal irradiation to the internal mammary nodes and the supraclavicular region significantly improves outcome in patients, in whom the axillary lymph node was positive at initial diagnosis. 14, 29 In the MA.20 and EORTC trial, regional recurrences were reduced to 2.7% and 4.2% respectively with adjuvant breast irradiation only, to 0.7% and 2.7% respectively with the addition of nodal irradiation. Most importantly, the distant recurrences were significantly reduced from 17.3% and 19.6% respectively to 13.4% and 15.9% respectively at a median follow-up of more than 10 years. In addition, there was a corresponding improvement of disease-free survival. Interestingly, these positive aspects of additional nodal irradiation have been shown not only for patients with a least four positive lymph nodes but similarly for those with one to three affected lymph nodes 31, 29. Furthermore, fears that radiotherapy of the retrosternal lymph nodes could lead to a significant increase in cardiac mortality (especially when combined with anthracycline chemotherapy and treatment with trastuzumab) have not been confirmed to date. 19, 21 All of this advocates discussion with the patient, in whom at least one axillary lymph node has been found to be positive, about also giving radiotherapy for the ipsilateral supraclavicular and retrosternal lymph nodes also (see ▶ Fig. 13.1). As a result, the National Comprehensive Cancer Network (NCCN) panel strongly recommends additional irradiation of infraclavicular and supraclavicular areas and the internal mammary nodes in patients with positive axillary lymph nodes. In contrast, irradiation of the regional nodal area is generally not indicated for those with negative axillary nodes. 14 It is unknown at present whether special diagnostic measures, such as positron emission tomography (PET) combined with CT, or a representation of the lymph channels with scintigraphy, can contribute to a more targeted choice for radiotherapy of the retrosternal lymph nodes. 8, 27 Take Home Points Radiotherapy of the Regional Lymphatic Drainage Areas Radiotherapy should not be administered to the regional lymphatic drainage areas for stage pN0. Radiotherapy of the supraclavicular and infraclavicular lymph drainage channels and the internal mammary nodes is recommended in the case of positive lymph nodes. Radiotherapy should be considered for any part of the axilla at risk: Postoperative residual tumor in the axilla. Extensive tumor load in the axilla. Positive axillary nodes if only sentinel node has been removed (no lymph node dissection). 30 The utility of radiotherapy of the regional lymphatic drainage channels in cases of verified isolated tumor cells or of micrometastases in the regional lymph nodes has not been demonstrated, so that this should not be routinely carried out. There have been numerous attempts after breast-conserving surgery to replace percutaneous radiotherapy of the entire residual breast with partial breast irradiation. The main objective here was to further reduce the acute side effects and late sequelae and to shorten the treatment time through accelerated treatments, or even a single treatment. 14, 17, 32 Several methods were employed for this, including percutaneous irradiation with electron beams and a three-dimensional conformal or intensity-modulated technique (both with and without proton beams); most frequently, interstitial forms of therapy with multicatheter or balloon catheter techniques, or intraoperative techniques with electron beams or X-rays have been used. 25, 32 After the first limited experiences, the debate over partial breast irradiation was reignited by the release of the first results of the Targit A trial. 25 In this study, a total of 2,232 patients were randomized into a standard arm involving treatment exclusively with percutaneous radiotherapy of the breast, and an arm involving treatment with intraoperative radiation therapy. In the later treatment arm, 854 patients received exclusively intraoperative radiation therapy; only 142 received an additional percutaneous irradiation of the entire mammary gland. The intraoperative radiotherapy was carried out with conventional X-irradiation, which was delivered to the surgical area by means of a specially adapted applicator after tumor resection. The published 3-year follow-up data showed no significant difference with regard to local risk of recurrence to that point (approximately 1% in both arms of the study). The incidence of observed side effects of the therapy also did not differ significantly. 25 However, because the follow-up time for the exclusively intraoperative radiotherapy group is still very short, this method has to date only been approved as boost therapy in Germany, except for its use in medical studies. Further follow-up of the Targit trials and the performance of further studies (e.g., for patients over 70 years of age) will reveal more clearly which form of partial irradiation is particularly suitable for which indication area and whether this can replace the current standard methods. As this unfolds, questions about the local recurrence rate, the long-term overall survival rate, and possible late sequelae (in particular the cosmetic results) will be in the foreground. Previous experience shows that follow-up periods of at least 10 years need to pass before significant effects on the survival rate can be expected (see ▶ Table 13.1). Treatment Time after treatment (years) Locoregional recurrence (%) Mortality from breast cancer (%) All-cause mortality (%) Without RT With RT Without RT With RT Without RT With RT After breast-conserving surgery 5 25.9 7.3 11.4 10.1 12.9 11.9 10 32.0 10.3 24.8 20.7 27.7 24.5 15 35.9 30.5 40.5 35.2 After mastectomy (8,505 node-positive patients) 5 22.8 5.8 34.0 32.1 35.5 33.6 10 27.6 7.5 50.9 46.7 53.7 49.9 15 29.2 7.8 60.1 54.7 64.2 59.8
13.1 Adjuvant Radiotherapy after Breast-Conserving Surgery
13.2 Adjuvant Radiotherapy after Mastectomy
13.3 Effectiveness of Adjuvant Radiation Therapy: Prognostic Factors
13.4 Integration of Adjuvant Radiotherapy into the Multimodal Treatment Concept
13.5 Target Volume and Dose Concept
13.5.1 Clinical Target Volume: Former Tumor Region, Mammary Gland, Chest Wall, and Regional Lymph Channels


13.5.2 Partial Breast Irradiation
(7,311 patients, of which 17% were node-positive)
Radiology Key
Fastest Radiology Insight Engine