elements is more likely to result in misinterpretations and inaccurate, incoherent reports. Preferably, the room in which the report is dictated should be isolated from the clinical setting and in an area where the least amount of disturbance will occur, making it conducive to focused concentration. In addition, the room should have the capability for adequately decreasing external light sources.
Table 15-1 Fifteen-Year Cost Analysis: Film-Based X-Ray Versus Direct Radiography | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Table 15-2 Essentials of Plain-Film Musculoskeletal Reporting | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
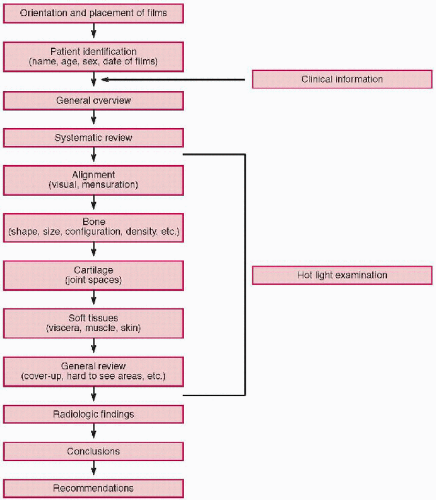
and other demographics. Then identify what projection each film represents. At this stage it is vital to assess each film for technical quality, including exposure, collimation, positioning, motion, phase of respiration, applied markers (erect, supine, right-left, etc.), and artifacts.
Table 15-3 Summary of Key Terms for Reporting Musculoskeletal Disease | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
disc spaces and the apophyseal, atlantoaxial, neurocentral, and costovertebral articulations. The peripheral joints are readily recognized. Each joint can be assessed for the depth of the joint space, the smooth articular bony cortex, and the bone density beneath the cortex (subchondral bone). The width of the joint cavity reflects the cartilage thickness, with only the small loose joints of the toes or fingers widening owing to effusion. Narrowing of the joint space reflects loss of the articular cartilage and is a sign of arthritis. The articular cortex is thin but is usually clear and sharp in its outline and smooth in contour. Loss of the joint cortex is a key sign of articular disease and may be the result of synovial proliferation, infection, or degenerative synovial cyst (geode). Thickening of the joint cortex can be seen with degenerative joint disease. When reporting about a joint, comments on these features should be made; for a normal joint a relevant statement would be “the joint space is preserved, the articular surfaces are smooth and congruent and of normal density” or “there is no joint abnormality.”
Review of hard-to-see areas. On any radiograph there are always details that are usually obscured and difficult to visualize because of anatomic superimposition or because of the projection. Therefore, if an abnormality is present in one of these obscured areas, it is likely to be overlooked without careful scrutiny. (23) This includes those portions of the film that are inherently overexposed or covered by another anatomic structure, such as the view box holding clip, positioning markers, identification plate, and any other obscuring artifact. (Table 15-4)
Hot (bright) light examination. No interpretation is complete without each radiograph being illuminated by the hot light. Examination by this method is especially useful in overexposed areas that are not normally rendered visible on the ordinary view box. In addition, by limiting the field of view, closer inspection of individual details is enhanced. (7,24)
Cover-up examination. This is a useful technique for larger-size radiographs, but it can also be applied to any film. The basic idea is to limit the field of view to a small area, inspect it, and move to another portion of the radiograph. The larger the surface area available to be inspected, the more anatomic details that must be examined. A simple way to reduce the observable area is to take a 45- by 37-cm (14- by 17-inch) film envelope, cover the entire film up, and slowly move the envelope down while observing the limited view of the film. In addition to limiting the field, the interpreter’s eyes are forced to compare one side with the other, carefully noting individual details. The combination of reduced visual field and augmented visual acuity makes this a useful review method.
Table 15-4 Hard-to-See Review Areas
Cervical spine
Skull base
Odontoid process
Neurocentral joints
Cervicothoracic junction
Prevertebral soft tissues
Trachea
Lung apices
Thoracic spine
Pedicles
Posterior ribs
Paravertebral lines
Posterior lung fields
Diaphragms
Posterior costophrenic sulcus
Costotransverse joints
Lumbar spine
Apophyseal joints
Pedicles
Pars interarticularis
Lung bases
Lower ribs and costal joints
Gas patterns
Psoas
Pelvis and hips
Acetabular floor
Iliac crest
Sacral foramina
Sacroiliac joints
Femoral head and neck
Knee
Patellofemoral joint
Intercondylar notch
Tibial eminences
Tibial tuberosity
Hoffa’s fat-pad
Ankle
Malleoli (3)
Talar dome
Anterior process of calcaneus
Cuneiforms, cuboid
Subtalar joint
Foot
Phalanges
Metatarsal heads
Hallux sesamoids
Shoulder
Lung apex
Greater tuberosity
Coracoid and acromion process
Elbow
Fat-pad positions
Radial tuberosity
Olecranon, coronoid fossae
Supinator fat line
Wrist
Scaphoid waist
Scapholunate interspace
Hook of the hamate
Ulnar variance
Triangular fibrocartilage
Metacarpotrapezial joint
Hand
Distal phalanx
Metacarpal heads
Other examinations. Many other methods have been proposed by individuals to enhance visual perception, most of which were “discovered” by personal experience. These methods range from scientific attempts to enhance eye physiology to simple cheating (discussed below). (18)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree