Presentation and Presenting Images
( ▶ Fig. 94.1, ▶ Fig. 94.2, ▶ Fig. 94.3, ▶ Fig. 94.4, ▶ Fig. 94.5, ▶ Fig. 94.6, ▶ Fig. 94.7, ▶ Fig. 94.8, ▶ Fig. 94.9)
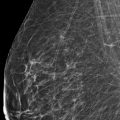
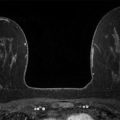
A 69-year-old female recently diagnosed with high-grade ductal carcinoma in situ (DCIS) of the right breast presents for diagnostic mammography and evaluation.
94.2 Key Images
( ▶ Fig. 94.10, ▶ Fig. 94.11, ▶ Fig. 94.12, ▶ Fig. 94.13, ▶ Fig. 94.14, ▶ Fig. 94.15, ▶ Fig. 94.16)
94.2.1 Breast Tissue Density
The breasts are heterogeneously dense, which may obscure small masses.
94.2.2 Imaging Findings
The imaging of the left breast is normal (not shown). The right breast demonstrates pleomorphic calcifications in a regional distribution with an associated postbiopsy clip and a high-density mass at the 10 to 11 o’clock location (circle in ▶ Fig. 94.10, ▶ Fig. 94.11, ▶ Fig. 94.12, ▶ Fig. 94.13, and ▶ Fig. 94.14). The high-density mass was not present on the prebiopsy mammogram ( ▶ Fig. 64.6 and ▶ Fig. 64.7) and is consistent with a postbiopsy hematoma. Digital breast tomosynthesis images clearly demonstrate the malignant calcifications, and the benign vascular calcifications are adjacent to the known malignancy (broken arrow; ▶ Fig. 94.15 and ▶ Fig. 94.16). The postbiopsy clip at the 8 o’clock location (short solid arrow in ▶ Fig. 94.10, ▶ Fig. 94.11, and ▶ Fig. 94.12) denotes the site of a prior benign biopsy. An abnormal lymph node (long solid arrow in ▶ Fig. 94.11) is noted in the right axilla.
94.3 BI-RADS Classification and Action
Category 6: Known biopsy-proven malignancy
94.4 Differential Diagnosis
Ductal carcinoma in situ (DCIS) and postbiopsy hematoma: DCIS may present as pleomorphic calcifications. The absence of the high-density mass on the prebiopsy mammogram makes this finding more consistent with a postbiopsy hematoma.
Ductal carcinoma in situ and invasive ductal carcinoma: Suspicious calcifications and a high-density mass are concerning for ductal carcinoma in situ and invasive ductal carcinoma. The absence of the high-density mass on the prebiopsy mammogram makes this mass more consistent with a postbiopsy hematoma than a malignant mass. Even excluding the mass as malignant, the abnormal axillary lymph node makes this a likely possibility.
Fat necrosis: Although fat necrosis has many appearances, the presence of the abnormal lymph node makes this an unlikely possibility.
94.5 Essential Facts
DBT is helpful in evaluating the distribution of both the suspicious calcifications and the benign vascular calcifications.
Comparison of the two-dimensional (2D) mammography and DBT images helped resolve that the density associated with the calcifications was a postbiopsy change and not an associated mass lesion.
Theoretically DCIS of the breast is considered a preinvasive and/or noninvasive lesion without potential for lymph node or distant metastases. Tan and colleagues (2007) found no risk factors that were predictive for sentinel lymph node biopsy; however, some authors believe that there is a subset of patients with DCIS who would benefit from sentinel lymph node biopsy.
Axillary metastases at sentinel lymph node sampling are uncommon in patients with DCIS, but have been reported in up to 15% of patients.
Most axillary metastases are likely due to occult invasive cancer in patients with high-grade or large volume DCIS. A small invasive cancer can go undetected at histopathologic diagnosis.
94.6 Management and Digital Breast Tomosynthesis Principles
Axillary views may be performed with DBT; however, the likely yield using DBT to evaluate axillary lymph nodes is low.
Although limited with respect to the inability to magnify calcifications, DBT can identify and localize calcifications.
If this finding were visualized only on DBT and biopsy needed to be performed, you would want to target away from the vascular calcifications.
94.7 Further Reading
[1] Boler DE, Cabioglu N, Ince U, Esen G, Uras C. Sentinel lymph node biopsy in pure DCIS: is it necessary? ISRN Surg. 2012; 2012: 394095PubMed
[2] Khakpour N, Zager JS, Yen T, et al. The role of ultrasound in the surgical management of patients diagnosed with ductal carcinoma in situ of the breast. Breast J. 2006; 12(3): 212‐215 PubMed
[3] Tan JCC, McCready DR, Easson AM, Leong WL. Role of sentinel lymph node biopsy in ductal carcinoma-in-situ treated by mastectomy. Ann Surg Oncol. 2007; 14(2): 638‐645 PubMed
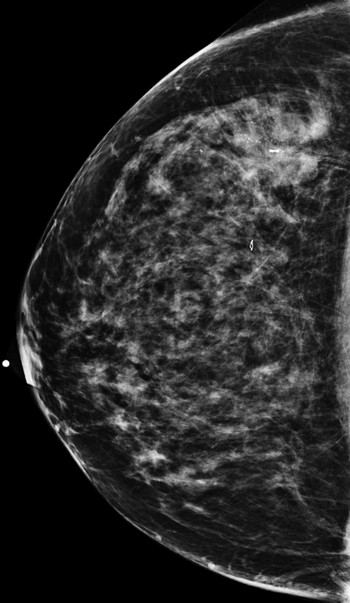
Fig. 94.1 Right craniocaudal (RCC) mammogram.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree