Fig. 1
a–b T1- and T2-weighted images show multiple hepatic masses throughout the liver, with a more confluent area of tumor within the inferior right hepatic lobe consistent with metastatic cholangiocarcinoma. These lesions demonstrate rim enhancement on c arterial phase
Fig. 2
A 73-year-old male diagnosed with cholangiocarcinoma. There is a heterogeneous mass of approximately 8 × 5.5 cm to the left of the falciform ligament involving the left and anterior right hepatic lobes. The left and middle hepatic veins are occluded. The mass demonstrates irregular borders predominantly hypointense in a T1- and b T2-weighted images. There is rim irregular enhancement of the mass after contrast administration in c arterial and d venous phases with presence
Fig. 3
a MRCP shows marked intrahepatic biliary dilatation or the right and left ducts (arrows); the pancreatic duct (PD) and the extrahepatic biliary duct (EHD) are normal. b Delayed contrast-enhanced image depicts an abrupt transition point at the porta hepatis showing a nodular area of enhancement (circle) due to a small tumor demonstrated by brushing
Cholangiocarcinoma is broadly classified into (1) extrahepatic and (2) intrahepatic cholangiocarcinoma (ICC).
3.1 Intrahepatic Cholangiocarcinoma
ICC is the second most common primary malignancy of the liver behind hepatocellular carcinoma (HCC). Based on the morphology and growth patterns, cholangiocarcinoma has been classified into three types: (1) mass-forming (2) intraductal-growing, and (3) periductal-infiltrating types [19].
Dynamic contrast-enhanced MR imaging findings in cholangiocarcinoma, in general, include early rim enhancement, characteristic delayed and persistent enhancement of the tumor. These findings reflect the characteristic fibrous content in the tumor and delayed diffusion of the contrast through the tumor interstitium [20]. On Gd-EOB-DTPA-enhanced MRI (Eovist), ICC presents as a hypointense lesion in delayed phase. Images in the hepatobiliary phase demonstrate highest lesion conspicuity with high contrast-to-noise ratio (CNR), and there will be no liver-specific contrast uptake since there will be negligible increase in SNR from late venous to hepatobiliary phases [21].
3.2 Intrahepatic Cholangiocarcinoma: Mass-Forming Type
Mass-forming cholangiocarcinoma presents as a homogenous mass with irregular, well-defined margins often associated with dilatation of the biliary trees in the periphery (Fig. 4). On MR imaging, the mass demonstrates irregular margins with high signal intensity on T2-weighted imaging and low signal intensity on T1-weighted imaging. On T2-weighted images, there may be a central hypointense area, which probably reflects severe fibrosis. On post-contrast MR images, there will be irregular peripheral enhancement with concentric filling of contrast material [22]. Significant central enhancement can be seen in delayed phase MR imaging, and this may be, again, due to the fibrous stroma of the tumor. Atypical presentations such as homogenous hypervascular enhancement, strong hyperintensity, and centripetal enhancement on T2-weighted MR images can be seen in mucinous carcinoma, but it presents with continuous ragged rim enhancement, which can help differentiate it from a hemangioma.
Fig. 4
a T1-weighted and b T2-weighted images demonstrate atrophy of the left hepatic lobe (LHL) with intrahepatic biliary dilatation (*). The biliary dilatation terminates at the level of an enhancing mass (arrows) in the left lobe as shown in the arterial c and venous phases d consistent with cholangiocarcinoma
3.3 Intrahepatic Cholangiocarcinoma: Periductal-Infiltrating Type
Periductal-infiltrating type of cholangiocarcinoma usually presents as a growth along a dilated or narrowed bile duct without mass formation and as an elongated or branchlike abnormality. Early diagnosis of periductal-infiltrating type of cholangiocarcinoma may be difficult since it may appear to be a benign looking stricture in the early stages. It is important to differentiate a benign from a malignant stricture and findings such as stricture with an irregular margin, asymmetric narrowing, lymph node enlargement, enhancing ducts, and periductal soft tissue lesion should raise strong suspicion for a malignant stricture [6]. On MR imaging, periductal-infiltrating type of cholangiocarcinoma presents with diffuse periductal thickening and increased enhancement due to tumor infiltration with abnormally dilated or irregularly narrowed duct and peripheral ductal dilatation [23] (Figs. 5 and 6).
Fig. 5
There is a hypointense ill-defined 9.4 × 6.2 cm mass within the left hepatic lobe associated with atrophy of the left hepatic lobe. After contrast administration, there is heterogeneously rim enhancement in a portal and b delayed phases. c MRCP shows intrahepatic biliary ductal dilatation in the right and left hepatic lobes
Fig. 6
A 66-year-old female diagnosed with intrahepatic cholangiocarcinoma. There is a large heterogeneously infiltrating mass involving the right and left hepatic lobes. a–c after contrast administration enhanced images showed peripheral enhancement (arrows) and central hypointense region probably associated with necrosis (+)
3.4 Intrahepatic Cholangiocarcinoma: Intraductal-Growing Type
Intraductal-growing-type cholangiocarcinoma has a significantly better prognosis than mass-forming-type or periductal-infiltrating-type cholangiocarcinoma (Fig. 7). MR imaging features suggestive of intraductal-growing-type cholangiocarcinoma include (1) papillary or irregular polypoid shape, (2) lack of constriction of the tumor-bearing segment, (3) hypoenhancement of the tumor to the liver during the equilibrium phase, (4) tumor multiplicity, (5) upstream and downstream bile duct dilatation, and (6) no bile duct wall thickening adjacent to the tumor. Kim et al. suggested that the presence of at least two of these six imaging features, when used in combination, has a sensitivity and specificity in the diagnosis intraductal-growing-type cholangiocarcinoma of 95 and 70 %, respectively. Intraductal-growing-type cholangiocarcinoma has a tendency to spread superficially along the mucosal surface, resulting in multiplication. Intraductal-growing-type cholangiocarcinoma more often showed washout, whereas mass-forming cholangiocarcinoma more often showed gradual persistent or progressive enhancement, which will help in differentiating between the two [24] (Figs. 8 and 9).
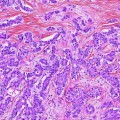
Fig. 7
A 73-year-old female with history of metastatic cholangiocarcinoma. a T1 image shows a dark infiltrative mass with irregular border on the right hepatic lobe. On b T2-weighted image, the mass looks heterogeneously hyperintense. After contrast administration, c portal and d delayed images showed peripheral enhancement. The mass appears contiguous with the gallbladder fundus with associated thickening of the fundus (arrows) and gallbladder stones
Fig. 8
Shrinkage of left hepatic lobe is noticed. a T1-weighted image shows a hypointense mass (M), which nearly replaces the entire left lobe of the liver, and it measures 8 × 7 cm. There is mild intrahepatic biliary duct dilatation (arrows). After contrast administration (c–e), there is late and heterogeneously enhancement of the mass. There is ascites seen in abdomen (*)
3.5 Extrahepatic Cholangiocarcinoma
Extrahepatic cholangiocarcinoma arises from the ductal epithelium of the extrahepatic bile duct. The most important factors in evaluating patients with extrahepatic cholangiocarcinoma are to determine tumor location and its longitudinal extent since these factors have greatest influence on surgical method and survival [13]. MRI is one of the most important diagnostic imaging modalities of choice used in assessing the longitudinal and lateral spread of a tumor when determining resectability. Perihilar cholangiocarcinomas have been categorized into four types by the modified Bismuth–Corlette classification adapted from the original classification [25]. On MR imaging, the enhancement pattern of extrahepatic cholangiocarcinomas is similar to that of ICCs. The tumors are hypovascular and enhance slowly and gradually to a peak on delayed imaging. These tumors are less heterogeneous than ICC since they present as small infiltrating tumors. Satellite nodules and central scars are unusual compared to ICC. Extrahepatic cholangiocarcinoma typically presents as abnormal circumferential extrahepatic bile duct wall thickening and enhancement best visualized 1–5 min after gadolinium administration [26].
On diffusion-weighted imaging, extrahepatic cholangiocarcinoma demonstrates differential levels of high signal intensity and low signal intensity in apparent diffusion coefficient maps and has great sensitivity in detection of extrahepatic cholangiocarcinoma comparable to MRCP [27].
3.6 Hilar Cholangiocarcinoma/Klatskin Tumors
Hilar cholangiocarcinoma, also known as Klatskin tumors, are adenocarcinomas that arise at the confluence of the right and the left hepatic bile ducts. MRI and MRCP can provide accurate preoperative staging of biliary tree, liver, and vascular involvement, and this is crucial in choosing the most appropriate treatment option in patients with cholangiocarcinoma.
Hilar cholangiocarcinoma demonstrates circumferential growth and spreads along the bile ducts with poor conspicuity on non-contrast MR images [28]. Hilar cholangiocarcinoma presents with the same signal intensity as peripheral tumors on both T1- and T2-weighted images. On post-contrast images, hilar cholangiocarcinomas do not always show a unique enhancement pattern. Most of the lesions are hypovascular compared to the adjacent liver parenchyma, with a heterogeneous enhancement that gradually peaks on delayed phase images, which is due to the fibrous nature of the tumor [29]. Some lesions show periductal enhancement, whereas very few hilar cholangiocarcinoma are hypervascular, but they do not demonstrate immediate diffuse enhancement unlike other hypervascular lesions.
3.7 Mixed Hepatocellular carcinoma–Cholangiocarcinoma
Mixed hepatocellular carcinoma–cholangiocarcinoma (HCC-CC) contributes to a small but significant proportion of primary liver malignancies, and they are comprised of cells with histopathological features of both cholangiocarcinoma and HCC [30].
On MRI, mixed hepatocellular carcinoma–cholangiocarcinoma usually presents with a single mass, moderately high signal intensity on T2, tumor demonstrating progressive enhancement or contrast retention, and frequent lack of capsule. Enhancement patterns include early rim enhancement and diffuse heterogeneous enhancement [31]. Hwang et al. demonstrated that on Gadoxetic acid-enhanced MRI, irregular shape, strong rim enhancement during early dynamic phase MRI, and absence of target appearance on hepatobiliary phase were more suggestive of hepatocellular carcinoma–cholangiocarcinoma (HCC-CC), whereas the findings of a lobulated shape, weak peripheral rim enhancement, and presence of complete target appearance on the hepatobiliary phase were more of suggestive ICC [32].
Differential Diagnosis:
Variety of neoplastic and non-neoplastic conditions can mimic the findings of cholangiocarcinoma and, thus, poses significant challenges in the diagnosis and management of these patients.
Neoplastic Conditions:
A tumors that should be considered in the differential diagnosis of cholangiocarcinoma includes HCCs. Patients where clinical background of cirrhosis, hepatitis B/C positive serology, and/or high levels of alpha feto protein (AFP) should alert toward the suspicion of HCC. According to the American Association for the Study of Liver Diseases (AASLD), diagnosis of HCC is to be considered in a mass larger than 2 cm with typical features of hypervascularity in the arterial phase and washout in the venous phase on a contrast-enhanced computed tomography or magnetic resonance (MR) imaging. A mass measures 1–2 cm is also considered suspicious for HCC if it shows these features at both CT and MRI. Park et al. demonstrated that a target appearance, with central enhancement and a hypointense rim on diffusion-weighted imaging (DWI), proved to be a reliable imaging marker indistinguishing small mass-forming an ICC from a small HCC [33].
Other neoplastic conditions to be considered in the differential diagnosis include intrabiliary metastases. Although rare, if suspected, metastasis from colonic adenocarcinoma tops the list since it shows increased predilection for biliary ducts [34]. Biliary tract melanoma can either be a primary melanoma arising from the biliary epithelium or metastasis from elsewhere. Owing to its own melanin content, this mass may demonstrate high signal intensity on T1-weighted images and low signal intensity on T2-weighted images [35]. Lymphoma of the bile ducts is very rare and usually a secondary manifestation of systemic disease. Most biliary lymphomas are non-Hodgkin’s lymphomas. Carcinoid tumors of the bile ducts are rare and account for less than 2 % of gastrointestinal carcinoid tumors. Imaging findings vary and are non-specific, including biliary strictures with associated wall thickening or a large exophytic mass, thus mimicking the periductal-infiltrating or mass-forming types of cholangiocarcinoma.
Non-neoplastic Conditions:
Various conditions that mimic cholangiocarcinoma on imaging include primary and secondary sclerosing cholangitis (SSC) and Mirizzi syndrome. MR cholangiopancreatography (MRCP) is considered the best initial approach in the diagnosis of primary sclerosing cholangitis (PSC) and characteristic imaging findings suggestive of PSC include multifocal strictures, irregular beading of the intra- and extrahepatic bile ducts, segmental ectasia, and ductal wall thickening [36]. SSC represents various disorders that are similar to PSC resulting from distinct pathologic process and include recurrent pyogenic cholangitis, which presents in the setting of biliary obstruction by stones or biliary strictures with recurrent episodes of acute pyogenic cholangitis and usually affects the extrahepatic duct, lateral segment of the left lobe, and posterior segment of the right lobe. MR imaging findings characteristic of recurrent pyogenic cholangitis include biliary strictures, intraductal pigmented stones, and ductal wall thickening due to fibrosis [37]. Mirizzi syndrome occurs due to the obstruction of the common hepatic duct due to compression by a gallstone impacted at the gallbladder neck or cystic duct, and it is considered that a low insertion of the cystic duct into the common hepatic duct is a predisposing factor for Mirizzi syndrome [38]. MRCP is a useful imaging modality in detecting gall stones and bile duct stenosis. Although imaging findings may not be specific, MRCP imaging findings suggestive of Mirizzi syndrome include presence of gallstone in the cystic duct, extrinsic narrowing of the common hepatic duct, dilatation of the intrahepatic and common hepatic ducts, and a normal common bile duct. In some cases, there will be strictures secondary to inflammation around the common bile duct and, thus, can resemble cholangiocarcinoma of the periductal-infiltrating type [39].
Another condition that resembles periductal-infiltrating-type cholangiocarcinoma is autoimmune pancreatitis–cholangitis. It presents with focal or diffuse strictures of the pancreatic ducts and the bile ducts. Narrowing of the intrapancreatic bile duct and bile duct strictures with upstream ductal dilatation can be seen resembling the periductal-infiltrating-type cholangiocarcinoma on MRI. The presence of pancreatic abnormalities, which include focal/diffuse/sausage-shaped diffuse enlargement of the pancreas with a peripheral hypoattenuating halo, should favor the diagnosis of autoimmune pancreatitis [40].
MRCP has been demonstrated to be a useful noninvasive imaging modality comparable to ERCP in differentiating extrahepatic bile duct cholangiocarcinoma from benign stricture. Based on cholangiographic criteria described by Park et al. [6] for malignant biliary strictures, irregular margins, and asymmetric narrowing were more commonly found in cholangiocarcinomas than in biliary strictures.
4 Periampullary Tumors
Periampullary tumors are neoplasms that arise within 2 cm of the major duodenal papilla and include pancreatic head carcinoma, intrapancreatic bile duct carcinoma, and periampullary duodenal carcinoma. While they share an anatomic location and clinical presentation, each malignancy has a different prevalence and outcome. While obstructive jaundice is the most common clinical symptom, the major changes seen on cross-sectional imaging are pancreaticobiliary duct dilatation, double duct sign, three-segment sign, four-segment sign, and shape and wall thickness of the distal margins of the common bile duct and the main pancreatic duct [41–43]. Periampullary tumors appear as low signal intensity masses in the region of the ampulla on T1-weighted fat-suppressed MRI. Most lesions are hypovascular with low signal intensity relative to adjacent normal tissue on contrast-enhanced T1-weighted images; however, a thin rim of peripheral enhancement can often be found on these fat-suppressed images. MRCP helps determine the precise location and organ of origin of these tumors. MR imaging can not only be used to differentiate these lesions, but also to assess resectability [44].
5 Ampullary Carcinoma
Ampullary carcinoma is often considered part of the group of periampullary tumors. They are small tumors arising in the ampulla of Vater that often cause biliary outflow obstruction. Diagnosis can be difficult because these small tumors mimic the appearance of benign causes of biliary outflow obstruction such as papillitis, papillary stenosis, and sphincter of Oddi dysfunction [41, 45–47




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree